Abstract
First-line treatment of recurrent and/or refractory head and neck squamous cell carcinoma (HNSCC) is based on platinum, 5-fluorouracil (5-FU) and the monoclonal antiEGFR antibody cetuximab. However, in most cases this chemoimmunotherapy does not cure the disease, and more than 50% of HNSCC patients are dying because of local recurrence of the tumors. In the majority of cases, HNSCC overexpress the epidermal growth factor receptor (EGFR), and its presence is associated with a poor outcome. In this study, we engineered an EGFR-targeted oncolytic measles virus (MV), armed with the bifunctional enzyme cytosine deaminase/uracil phosphoribosyltransferase (CD/UPRT). CD/UPRT converts 5-fluorocytosine (5-FC) into the chemotherapeutic 5-FU, a mainstay of HNSCC chemotherapy. This virus efficiently replicates in and lyses primary HNSCC cells in vitro. Arming with CD/UPRT mediates efficient prodrug activation with high bystander killing of non-infected tumor cells. In mice bearing primary HNSCC xenografts, intratumoral administration of MV-antiEGFR resulted in statistically significant tumor growth delay and prolongation of survival. Importantly, combination with 5-FC is superior to virus-only treatment leading to significant tumor growth inhibition. Thus, chemovirotherapy with EGFR-targeted and CD/UPRT-armed MV is highly efficacious in preclinical settings with direct translational implications for a planned Phase I clinical trial of MV for locoregional treatment of HNSCC.
Similar content being viewed by others
Introduction
Head and neck cancer is currently the sixth most common cancer worldwide comprising 5% of all malignancies.1 A vast majority (>90%) of head and neck cancers represent squamous cell carcinomas (HNSCC) abundantly expressing the epidermal growth factor receptor (EGFR) associated with poor prognosis.2 Standard treatment regimens for recurrent and/or metastatic HNSCC were based on platinum plus 5-fluorouracil (5-FU). Therapeutic outcome could not be improved significantly for decades until the monoclonal antiEGFR antibody cetuximab augmented this regimen significantly. In the first-line setting, addition of cetuximab to platinum/5-FU prolongs survival from 7.4 to 10.1 months.3 Furthermore, cetuximab is active as monotherapy in patients with progressive disease after platinum-based treatment. However, in most cases there is no cure of disease, and substantial improvement of the current therapeutic outcome is urgently needed. Importantly, as the majority of patients suffer from local recurrence without metastatic disease, local delivery of therapeutics might be most favorable.
Oncolytic virotherapy, the treatment of cancer patients with replication-competent viruses, has progressed from preclinical experiments to clinical trials in humans.4, 5 Early clinical trials have demonstrated the safety of this approach, and oncolytic viruses are now being combined with chemotherapy in various multimodal approaches of chemovirotherapy.6 Particularly, for the treatment of advanced and/or metastasized HNSCC, Phase III clinical trials are going on using different oncolytics, which include vectors based on herpes simplex virus, adenovirus and reovirus in combination with platinum and/or taxane.7
Measles virus (MV) vectors based on the vaccine-lineage MV-Edmonston have proven to be a platform with broad utility, having been developed for the treatment of several types of cancer in preclinical settings.8, 9, 10, 11, 12, 13, 14, 15, 16 Since 2005, clinical trials including Phase I studies for treatment of ovarian cancer, myeloma and recurrent glioma are going on.17, 18, 19 Currently, improved specificity and efficacy are the main aims in the process of rational MV vector design. MV oncolytic specificity can be achieved by entry-targeting based on single-chain antibodies displayed on the viral attachment protein H blinded for its natural receptors CD46 and SLAM.20, 21 To date, a wide variety of tumor antigen-specific MV have been generated including vectors with EGFR specificity for glioma therapy.22 Furthermore, MV has shown great utility for delivering therapeutic transgenes to tumor cells, including the prodrug convertase Escherichia coli purine nucleoside phosphorylase. Expression of this particular transgene allows the virus to synergize with current clinical therapies, with purine nucleoside phosphorylase activating the clinically approved lymphoma drug fludarabine within the tumor microenvironment leading to bystander killing of uninfected tumor cells.10
A similar mechanism of action is the basis for treatment with the bi-functional prodrug convertase cytosine deaminase/uracil phosphoribosyltransferase (CD/UPRT) that locally activates the non-toxic prodrug 5-fluorocytosine (5-FC) to the chemotherapeutics 5-FU and 5-FU monophosphate. When converted into its active metabolites, 5-FU inhibits thymidylate synthase by incorporation into DNA and RNA eventually leading to inhibition of DNA and RNA synthesis and interference with DNA repair.23 To date, oncolytic efficacy of different vectors including vesicular stomatitis virus, vaccinia virus, herpes simplex virus and adenovirus has been enhanced significantly by arming with CD variants.24, 25, 26
In the present study, we hypothesized that an EGFR-specific MV locally activating 5-FU would offer highly specific and efficient chemovirotherapy for HNSCC abundantly expressing EGFR. We generated a recombinant MV fully retargeted with a single-chain antibody conferring selective entry through EGFR.27 This virus was armed with a chimeric gene encoding CD/UPRT to further enhance its oncolytic potency. We demonstrate that MV-CD/UPRT-antiEGFR can infect primary HNSCC in an EGFR-mediated manner, and exhibit a strong anti-tumor activity. Furthermore, we show that therapeutic efficacy in a xenograft model of HNSCC is enhanced significantly after systemic administration of the cognate prodrug 5-FC. These findings have direct translational implications for future clinical trials in chemovirotherapy of HNSCC with armed and targeted MV.
