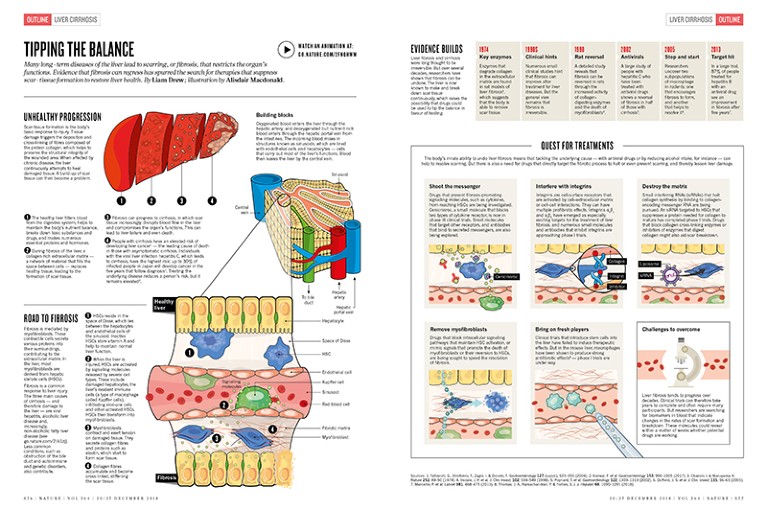
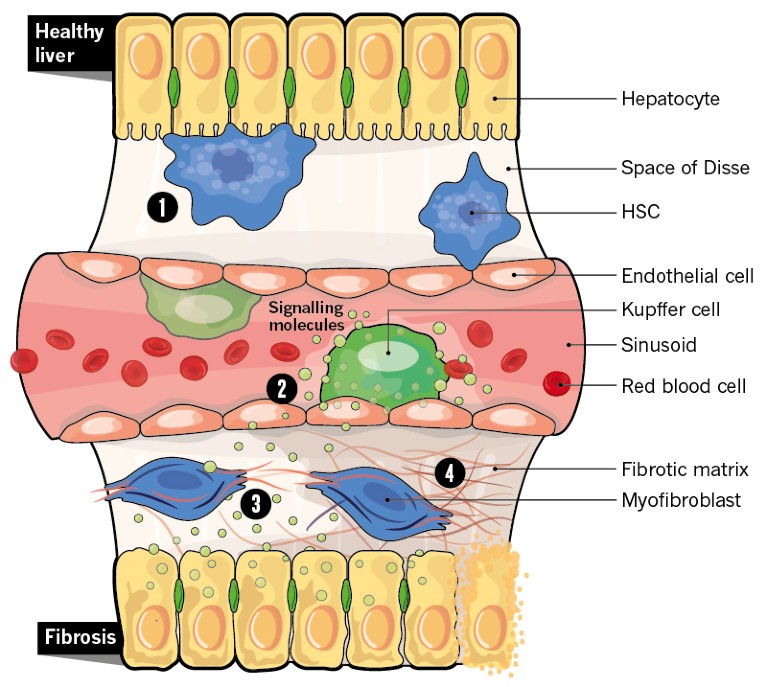
Unhealthy progression
Scar-tissue formation is the body’s basic response to injury. Tissue damage triggers the deposition and cross-linking of fibres composed of the protein collagen, which helps to preserve the structural integrity of the wounded area. When affected by chronic disease, the liver continuously attempts to heal damaged tissue. A build-up of scar tissue can then become a problem.
Credit: Alisdair Macdonald
1. The healthy liver filters blood from the digestive system, helps to maintain the body’s nutrient balance, breaks down toxic substances and drugs, and makes numerous essential proteins and hormones.
2. During fibrosis of the liver, a collagen-rich extracellular matrix — a network of material that fills the space between cells — replaces healthy tissue, leading to the formation of scar tissue.
3. Fibrosis can progress to cirrhosis, in which scar tissue increasingly disrupts blood flow in the liver and compromises the organ’s functions. This can lead to liver failure and even death.
4. People with cirrhosis have an elevated risk of developing liver cancer1 — the leading cause of death in those with asymptomatic cirrhosis. Individuals with the viral liver infection hepatitis C, which leads to cirrhosis, have the highest risk: up to 30% of infected people in Japan will develop cancer in the five years that follow diagnosis1. Treating the underlying disease reduces a person’s risk, but it remains elevated2.
