Researchers in Japan, led by cardiac surgeon Yoshiki Sawa (second from right) at Osaka University, are pushing ahead with a stem-cell therapy for damaged hearts.Credit: Asahi Shimbun/Getty
As we report in a News story this week, Japan is set to push ahead with a promising treatment for heart disease that relies on stem cells. It could soon be made available under a fast-track approval system that the country put in place in 2014. Designed to speed access to regenerative therapies, the law allows prospective treatments to be marketed and used as long as they have been proved to be safe. Only a suggestion of efficacy is required — with more-convincing data supposed to be gathered retrospectively from patients who have been given the approved treatment.
The system has its critics — Nature among them (see Nature 528, 163–164; 2015). The latest move adds further concerns.
The therapy is the work of a physician who was also the first to take advantage of the new law with a related treatment: Osaka University cardiac surgeon Yoshiki Sawa. There is no suggestion that Sawa has not followed the rules, set out by the Pharmaceuticals and Medical Devices Agency. He has. The issue is whether those rules are adequate and appropriate and have the welfare of patients at their heart. They do not. Treatments of no proven efficacy are being sold to patients (who effectively subsidize the clinical trials to test them). They receive no refund if the therapy is subsequently found not to work. Patients also take risks: they undergo immunosuppression and the surgery itself.
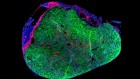
The new study takes induced pluripotent stem cells (iPS cells) that have been banked and characterized to ensure they are safe, and converts them to heart-muscle cells. These are then spread into a thin sheet that is attached to the weakened heart muscle. It is only the second clinical application of iPS cells and is generating excitement around the world. The problem is that the earlier treatment from Sawa — which is ongoing under the fast-track system — has yet to produce convincing results.
In that treatment, approved in September 2015, patients received a sheet of muscle cells made from their own leg tissue, rather than from iPS cells. Called HeartSheet, the muscle sheet is attached to weakened heart muscle that has usually been damaged as a result of a heart attack or plaque build-up and is often the cause of heart failure. The scientists behind the treatment speculate that the muscle cells work by releasing growth factors, not by becoming supporting tissue themselves. Other researchers are sceptical.
Now there are two new treatments being investigated for the same condition, and it’s impossible to know yet whether either will work or which might be best for individual patients.
It makes sense that heart-muscle cells (used in the second study) might work better for the heart than leg-muscle cells (used in the first). Indeed, it was reported a decade ago that injecting muscle cells from the leg did not improve heart function (P. Menasché et al. Circulation 17, 1189–1200; 2008).
Most physicians hoping to treat heart disease by way of regenerative medicine have moved on to other strategies, with many looking to heart-muscle cells. That doesn’t mean HeartSheet cannot work, but it does raise the question of whether patients who are given it will benefit.
Sawa himself has raised the issue. At a symposium last month touting the new iPS cell trial, he said “leg cells are not good, well, at least not enough”. And the Osaka University web page announcing the iPS cell trial says that HeartSheet was found to be ineffective for more serious cases. Sawa told Nature that the cells work in some cases, but that he expects the new iPS cell therapy to be more effective.
All this places a question mark over how the efficacy of HeartSheet can be proved as required. Half way through its scheduled 5-year plan, fewer than 10 patients — of the 60 required by the terms of its approval — have received the treatment. If the trial doesn’t make 60, the health ministry told Nature, there would either be an extension or the ministry would try to make a decision on the basis of the available data.
Some physicians have called for the HeartSheet tests to end and the data to be assessed before the new iPS cell study can begin. That might be an over-reaction, but pressure on the Japanese government is increasing. The government needs to move quickly to make sure that evaluation of the HeartSheet therapy is as rigorous as promised. As more treatments emerge, officials should make sure that — fast track or not — they have a valid claim to efficacy before being sold to patients.
A therapy for heart disease could be the first iPS-cell clinical breakthrough that Japan so ardently desires. The country shouldn’t sell short the promising technology or the patients who hope to benefit from it.

 A slow road for stem cells
A slow road for stem cells
 ‘Reprogrammed’ stem cells approved to mend human hearts for the first time
‘Reprogrammed’ stem cells approved to mend human hearts for the first time