Materials and methods
Cell culture
Vero (African green monkey kidney) and HT1080 cells were purchased from American Type Culture Collection (Manassas, VA); HNO97, HNO210 and HNO410 cells were established from oral cavity (HNO97), larynx (HNO210) and hypopharyngeal lymph node metastasis (HNO410) HNSCC (kindly provided by Christel C. Herold-Mende, University Hospital Heidelberg, Germany) and cultured in Dulbecco's modified Eagle's medium (Invitrogen, Darmstadt, Germany) supplemented with 10% fetal bovine serum in a humidified atmosphere of 5% CO2 at 37 °C. Every specimen of the three HNSCC was obtained intraoperatively after informed consent and approval of the local ethics committee. Vero-αHis (kind gift of Stephen J. Russell, Mayo Clinic, Rochester, MN) and HT1080-CD20 cells were generated by stable transfection of the parental cell lines.28, 29 The breast ductal carcinoma cell line MCF-7 (kindly provided by Daniel Herr, University Hospital Ulm, Germany) was cultivated in RPMI supplemented with 10% fetal bovine serum. All cell lines were routinely checked for mycoplasma contamination using a multiplex cell contamination test (DKFZ Genomics and Proteomics Core facility, Heidelberg, Germany).30
Flow cytometry quantification of cell-surface EGFR
Trypsinized and resuspended cultured cells were washed and diluted in fluorescence-activated cell sorting (FACS) buffer (0.5% fetal bovine serum, 0.05% NaN3 in phosphate-buffered saline). Cells (5 × 105 each) were incubated either with antiEGFR monoclonal antibody cetuximab (Merck, Darmstadt, Germany) or with human IgG isotype control (Jackson ImmunoResearch, Suffolk, UK) at 3 μg ml−1 in FACS buffer on ice for 30 min. After washing, cells were stained with phycoerythrin-conjugated goat anti-human IgG (NatuTec, Frankfurt, Germany) at 10 μg ml−1 in FACS buffer for 15 min at room temperature. Washed cells were fixed in FACS buffer+1% paraformaldehyde for 10 min at 4 °C and analyzed by flow cytometry (BD LSRII; Becton Dickinson, Franklin Lakes, NJ, USA) using CellQuest software (Becton Dickinson).
Generation of recombinant MV
The constructions of MV genomic cDNA plasmids were based on pMV-EGFP31 (designated pMeGFPNV) containing the MV Edmonston-B vaccine lineage strain. The coding sequence of the single-chain variable fragment against EGFR27 was synthesized (Eurofins MWG, Ebersberg, Germany) containing flanking 5′-NotI and 3′-SfiI cloning sites. The NotI–SfiI fragment was inserted via exchange subcloning in pCG-HmutI-αCD20 containing the ‘blind’ H protein with CD46- and SLAM-ablating mutations10 leading to pCG-HmutI-αEGFR. Thereof, the EGFR-retargeted PacI–SpeI fragment was isolated and exchanged in pMV-EGFP resulting in the full-length genomic plasmid pMV-EGFP-antiEGFR. The hybrid open reading frame of E. coli CD/UPRT (pORF-codA::upp was purchased from InvivoGen, San Diego, CA) was subcloned via flanking MluI/AatII sites. In pMV-EGFP-antiEGFR, the EGFP cassette was removed via MluI and AatII digestion and replaced with the respective CD/UPRT fragment, giving rise to pMV-CD-antiEGFR. All cloning steps were designed to fulfill the rule of six as a requirement for recombinant MV.32, 33
Recombinant MV particles were generated from cDNA constructs according to Radecke et al.,32 and fully retargeted viruses were subsequently propagated on Vero-αHis cells as described previously.28 To prepare virus stocks, Vero-αHis cells were infected at a multiplicity of infection (MOI) of 0.03 and incubated at 37 °C for 36 h. Viral particles were harvested by one freeze/thaw cycle and centrifugation from their cellular substrate resuspended in Opti-MEM (Invitrogen). All following infection experiments were performed with viral stocks from the third passage. Titers were determined by 50% tissue culture infectious dose (TCID50) titration on Vero-αHis cells.
Virus infection
Cell lines (seeded in a 6, 12 or 24-well plate) were infected with the respective MV variant at an MOI of 0.01, 0.1 or 1 in Opti-MEM (Invitrogen) for 3 h at 37 °C. The inoculum was removed and the cells were maintained in their standard medium. Infected cells were photographed using a fluorescence microscope (Cell Observer; Zeiss, Jena, Germany) and the software Axiovision (Zeiss), or subjected to cell viability assay.