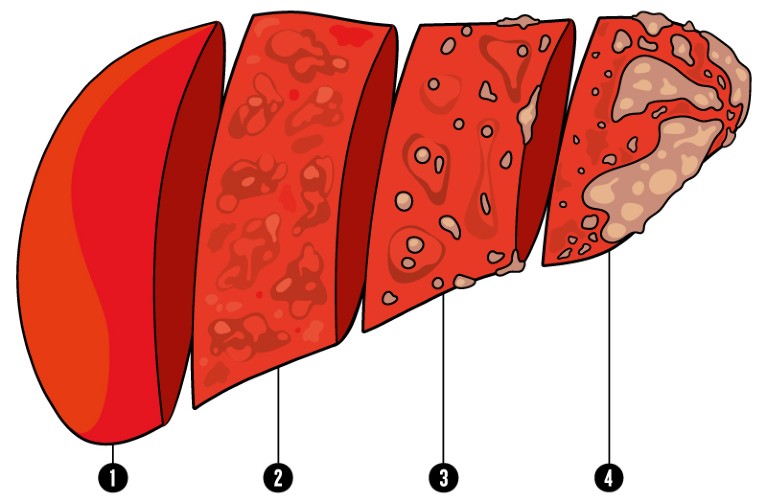
Building blocks
Credit: Alisdair Macdonald
Oxygenated blood enters the liver through the hepatic artery, and deoxygenated but nutrient-rich blood enters through the hepatic portal vein from the intestines. The incoming blood mixes in structures known as sinusoids, which are lined with endothelial cells and hepatocytes — cells that carry out most of the liver’s functions. Blood then leaves the liver by the central vein.
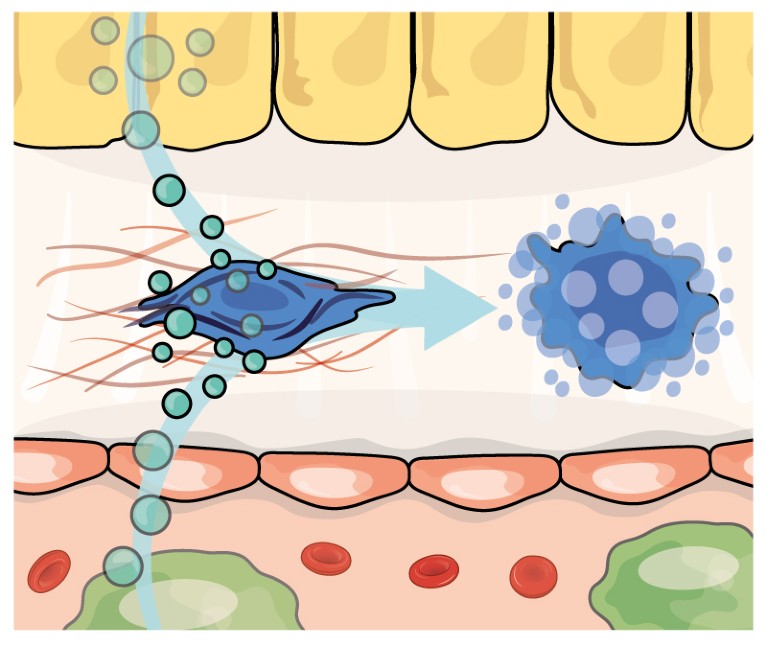
Road to fibrosis
Fibrosis is mediated by myofibroblasts. These contractile cells secrete various proteins into their surroundings, contributing to the extracellular matrix. In the liver, most myofibroblasts are derived from hepatic stellate cells (HSCs). Fibrosis is a common response to liver injury. The three main causes of cirrhosis — and therefore damage to the liver — are viral hepatitis, alcoholic liver disease and, increasingly, non-alcoholic fatty liver disease (see go.nature.com/2ilk1zj). Less common conditions, such as obstruction of the bile duct and autoimmune and genetic disorders, also contribute.
Credit: Alisdair Macdonald
1. HSCs reside in the space of Disse, which lies between the hepatocytes and endothelial cells of the sinusoid. Inactive HSCs store vitamin A and help to maintain normal liver function.
2. When the liver is injured, HSCs are activated by signalling molecules released by several cell types. These include damaged hepatocytes, the liver’s resident immune cells (a type of macrophage called Kupffer cells), infiltrating immune cells and other activated HSCs. HSCs then transform into myofibroblasts.
