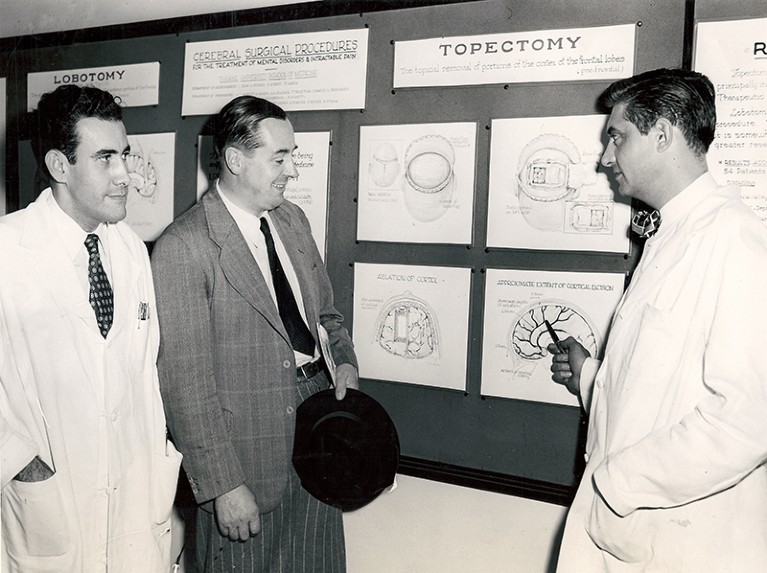
Robert Heath, far right, conducted experiments with brain stimulation.Credit: University Archives, Howard-Tilton Memorial Lib., Tulane Univ.
The Pleasure Shock: The Rise of Deep Brain Stimulation and Its Forgotten Inventor Lone Frank Dutton: 2018.
Many people consider deep-brain stimulation (DBS) to have begun in 1987 in Grenoble, France, when Pierre Pollak and Alim Benabid stopped a person’s tremor by delivering high-frequency pulses of electricity to her thalamus. In fact, more than three decades earlier, a psychiatrist called Robert G. Heath at Tulane University in New Orleans, Louisiana, had experimented with this approach. Now, science writer Lone Frank pulls Heath (1915–99) from obscurity for her exploration of DBS, The Pleasure Shock.
Frank has traced and interviewed surviving patients, former collaborators, family members and current DBS scientists. The result is a rarity: a thrilling, well-researched read. Above all, it is a chilling reminder of how early neurosurgical experimentation knew few ethical boundaries — even firmly within the medical and academic establishment. Heath was chair of Tulane’s psychiatry and neurology department for 31 years, from 1949 to 1980.
Today, DBS is an approved treatment for Parkinson’s disease, dystonia (uncontrollable muscle contractions) and essential tremor. Other indications, such as therapy for obsessive–compulsive disorder, depression and addiction, are the focus of intensive research. Just a few patients are treated ‘off label’, with mixed results.
Heath explored the effects of electrical stimulation on various people, with and without their informed consent. Infamously, in the 1970s he subjected a homosexual man to DBS — for so-called ‘conversion therapy’, the now-discredited practice of attempting to alter sexual preference. Heath delivered pulses to the septal region of the man’s brain (normally active during pleasure), and showed him pornographic material featuring women. Heath obtained permission from a state court to pay a woman to perform sexual acts with the man, while recording activity in his septum. Heath claimed that the man became heterosexual; this was later contested.
As early as the 1950s, Heath also implanted electrodes in people with schizophrenia, violent behaviour and depression. Towards the end of his career, he proposed stimulation of the cerebellum for the treatment of epilepsy, which he thought was closely related to schizophrenia.
Frank paints a detailed picture of the staggering ethical vacuum in which this egregious research was conducted. This was the period after the rise and fall of prefrontal lobotomies, from the 1940s to the 1950s. It was also when chlorpromazine was introduced as the first drug for psychosis. Several of the people Heath experimented on experienced post-operative complications, and contemporaries raised serious questions in the literature of the time about his methods and conclusions. All of this makes Heath’s long and troubling career a useful subject of study, because it illustrates the beginnings of biological psychiatry.
A strength of the book stems from the parallels that Frank draws with current brain research, notwithstanding today’s dramatically different protections for the dignity, rights and welfare of research participants. For example, Frank compares Heath’s involvement in the CIA’s mind-control experiment MKUltra, which ran from the 1950s to the 1970s, with the current DBS initiative led by the Defence Advanced Research Project Agency, which aims to understand the workings of the brain. The comparison might not please everyone, but it underlines the need for a debate on the independence of research in psychiatry.
Beyond DBS, Heath tested pharmacological substances such as bulbocapnine, which induces therapeutic stupor, on inmates of the Louisiana State Penitentiary at Angola, in the context of MKUltra. Sadly, he was not alone in using prisoners for medical research; from the 1940s to the 1960s, covert testing of drugs, radioactive substances and more was carried out on many people powerless to refuse.
Heath also propounded the idea that a component that he called taraxein, isolated from the blood serum of people with schizophrenia, would elicit symptoms in healthy people. The prisoners he injected quickly learned to perform what he expected them to, for example acting out hallucinations. The episode encapsulates both the alarming ethical mores of the day and why observations need to be made under blinded conditions.
There are a few gaps. Frank talked to many DBS experts, but not to Pollak or Benabid, who pioneered the most important use of the technique today, in the subthalamic nucleus. I also wanted to know whether Heath knew of the Nobel-prizewinning work of physiologist Walter Rudolf Hess on cats’ emotional reaction to electrical brain stimulation, carried out in the 1930s. That evidence could have been a stimulus for Heath’s experiments in humans. Some anatomical schematics could have helped the non-expert; and I wished for photographs of Heath at work.
Was Heath an out-and-out monster or a deeply flawed visionary? Frank does not shy away from that question. She vividly describes his charismatic, take-charge personality, analysing his work in the context of his time. He called his house outside New Orleans Hedonia (meaning pleasure); hosted lavish parties; and was a gifted tennis player, all of which probably contributed to his social success in the American deep south of the mid-twentieth century. Frank also makes it clear that much of Heath’s research — and the academic environment that allowed it — was appalling.
Today, little remains of Heath’s science, in part because he did not systematically investigate underlying mechanisms. In the absence of a demonstration of what causes a condition, it is difficult to propose a stimulation protocol that works. When DBS is used for Parkinson’s disease, we know that high-frequency stimulation in the subthalamic nucleus alleviates symptoms, even though the underlying cellular mechanism is debated.
The future of DBS seems bright thanks to optogenetics, the use of light to control the activity of cells. Over the past decade, scientists have teased apart neural dysfunction in animal models of behavioural conditions such as obsessive–compulsive disorder or addiction. New DBS protocols are currently tested in such models. Treatments likely to reach clinics over the few next years are inspired by optogenetic manipulations of cellular mechanisms to restore normal function in specific brain regions.
The main message of Frank’s fascinating, horrifying tale is that progress can be made only through research that is scrupulously ethical. Luckily for the patients of today and tomorrow, DBS got a second chance when it was reinvented in 1987.

 Psychiatry: A very sad story
Psychiatry: A very sad story
 Chemistry: The hidden war
Chemistry: The hidden war
 The wilder shores of brain boosting
The wilder shores of brain boosting