One-step growth kinetics and viral replication in presence of prodrug
HNO97 and Vero-αHis cells were infected with the respective MV variant at a MOI of 3 in duplicates. At designated time points (24, 36, 48, 72 and 96 h post infection (p.i.)), cells were scraped into the medium and the titers of progeny virus particles were determined in octuplicates by serial dilutions on Vero-αHis cells. Individual syncytia in all wells of the appropriate dilution step were counted 48 h p.i. and the viral titer (infectious units per ml) was calculated. Vero cells were infected with MV-CD or MV-TK at a MOI of 0.01. The inoculum was removed 2 h later and replaced with standard medium containing additionally 5-FC at various concentrations. Fifty hours later, cells were scraped into fresh media and the infectivity was determined in a titration assay.
Cell viability assay of infected/prodrug-converting cells
Cell viability was determined in using the Cell Viability Kit III (PromoKine, Heidelberg, Germany) according to the manufacturer's instructions. Cells were grown in 96-well microtiter plates (104 cells per well) in the recommended culture medium. Infection at MOI 0.01, 0.1 or 1 was carried out by adding the respective virus to the cells. Thirty-six hours after infection, the prodrug 5-FC (final concentration of 1 mM) or 0.9% NaCl (mock treatment) was added accordingly to the samples and cell viability was measured at the indicated time after infection by dye absorbance at 465 nm using an automated microplate reader (SpectraMax 340PC384; Molecular Devices, Ismaning, Germany). The viability of cells treated with or without the respective agents was calculated as the mean of quadruplicate OD values and expressed in relation to the untreated control samples (100% viable).
Bystander killing measurement in vitro
In a 24-well plate, 105 Vero-αHis cells were seeded, infected 6 h later at a MOI of 0.1 with MV-CD-antiEGFR and incubated for 36 h. 5-Fluorocytosine (Sigma-Aldrich, Taufkirchen, Germany) was added to the media at a final concentration of 1 mM for 12 h. Supernatants were harvested, cleared by centrifugation and heat inactivated at 60 °C for 30 min. Different fractions of conditioned media (0.5; 0.1; 0.01; 0.001) were transferred onto fresh test cell monolayers in 96-well plates (104 cells per well) in quadruplicates. The cytotoxic effect was measured 72 h after the transfer via XTT assay.
Subcutaneous xenograft tumor model
All animal experimental procedures were approved by the responsible Animal Protection Officer at the German Cancer Research Center and by the Regional Council according to the German Animal Protection Law. Tumors were established by inoculating subcutaneously HNO97 cells (5 × 106) in a total volume of 100 μl phosphate-buffered saline into the right flank of 6- to 8-weeks-old female immunodeficient NOD/SCID mice (Harlan, Borchen, Germany). When solid tumors reached an average volume of 50 μl, they were injected with 3 × 106 infectious units of MV-CD-antiEGFR in 100 μl Opti-MEM on five consecutive days. Two days after the last virus application, mice received 200 mg kg−1 per dose of 5-FC twice daily by intraperitoneal injection on five consecutive days. The control animals were injected with equal volumes of Opti-MEM containing no virus and saline containing no 5-FC, respectively. Tumor diameters were measured every third day (starting from the day of implantation) using a caliper, and the volume was calculated by the formula (largest diameter) × (smallest diameter)2 × 0.5. Mice were examined daily, tumor size and body weight was measured every 3 days. Animals were killed by cervical dislocation, if tumor ulceration occurred (maximum diameter more than 6 mm) or when tumor volume reached 1500 μl.
Statistics
Statistical analyses were performed using the GraphPad Prism software (version 5.04; GraphPad Software, La Jolla, CA, USA). Comparisons of data in cytotoxic effects were carried out using the two-tailed Student's t test. We applied the two-way analysis of variance test on the data to support the conclusion of tumor growth inhibition. Survival was analyzed by the Kaplan–Meier survival curves with comparison carried out by the log-rank test. Statistical differences were considered significant at P-values less than 0.05 and highly significant at P-values less than 0.001.
Results
Generation of CD/UPRT-armed and EGFR-targeted MVs
We generated recombinant MV from the Edmonston vaccine strain lineage with modifications in the attachment protein hemagglutinin (H) that ablate entry through the natural MV receptors CD46 and SLAM,20 and include the C-terminally fused single-chain antibody (scFv) against human EGFR27 for retargeted infection via EGFR. To enhance oncolytic properties, the hybrid prodrug convertase gene E. coli CD/UPRT was inserted in an additional transcription unit preceding the N gene (Figure 1, line MV-CD-antiEGFR). Furthermore, MV vectors coding for the reporter gene enhanced green fluorescent protein (EGFP) in combination with unmodified H (MV-EGFP), EGFR-targeted H (MV-EGFP-antiEGFR), and CD20-targeted H (MV-EGFP-antiCD20)10 were generated as controls.
Schematic representation of recombinant MV genomes. Vectors harbor either unmodified hemagglutinin (H) or fully retargeted H against EGFR and CD20 (listed at the bottom, middle), respectively, in combination with transgene X=EGFP or the hybrid E.coli CD/UPRT (listed at the bottom, left). Corresponding names of viruses are listed at the bottom right side.
