Links between the central nervous system and the trillions of microorganisms in the human gut have been a major focus of research and public interest.Credit: Steve Gschmeissner/SPL
Just ten years ago, the idea that microorganisms in the human gut could influence the brain was often dismissed as wild. Not any more.
Links between the central nervous system and the trillions of bacteria in the gut — the microbiota — are now a major focus of research, public interest and press coverage. But how does this ‘gut–brain axis’ work? The mechanisms by which microorganisms shape aspects of brain functioning such as memory and social behaviour, and how they might contribute to conditions such as depression and neurodegenerative disease, are tenuous and often controversial.
Much of what we know so far is based on studies showing correlations between specific gut bacteria, their metabolites and neurological symptoms. But these correlations do not prove cause and effect. Many studies use animal models, which don’t accurately mirror human traits or behaviours. Human studies have been limited: they’re usually based on relatively small numbers of people, and might not control for a wealth of confounding factors — such as unusual diets, antibiotics or antidepressants — that can affect the microbiota.
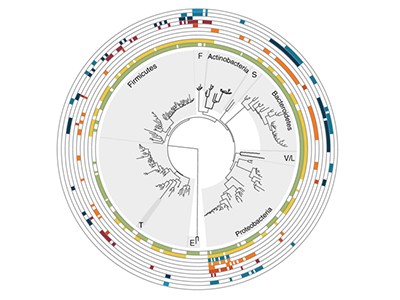
A study published this week in Nature Microbiology tackles some of these issues (M. Valles-Colomer et al. Nature Microbiol. https://doi.org/10.1038/s41564-018-0337-x; 2019). The authors used DNA sequencing to analyse microbiota in the faeces of more than 1,000 people enrolled in Belgium’s Flemish Gut Flora Project. The team then correlated different microbial taxa with the participants’ quality of life and incidence of depression, using self-reported and physician-supplied diagnoses. The researchers validated the findings in an independent cohort of 1,063 individuals in the Netherlands’ LifeLines DEEP project. Finally, they mined the data to generate a catalogue describing the microbiota’s capacity to produce or degrade molecules that can interact with the human nervous system.
The researchers found that two groups of bacteria, Coprococcus and Dialister, were reduced in people with depression. And they saw a positive correlation between quality of life and the potential ability of the gut microbiome to synthesize a breakdown product of the neurotransmitter dopamine, called 3,4-dihydroxyphenylacetic acid. The results are some of the strongest yet to show that a person’s microbiota can influence their mental health.
These are still correlations, not causes. Researchers know that the gut microbiota can produce or stimulate the production of neurotransmitters and neuroactive compounds, such as serotonin, GABA and dopamine, and that these compounds can modulate bacterial growth. The challenge now is to find out whether, and how, these microbe-derived molecules can interact with the human central nervous system, and whether that alters a person’s behaviour or risk of disease. At least now, answering these questions is a wise pursuit, not a wild one.

 Read the paper: The neuroactive potential of the human gut microbiota in quality of life and depression
Read the paper: The neuroactive potential of the human gut microbiota in quality of life and depression
 Why does the microbiome affect behaviour?
Why does the microbiome affect behaviour?
 The tantalizing links between gut microbes and the brain
The tantalizing links between gut microbes and the brain
 Action on mental health needs global cooperation
Action on mental health needs global cooperation