- COMMENT
Deploy vaccines to fight superbugs
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Rent or buy this article
Prices vary by article type
from$1.95
to$39.95
Prices may be subject to local taxes which are calculated during checkout
Nature 552, 165-167 (2017)
doi: https://doi.org/10.1038/d41586-017-08323-0
References
The Review on Antimicrobial Resistance. Antimicrobial Resistance: Tackling A Crisis For The Health And Wealth Of Nations (Wellcome Trust and UK Government, 2014).
The Review on Antimicrobial Resistance. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations (Wellcome Trust and UK Government, 2016).
Falkow, S. Infectious Multiple Drug Resistance (Pion, 1975).
Kennedy, D. A. & Read, A. F. Proc. Biol. Sci. 284, 20162562 (2017).
Rappuoli, R., Pizza, M., Del Giudice, G. & De Gregorio, E. Proc. Natl Acad. Sci. USA 111, 12288–12293 (2014).
Rappuoli, R., Bottomley, M. J., D’Oro, U., Finco, O. & De Gregorio, E. J. Exp. Med. 213, 469–481 (2016).
Moriel, D. G. et al. MBio 3, e00118–12 (2012).
Cunningham, A. L. et al. N. Engl. J. Med. 375, 1019–1032 (2016).
von Gottberg, A. et al. N. Engl. J. Med. 371, 1889–1899 (2014).
Kwong, J. C., Maaten, S., Upshur, R. E., Patrick, D. M. & Marra, F. Clin. Infect Dis. 49, 750–756 (2009).
Competing Interests
R.R. is a full-time employee and shareholder at GlaxoSmithKline Vaccines.

 Antibiotic resistance has a language problem
Antibiotic resistance has a language problem
 Vaccines promoted as key to stamping out drug-resistant microbes
Vaccines promoted as key to stamping out drug-resistant microbes
 Combatting antimicrobial resistance globally
Combatting antimicrobial resistance globally
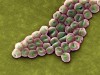 The drug-resistant bacteria that pose the greatest health threats
The drug-resistant bacteria that pose the greatest health threats
 Resistance to last-ditch antibiotic has spread farther than anticipated
Resistance to last-ditch antibiotic has spread farther than anticipated