Retargeted infection of HNSCC via EGFR
Surface expression of the designated receptor EGFR was determined via FACS analysis (Figure 2a). Primary HNSCC lines HNO97, HNO210 and HNO410 showed a differential pattern of EGFR surface density with the highest expression level on HNO97. In contrast, only a marginal EGFR expression could be detected on the control cell line MCF-7.
Targeting specificity of MV-EGFP-antiEGFR. (a) Mean fluorescence intensity of the surface marker EGFR was determined via FACS analyses of HNO97 (continuous line), HNO210 (dotted), HNO410 (broken) and MCF-7 as control (gray marked). (b) Three HNSCC cell lines, MCF-7, HT1080-CD20 and Vero-αHis cells were infected with the respective viruses (indicated above of each row) at a MOI of 1. Pictures were taken at 48 h p.i. using a fluorescence microscope ( × 100 magnification). Merged pictures of EGFP fluorescence and phase contrast are shown.
Next, to assess the specificity of retargeted infection, we infected a panel of different cell lines including HNO97, HNO210 and HNO410, MCF-7, Vero-αHis28 and transgenic HT1080-CD2029 at MOI of 1, and monitored for the appearance of syncytia formation and EGFP expression, reporting viral replication (Figure 2b). In all cell lines tested, MV-EGFP infection via ubiquitous CD46 caused the characteristic MV cytopathic effect of syncytia formation followed by cell death (Figure 2b, column MV-EGFP). Importantly, all HNSCC variants were efficiently infected by the fully retargeted MV-EGFP-antiEGFR virus (Figure 2b, column MV-EGFP-antiEGFR). In contrast, no virus-induced syncytia formation at all could be detected in MCF-7. Targeted infection with the control virus MV-EGFP-antiCD20 occurred only in HT1080-CD20 cells (Figure 2b, column MV-EGFP-antiCD20), but no syncytia formation could be detected on HNSCC cell lines or MCF-7 at any time point. The producer cells Vero-αHis were highly susceptible to all MV variants (fully retargeted H variants are displaying a C-terminal histidine hexapeptide for infection via the His-antibody pseudoreceptor on Vero-αHis cells) and showed complete lysis at 48 h p.i.
In summary, we demonstrated highly specific viral infection via EGFR without any visible impact on syncytia formation by EGFR targeting.
Retargeting of MV against EGFR and arming with CD/UPRT does not impair growth kinetics at early stages
To enhance the oncolytic potential of EGFR-retargeted MV, the hybrid gene of E. coli CD/UPRT was inserted into the viral genome (see Figure 1) leading to the armed and targeted virus designated MV-CD-antiEGFR. The kinetics of replication in target HNSCC cells (HNO97) was tested in a one-step growth curve assay, comparing the unmodified parental virus MV-EGFP, the retargeted variants MV-EGFP-antiEGFR and MV-CD-antiEGFR (Figure 3a). All virus variants reached similar titers and showed comparable growth kinetics on HNO97 and Vero-αHis 48 h p.i. The amount of progeny particles from MV-EGFP and MV-CD-antiEGFR infections started to differ by a factor of about 7 only at later stages after 72 and 96 h p.i., excluding a significant impairment of viral replication by the dual arming and retargeting approach of MV-CD-antiEGFR.
Viral replication kinetics. (a) One-step growth curves were performed by infection (MOI=3) of HNO97 and Vero-αHis cells in duplicates with MV-EGFP (circle), MV-EGFP-antiEGFR (square) or MV-CD-antiEGFR (triangle). Titers of progeny particles after the indicated time points were determined in octuplicates by serial dilution titration assay on Vero-αHis cells. (b) Vero cells were infected with MV-CD or MV-TK (MOI=0.01) and incubated with increasing concentrations of 5-FC. Titers of progeny particles were determined 50 h later. Detection limit for the titration assay is 100 ciu ml−1.
To determine the influence of prodrug on viral progeny production we assessed viral replication in the presence of 5-FC (Figure 3b). Two hours post infection with MV-CD or the control virus MV-TK (encoding the Herpes simplex thymidine kinase; unpublished data) at MOI 0.01 different amounts (0, 10, 100, 500 and 1000 μM) of 5-FC were added to the media and incubated for 50 h before viral titers were determined. Replication of MV-CD was completely inhibited at 5-FC concentrations of 500 μM and above. MV-TK grew to the expected titers in the range of 106 ciu/ml and was unaffected under the same conditions even in the presence of 1000 μM 5-FC. As expected, since infected cells expressing CD are eliminated when 5-FC is administered, production of viral progeny is also impaired at this point. Obviously, these findings indicate the importance of adequately scheduled prodrug administration after oncolytic virus application in vivo.
