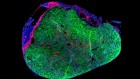
Embryonic stem cells have been developed slowly and so have a strong evidence base.Credit: Pedro Mara/Xinhua/ZUMA Wire
Regulators in the United States last week sought an injunction to stop a Florida company selling a controversial adult-stem-cell treatment for age-related macular degeneration (AMD). The move comes after three women treated by the company in 2005 went blind. The firm, now called US Stem Cell, hailed the cells as a therapy for AMD, which causes vision to blur so much that people affected can no longer recognize faces.
In the same year, two other people with AMD received a different stem-cell treatment at a London hospital. Those patients had patches made from embryonic stem cells implanted into their retinas. The scientists behind that therapy reported on the patients’ progress earlier this year: their eyesight had improved beyond expectations (L. da Cruz et al. Nature Biotechnol. 36, 328–337; 2018).
The conflicting outcomes highlight a difference between many treatments that use adult stem cells and those based on embryonic stem (ES) cells. ES-cell therapies emerged from a slowly built body of knowledge on how cells should be created and implanted, whereas adult-stem-cell treatments have too often been propelled by empty promises rather than by evidence.
Research with human ES cells has been slow because it was forced to be. Since scientists first created the cells 20 years ago, they have faced restrictions on funding and a need to pass through extra review committees, because of the sensitive nature of research based on donated human embryos. The path was difficult to navigate and full of setbacks, but something good came out of it.
Those who dared to proceed were few, but they were committed. Working under intense scrutiny, they progressed steadily, even if the work was too sluggish for some. Enter adult stem cells. Scientists, clinics and companies lined up to capitalize on the opportunity; many compared the ‘unethical’ nature of human ES cells with the ethical choice of adult stem cells. Some advertised, without evidence, how they were harnessing the body’s own power of rejuvenation. Some even kept a scorecard of adult-cell therapies marketed, versus zero for those from ES cells.
Adult stem cells can certainly be valuable. Bone-marrow transplants are a stem-cell therapy, and a tremendously successful one. Transplant of limbal stem cells found in the eye has fixed the corneas of hundreds of people. And last November, physicians in Italy reported using another kind of adult stem cell — epidermal — to save a German boy with a usually fatal skin disease (T. Hirsch et al. Nature 551, 327–332; 2017).
But in too many other cases, progress has been crippled by a lack of any proof of efficacy — in particular, when it comes to therapies based on mesenchymal stem cells taken from a person. Too many companies seeking a quick profit have exploited lax regulatory frameworks — in the United States and elsewhere — and the needs of desperate people facing sometimes terminal illnesses. Patient need has been presented as an excuse to forgo clinical trials. Careful bench experiments that were needed to reveal how the therapies might work have not been done.
The situation could get worse. An article last week argued that crowdfunding campaigns to drum up money for treatments accelerate the dissemination of inaccurate information (J. Snyder et al. J. Am. Med. Assoc. 319, 1935–1936; 2018).
Contrast that with solid scientific work that has shown, for example, how to use ES cells to derive retinal cells, pancreatic cells and dopamine-producing cells. Techniques based on years of rigorous work to characterize and develop ways of delivering these cells are now in or nearing clinical trials.
Other positive examples are described in a special Nature Insight supplement this week, which catalogues the growing knowledge base from experiments with ES cells that aim to treat diseases affecting the pancreas and brain. And it discusses innovative strategies, such as spurring ageing stem cells in the body to fight off disease.
Understandably, such progress can seem frustratingly slow to many patients. But speedy alternatives are more of a problem. Regulators have not been able to keep up. Last week’s request for an injunction is being heralded as a turning point in the US Food and Drug Administration’s (FDA’s) crackdown on clinics offering unproven stem-cell therapies. But there are still hundreds more such operators in the United States alone.
Other new treatments already hitting the market, including immunotherapy and gene therapy, are also vulnerable to hype. If the FDA and other regulators are to have any chance of sifting the good from the bad, and so protecting some of the most vulnerable people, they need to pick up the pace. Meanwhile, scientists should remember the merits of doing the opposite.


 Nature Insight: Regeneration
Nature Insight: Regeneration
 How human embryonic stem cells sparked a revolution
How human embryonic stem cells sparked a revolution
 Skin regeneration with insights
Skin regeneration with insights
 Behind the scenes of the world's first commercial stem-cell therapy
Behind the scenes of the world's first commercial stem-cell therapy