3. Myofibroblasts contract and exert tension on damaged tissue. They secrete collagen fibres and proteins such as elastin, which start to form scar tissue.
4. Collagen fibres accumulate and become cross-linked, stiffening the scar tissue.
Quest for treatments
The body’s innate ability to undo liver fibrosis means that tackling the underlying cause — with antiviral drugs or by reducing alcohol intake, for instance — can help to resolve scarring. But there is also a need for drugs that directly target the fibrotic process to halt or even prevent scarring, and thereby lessen liver damage.
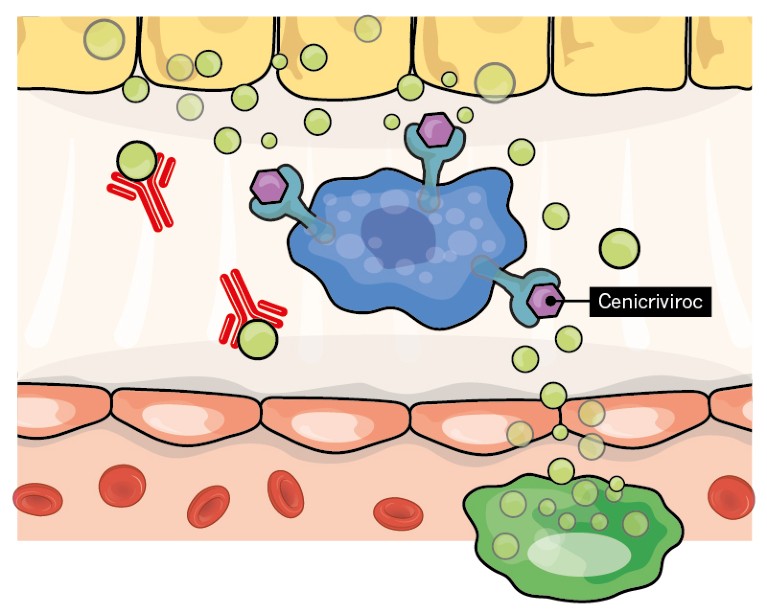
Shoot the messenger
Credit: Alisdair Macdonald
Drugs that prevent fibrosis-promoting signalling molecules, such as cytokines, from reaching HSCs are being investigated. Cenicriviroc, a small molecule that blocks two types of cytokine receptor, is now in phase III clinical trials. Small molecules that target other receptors, and antibodies that bind to secreted messengers, are also being explored.
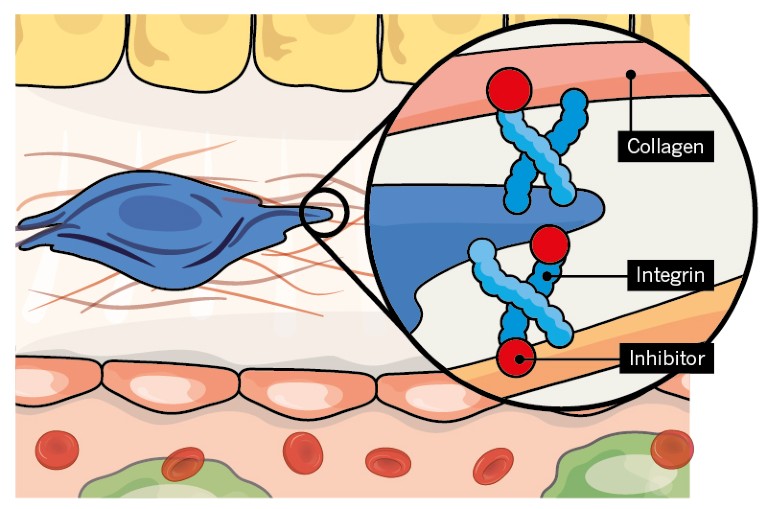
Interfere with integrins
Credit: Alisdair Macdonald
Integrins are cell-surface receptors that are activated by cell–extracellular matrix or cell–cell interactions. They can have multiple profibrotic effects. Integrins αvβ1 and αvβ6 have emerged as especially exciting targets for the treatment of liver fibrosis, and numerous small molecules and antibodies that inhibit integrins are approaching phase I trials.