The hybrid prodrug convertase CD/UPRT enhances cytotoxicity of EGFR-retargeted MV
Supporting cytotoxicity of the CD/UPRT/5-FC system was assessed quantitatively by infection of HNO97, HNO210, HNO410 and Vero-αHis cell lines with MV-CD-antiEGFR at MOIs of 0.01, 0.1 and 1 (Figure 4). The prodrug 5-FC (right column) or no drug (left column) was added 36 h p.i. at a final concentration of 1 mM and cell viability was determined at 36, 48, 72 and 96 h p.i. Early after infection, toxicity to the HNSCC cell lines was moderate without prodrug, but more pronounced after 72 and 96 h, at least at the higher MOI of 1. As expected, 5-FC applied alone was not toxic to any cell line. In clear contrast, infections with MV-CD-antiEGFR at different MOIs followed by prodrug application resulted in major cytotoxicity, accelerating almost complete cell lysis after 96 h for all HNSCC lines (4–21% remaining viability at MOI=1) and Vero-αHis control cells.
Cytotoxic efficacy of prodrug convertase CD/UPRT. HNO97, HNO210, HNO410 and Vero-αHis (104 cells each) were infected in quadruplicates with MV-CD-antiEGFR (triangle) at a MOI of 0.01 (continuous line), 0.1 (broken) or 1 (dotted) for 36 h and incubated without 5-FC (left column) or with 1 mM 5-FC (right column). Cell viability was determined at the indicated time points after infection. Means (and standard deviations only for values at 96 h) are shown (circle/continuous line, mock-treated cells defining 100% viability; square/continuous line, 5-FC only treated).
Even at a low MOI of 0.1 and 1 mM 5-FC a significant cytoredutctive effect (77–52% cell killing) was achieved for the HNSCC using the combined chemovirotherapy. Thus, local activation of 5-FC by CD/UPRT enhances viral cytotoxicity significantly in HNSCC even when only about 10% of the cells were initially infected.
CD/UPRT-armed MV in combination with 5-FC activation enables efficient bystander tumor cell killing
To assess bystander cell killing after toxification of the prodrug 5-FC, Vero-αHis cells were infected with MV-CD-antiEGFR at a MOI of 0.1, and 5-FC was added 36 h p.i. (final concentration 1 mM). As controls, Vero-αHis cells were mock-treated, infected with MV-CD-antiEGFR alone or incubated with prodrug only. After heat inactivation of viral particles in the collected cell supernatants, different fractions (0.1 and 0.001) of conditioned media were transferred onto subconfluent layers of the HNO97, HNO210, HNO410 and Vero-αHis cell lines, and viability was quantified 72 h later (Figure 5). In all HNSCC cells tested, toxicity increased with higher concentrations of the conditioned media derived from the infected Vero-αHis cells incubated with 5-FC. In clear contrast, test cells incubated with supernatants from non-infected Vero-αHis cells, infected with MV-CD-antiEGFR alone, or incubated with 5-FC only did not show significant differences in viability. Transfer of conditioned media using a fraction of 0.001 induced toxicity in all cell lines in a broader range of 33–56%, whereas the higher concentrated fraction of 0.1 had a strongly pronounced and similar impact (83–93% toxicity) on all cell lines used. Therefore, arming with CD/UPRT mediates highly efficient prodrug conversion providing bystander killing of non-infected tumor cells.
Cytotoxic efficacy of activated 5-FC in conditioned media. Vero-αHis cells were mock treated, treated with 1 mM 5-FC, infected with MV-CD-antiEGFR (MOI=0.1), or infected with MV-CD-antiEGFR and incubated with 1 mM 5-FC at 36 h p.i. for 12 h. Different fractions (0.001 and 0.1) of the conditioned and heat-inactivated media were added to fresh cell layers (HNO97, HNO210, HNO410 and Vero-αHis). Viability was determined 72 h after transfer via XTT assay. Means and standard deviations from four experiments are shown (black, mock-treated cells defining 100% viability; white, 5-FC alone; dark gray, MV-CD-antiEGFR; light gray, MV-CD-antiEGFR +5-FC).
Prodrug-enhanced chemovirotherapy of HNSCC xenografts
The anti-tumor activity of retargeted and armed MV-CD-antiEGFR was assessed after subcutaneous implantation of HNO97 xenografts in immunodeficient NOD/SCID mice. In an approach of chemovirotherapy, we compared the oncolytic potency of MV-CD-antiEGFR in presence of 5-FC with MV-CD-antiEGFR alone, to 5-FC alone or to mock treatment (Figure 6). When tumors reached an average volume of 50 μl at day 6 after implantation, mice were randomized into four groups (n=11 per group) and tumor diameters were measured every 3 days.
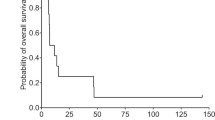
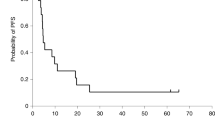
In vivo anti-tumor activity of MV-CD-antiEGFR with 5-FC. HNO97 cells (5 × 106) were implanted subcutaneously into the right flank of 6- to 8-weeks-old NOD/SCID mice (n=11 per group). When tumor volumes reached 50 μl, each mouse received five intratumoral doses on five consecutive days (3 × 106 infectious units each). 5-FC was given i.p. (200 mg kg−1 per dose, twice daily) 2 days after the last MV application on five consecutive days (circle, mock-treated animals; square, treated with 5-FC only; triangle, MV-CD-antiEGFR only; diamond, MV-EGFP-antiEGFR+5-FC). (a) Average tumor volumes of mice in each group (error bars indicate standard deviation of the mean; only upper parts are shown). (b) Distribution of tumor volumes at day 24 after implantation. Each dot represents one mouse. (c) Kaplan–Meier survival curve documenting the effects of oncolytic MV-CD-antiEGFR and prodrug, respectively. (d) Manifestation of tumor development at day 24 after implantation (Scale bar: 1 mm length).
