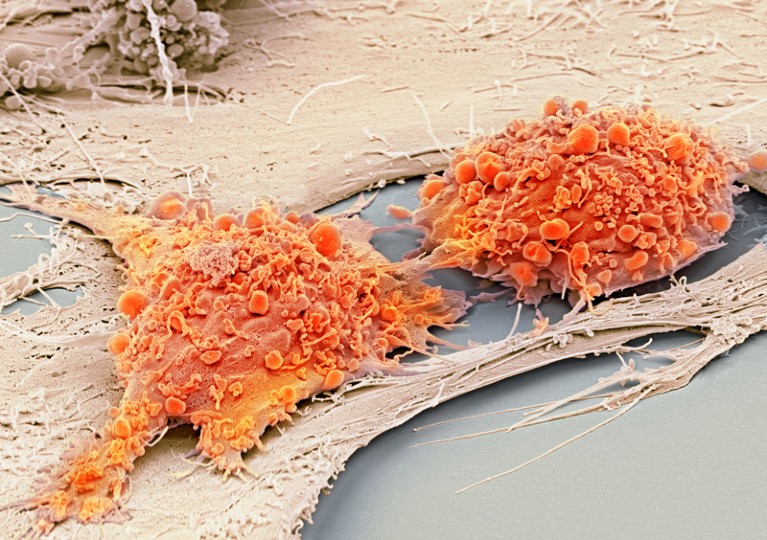
Japan is taking another unwise step to commercialize unproven stem-cell therapies.Credit: Steve Gschmeissner/SPL
Healing spinal-cord injuries has been one of the most difficult — and doggedly pursued — quests in medicine, and among the most symbolic goals for the field of stem cells and regenerative medicine.
Progress, however, has been frustratingly slow. Dozens of seemingly promising efforts, based on animal studies, have fallen flat.
Last week, a Californian company called Asterias Biotherapeutics released promising results from a 12-month first phase clinical trial, in which embryonic stem cells are converted into oligodendrocytes — cells of the central nervous system that support neurons and can stimulate their growth — and then injected into the backs of people with a spinal-cord injury. The data show that injected cells do stick around at the injury site, and that most patients (21 out of 22) showed improved movement.
But these are still early-stage results. It is not clear yet whether the improvements are the result of the cells, or whether something else, such as the body’s own regenerative capacity, was at work. To find out, the company wants permission to move forward with a randomized, controlled phase II clinical trial. That’s the right way to do things: stepping carefully, slowly and rigorously forward.
Japan’s approval of stem-cell treatment for spinal-cord injury concerns scientists
Meanwhile, in Japan, a more worrisome approach is unfolding. Last month, researchers at Sapporo Medical University leapfrogged all other spinal-cord injury treatments that use stem cells — including the one being investigated by Asterias — and received market approval for injections of a type of cell called a mesenchymal stem cell. There are reasons to be sceptical, or at least to delay the sale of this procedure to patients.
The very nature of these cells — in particular, whether they function as stem cells and do turn into neurons as suggested by the Japanese group — is subject to fierce debate (D. Sipp et al. Nature 561, 455–457; 2018). The clinical trials that demonstrated efficacy were based on only 13 participants. There was no control group and the trial data remain unpublished.
Through a fast-track process for regenerative medicine, launched in 2014 to speed treatments to patients and spur innovation, the Japanese government gave the mesenchymal stem-cell treatment, called Stemirac, ‘conditional approval’ to enter the market. It can be sold to patients, and the company was given seven years to show that it works. How that evidence will be collected once the treatment is on the market is an unanswered question.
A better way would have been to run a randomized controlled clinical trial, with both participants and physicians unaware of who received the cells and who received a placebo. But under Japan’s fast-track system, researchers at the university didn’t have to do this. The researchers also should have published the clinical data already collected, but in Japan they are discouraged from doing so.
This seems surprising. Some companies might not want to publish clinical results to protect their trade secrets. But in this case, it is Japan’s health ministry that seems to be telling researchers not to publish data. Although it is not a blanket ban — the propriety of publishing such data is evaluated on a case-by-case basis — a ministry representative told Nature that in this instance it would be discouraged. That’s because published data could be used as “promotional materials” and unduly influence patients or officials, according to the health ministry official.
Japan has set up a bizarre situation. The university has made promises about the treatment in an advertisement unencumbered by data, but the inclusion of scientific evidence, in a form that the world’s experts can evaluate, is considered too potentially misleading to publish. The Kafkaesque logic at play here seems to be that promoting a medicine without data is better than promoting it with.
The Japanese team has promised results so dramatically convincing that controlled trials would be unnecessary. Let’s hope that is the case. But it is more likely that ambiguous results from the uncontrolled trial will allow the treatment to continue in use indefinitely. That is fair neither to the patients who are willing to try the treatment, nor to other companies that are putting therapies through truly rigorous trials.
Japan could and should introduce a better and more transparent system, one that requires the production of sound clinical efficacy data through controlled trials, when possible, and that encourages broad evaluation of those data — in scientific publications, when feasible — by the international medical research community. Japan could, in other words, learn a lot from the way it’s being done in California. Until then, offering people such stem-cell treatments is premature and unfair.

 Japan’s approval of stem-cell treatment for spinal-cord injury concerns scientists
Japan’s approval of stem-cell treatment for spinal-cord injury concerns scientists
 Stem-cell tests must show success
Stem-cell tests must show success