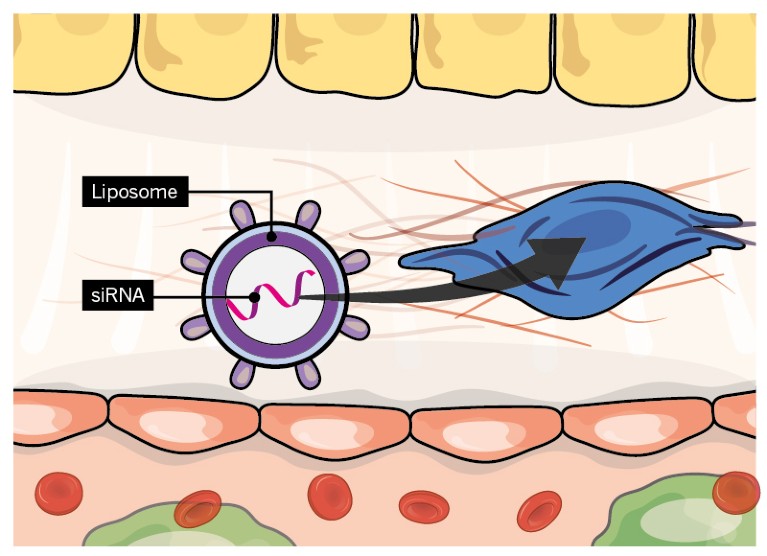
Destroy the matrix
Credit: Alisdair Macdonald
Small interfering RNAs (siRNAs) that halt collagen synthesis by binding to collagen- encoding messenger RNA are being pursued. An siRNA targeted to HSCs that suppresses a protein needed for collagen to mature has completed phase I trials. Drugs that block collagen cross-linking enzymes or inhibitors of enzymes that digest collagen might also aid scar breakdown.
Remove myofibroblasts
Credit: Alisdair Macdonald
Drugs that block intracellular signalling pathways that maintain HSC activation, or mimic signals that promote the death of myofibroblasts or their reversion to HSCs, are being sought to speed the resolution of fibrosis.
Bring on fresh players
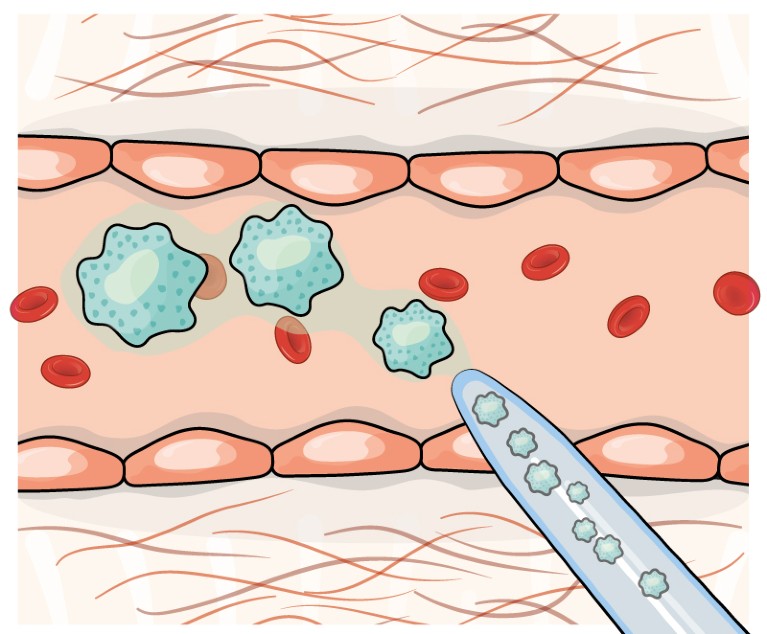
Credit: Alisdair Macdonald
Clinical trials that introduce stem cells into the liver have failed to induce therapeutic effects. But in the mouse liver, macrophages have been shown to produce strong antifibrotic effects8 — phase I trials are under way.
Challenges to overcome
Credit: Alisdair Macdonald
Liver fibrosis tends to progress over decades. Clinical trials can therefore take years to complete and often require many participants. But researchers are searching for biomarkers in blood that indicate changes in the rates of scar formation and breakdown. These molecules could reveal within a matter of weeks whether potential drugs are working.

 Nature Outline: Liver cirrhosis
Nature Outline: Liver cirrhosis
 Liver cirrhosis: scar wars
Liver cirrhosis: scar wars