Tumors of the first two groups were mock treated; the other two groups received MV-CD-antiEGFR (3 × 106 infectious units) intratumorally with a total of five injections on consecutive days. Subsequently 2 days after the last virus application, mice were treated via intraperitoneal injections accordingly to their group with saline or 5-FC (200 mg kg−1 twice daily) for 5 days. Oncolytic effects with potent tumor growth retardation were documented for mice treated with MV-CD-antiEGFR alone or MV-CD-antiEGFR in combination with 5-FC compared with the mock or 5-FC control groups (Figure 6a). The difference in tumor sizes between mock treatment and the chemovirotherapy was considered significant (P<0.05) from day 12 on, whereas the difference in tumor sizes between MV only and the combined treatment was considered significant (P<0.05) from day 21 on after implantation.
As shown for the tumor volume at day 24 after implantation (Figure 6b), treatment with MV-CD-antiEGFR and 5-FC resulted in a significantly enhanced oncolysis compared with sole viral (P<0.05) or sole 5-FC treatment (P<0.0001). The mean tumor volume at day 24 after implantation was 266 μl in the mock group and 250 μl in the 5-FC treated group, compared with 71 μl in the virus treated group and 18 μl in the chemovirotherapy group. Thus, the combined therapy resulted in a highly significant difference in mean tumor volume compared with mock treatment (P<0.0001; 15-times smaller mean tumor volume). Importantly, 2 out of 11 animals in the virus treated group and 5 out of 11 animals having obtained combined chemovirotherapy showed complete tumor remission at day 24 (Figures 6b and d).
Survival benefits were estimated using the Kaplan–Meier survival curves (Figure 6c) with defined endpoints (tumor ulceration >6 mm in diameter or tumor volume >1500 μl). Treatment with MV-CD-antiEGFR in the presence of 5-FC resulted in a highly significant increase of survival time compared with the mock treatment or administration of prodrug alone (P<0.0001 each). Combined chemovirotherapy was significantly superior in terms of survival compared with virus treatment alone at day 60 (P<0.0001). The median survival of mock-treated animals was 27 days, whereas 50% of mice having obtained viral and prodrug therapy survived until day 90 and until day 78 with sole virus application, respectively.
Moreover, no significant influence on mouse weight was detected for any treatment regimen including virus. Thus, chemovirotherapy represents a beneficial treatment regimen in this model of HNSCC.
Discussion
Advanced stages III/IV HNSCC are a clinical challenge with poor prognosis. In contrast to most other solid cancers, more than 50% of HNSCC patients are dying because of local recurrence of the tumors without having metastatic disease. In the majority of cases HNSCC overexpress the EGFR, and its presence is associated with a poor outcome.3 Consequently, standard of care is cetuximab in combination with radiotherapy, chemotherapy (platinum and/or 5-FU) or radiochemotherapy.
For most oncolytic viruses, local application seems to be favorable as this route of administration circumvents vector neutralization by circulating antibodies and avoids trapping of the vector in non-target organs. As most HNSCC are located in the oropharynx, hypopharynx, larynx or in the oral cavity, they are easily accessible for locoregional treatment and monitoring.
In this study, we demonstrated highly efficient killing of HNSCC by recombinant MV with vaccine strain tropism. HNSCC tumors are expressing the MV receptor CD46 abundantly.34 Hence, the three investigated HNSCC cell lines with different origins (oropharynx, larynx and cervical metastasis of a hypopharynx squamous cell carcinoma) were permissive to MV-EGFP, indicating efficient cell entry via CD46 and robust replication with a strong consecutive cytopathic effect.
For more specific cell entry, we generated an EGFR-targeted MV. As shown here, HNSCC cell lines were highly permissive to the MV-EGFP-antiEGFR with a significant cytopathic effect, whereas the low-level EGFR expressing breast ductal carcinoma control cell line MCF-7 did not show any syncytia formation.
To further improve the oncolytic MV system for treatment of HNSCC we armed the EGFR-retargeted vector with the bi-functional prodrug convertase CD/UPRT. It converts the non-toxic anti-fungal agent 5-FC into the chemotherapeutic agent 5-FU, a mainstay of HNSCC chemotherapy. Application of MV-CD-antiEGFR in combination with 5-FC resulted in enhanced cell killing in vitro (>80% cell death). Even a 0.001 fraction of conditioned media containing activated prodrug (from MV-CD-antiEGFR-infected Vero-αHis cells incubated with 5-FC) is killing 33–60% of cultured HNSCC cells, indicating a high bystander effect in vitro. Treatment of HNSCC xenografts in NOD/SCID mice using MV-CD-antiEGFR with or without prodrug resulted in highly significant overall survival for both MV-treated groups. Additional administration of 5-FC had an even more pronounced therapeutic benefit, and no systemic toxicity was detected by monitoring stable body weight and good general health conditions of all animal groups. However, further improvement of therapeutic outcome might be possible by optimizing the treatment schedule. Timing of prodrug administration after oncolytic virus delivery can be critical as previously demonstrated.15 In an empirical attempt to synchronize prodrug delivery with high levels of virus replication in vivo, we aimed to define the optimal time window between virus inoculation and prodrug delivery. In a lymphoma xenograft model maximum efficiency of oncolysis was achieved with a schedule in which prodrug was given one week after the last virus application. In this experimental setting, both extending and reducing this time window of subsequent prodrug administration led to decreased therapeutic outcome. In the current study we decided to schedule the prodrug administration 2 days after the last virus injection assuming that MV replication in HNSCC xenografts is less pronounced than in lymphomas and therefore the oncolytic effect needs to be boosted at an earlier time point. We chose 200 mg kg−1 per dose of 5-FC twice daily on five consecutive days, which is in the range of previously published treatment regimes using the CD/5-FC system to enhance viral oncolysis.35 However, in the present study, for the first time CD was encoded on a MV vector and data from other armed oncolytic viruses are hardly conferrable unbiased. The use of trackable MV, for example, encoding carcinoembryonic antigen as a soluble surrogate marker for viral replication, would help rendering prodrug timing even more precisely in the future.17
Up to now, three MV clinical trials have been initiated at the Mayo Clinic, exclusively conducted with untargeted virus,36 taking advantage of the preferential replication of MV in malignant cells. The MV-CD-antiEGFR is a newly designed MV vector intended for clinical translation, which is fully retargeted. Although locoregional application is planned for the treatment of HNSCC patients, we hypothesize that application of an EGFR-targeted MV will be beneficial, because dose limiting toxicity will be diminished due to vector restriction on the cell entry level to the highly EGFR-expressing tumor cells.37, 38 Even if dose limiting toxicity was not reached in ongoing MV trials so far, it could be the limiting factor in the planned setting of repeated direct intratumoral injection of HNSCC with single doses of >108 TCID50 and local prodrug toxification.
Future treatment efficacy of armed and targeted MV for HNSCC might further be improved in a multimodal approach with conventional therapies including radiotherapy and/or platinum. To date, first clinical studies using oncolytic viruses in HNSCC were conducted with a replication-selective adenovirus, combined with radiotherapy,39 and with herpes simplex virus40, 41 in Phase I/II studies in combination with radiotherapy and cisplatin in untreated stage III/IV HNSCC.7 First results suggested safety and some evidence of efficacy of these replicative oncolytic viruses. In a Phase III trial of patients with advanced head and neck carcinoma, the combination of chemotherapy (5-FU or adriamycin and cisplatin) with an intratumorally injected oncolytic adenovirus versus no virotherapy showed a synergistic effect.6 Moreover, adenovirus H101 in combination with cisplatin for treatment of HNSCC was the first oncolytic virus approved as a routine cancer drug in China in 2005.42
In the present study, we demonstrate that MV vaccine strain with unmodified tropism can infect, replicate in and kill HNSCC efficiently. To improve the therapeutic index of MV for the treatment of HNSCC abundantly expressing EGFR, we engineered an EGFR-targeted MV. In addition, this virus was armed with a chimeric gene encoding CD/UPRT to further enhance its oncolytic potency. We demonstrated in vitro and in vivo that MV-CD-antiEGFR can infect HNSCC via the designated receptor EGFR, and exhibited a strong anti-tumor activity. Furthermore, therapeutic efficacy was enhanced by administration of the cognate prodrug 5-FC. Hereby, the existing toolbox of recombinant MV is extended by a highly specific and effective vector for HNSCC, paving the way for clinical testing of this approach.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D . Global cancer statistics. CA Cancer J Clin 2011; 61: 69–90.
Temam S, Kawaguchi H, El-Naggar AK, Jelinek J, Tang H, Liu DD et al. Epidermal growth factor receptor copy number alterations correlate with poor clinical outcome in patients with head and neck squamous cancer. J Clin Oncol 2007; 25: 2164–2170.
Vermorken JB, Mesia R, Rivera F, Remenar E, Kawecki A, Rottey S et al. Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med 2008; 359: 1116–1127.
Pan JJ, Zhang SW, Chen CB, Xiao SW, Sun Y, Liu CQ et al. Effect of recombinant adenovirus-p53 combined with radiotherapy on long-term prognosis of advanced nasopharyngeal carcinoma. J Clin Oncol 2009; 27: 799–804.
Chang J, Zhao X, Wu X, Guo Y, Guo H, Cao J et al. A Phase I study of KH901, a conditionally replicating granulocyte-macrophage colony-stimulating factor: armed oncolytic adenovirus for the treatment of head and neck cancers. Cancer Biol Ther 2009; 8: 676–682.
Xia ZJ, Chang JH, Zhang L, Jiang WQ, Guan ZZ, Liu JW et al. [Phase III randomized clinical trial of intratumoral injection of E1B gene-deleted adenovirus (H101) combined with cisplatin-based chemotherapy in treating squamous cell cancer of head and neck or esophagus]. Ai Zheng 2004; 23: 1666–1670.
Harrington KJ, Hingorani M, Tanay MA, Hickey J, Bhide SA, Clarke PM et al. Phase I/II study of oncolytic HSV GM-CSF in combination with radiotherapy and cisplatin in untreated stage III/IV squamous cell cancer of the head and neck. Clin Cancer Res 2010; 16: 4005–4015.
Blechacz B, Splinter PL, Greiner S, Myers R, Peng KW, Federspiel MJ et al. Engineered measles virus as a novel oncolytic viral therapy system for hepatocellular carcinoma. Hepatology 2006; 44: 1465–1477.
Ungerechts G, Springfeld C, Frenzke ME, Lampe J, Parker WB, Sorscher EJ et al. An immunocompetent murine model for oncolysis with an armed and targeted measles virus. Mol Ther 2007; 15: 1991–1997.
Ungerechts G, Springfeld C, Frenzke ME, Lampe J, Johnston PB, Parker WB et al. Lymphoma chemovirotherapy: CD20-targeted and convertase-armed measles virus can synergize with fludarabine. Cancer Res 2007; 67: 10939–10947.
Allen C, Paraskevakou G, Iankov I, Giannini C, Schroeder M, Sarkaria J et al. Interleukin-13 displaying retargeted oncolytic measles virus strains have significant activity against gliomas with improved specificity. Mol Ther 2008; 16: 1556–1564.
Liu C, Hasegawa K, Russell SJ, Sadelain M, Peng KW . Prostate-specific membrane antigen retargeted measles virotherapy for the treatment of prostate cancer. Prostate 2009; 69: 1128–1141.
Msaouel P, Iankov ID, Allen C, Morris JC, von Messling V, Cattaneo R et al. Engineered measles virus as a novel oncolytic therapy against prostate cancer. Prostate 2009; 69: 82–91.
Li H, Peng KW, Dingli D, Kratzke RA, Russell SJ . Oncolytic measles viruses encoding interferon beta and the thyroidal sodium iodide symporter gene for mesothelioma virotherapy. Cancer Gene Ther 2010; 17: 550–558.
Ungerechts G, Frenzke ME, Yaiw KC, Miest T, Johnston PB, Cattaneo R . Mantle cell lymphoma salvage regimen: synergy between a reprogrammed oncolytic virus and two chemotherapeutics. Gene Ther 2010; 17: 1506–1516.
Leber MF, Bossow S, Leonard VH, Zaoui K, Grossardt C, Frenzke M et al. MicroRNA-sensitive oncolytic measles viruses for cancer-specific vector tropism. Mol Ther 2011; 19: 1097–1106.
Peng KW, TenEyck CJ, Galanis E, Kalli KR, Hartmann LC, Russell SJ . Intraperitoneal therapy of ovarian cancer using an engineered measles virus. Cancer Res 2002; 62: 4656–4662.
Dingli D, Peng KW, Harvey ME, Greipp PR, O’Connor MK, Cattaneo R et al. Image-guided radiovirotherapy for multiple myeloma using a recombinant measles virus expressing the thyroidal sodium iodide symporter. Blood 2004; 103: 1641–1646.
Galanis E, Hartmann LC, Cliby WA, Long HJ, Peethambaram PP, Barrette BA et al. Phase I trial of intraperitoneal administration of an oncolytic measles virus strain engineered to express carcinoembryonic antigen for recurrent ovarian cancer. Cancer Res 2010; 70: 875–882.
Vongpunsawad S, Oezgun N, Braun W, Cattaneo R . Selectively receptor-blind measles viruses: identification of residues necessary for SLAM- or CD46-induced fusion and their localization on a new hemagglutinin structural model. J Virol 2004; 78: 302–313.
Nakamura T, Peng KW, Vongpunsawad S, Harvey M, Mizuguchi H, Hayakawa T et al. Antibody-targeted cell fusion. Nat Biotechnol 2004; 22: 331–336.
Paraskevakou G, Allen C, Nakamura T, Zollman P, James CD, Peng KW et al. Epidermal growth factor receptor (EGFR)-retargeted measles virus strains effectively target EGFR- or EGFRvIII expressing gliomas. Mol Ther 2007; 15: 677–686.
Longley DB, Harkin DP, Johnston PG . 5-fluorouracil: mechanisms of action and clinical strategies. Nat Rev Cancer 2003; 3: 330–338.
Porosnicu M, Mian A, Barber GN . The oncolytic effect of recombinant vesicular stomatitis virus is enhanced by expression of the fusion cytosine deaminase/uracil phosphoribosyltransferase suicide gene. Cancer Res 2003; 63: 8366–8376.
Cao X, Huang X, Ju DW, Zhang W, Hamada H, Wang J . Enhanced antitumoral effect of adenovirus-mediated cytosine deaminase gene therapy by induction of antigen-presenting cells through stem cell factor/granulocyte-macrophage colony-stimulating factor gene transfer. Cancer Gene Ther 2000; 7: 177–186.
Nakamura H, Mullen JT, Chandrasekhar S, Pawlik TM, Yoon SS, Tanabe KK . Multimodality therapy with a replication-conditional herpes simplex virus 1 mutant that expresses yeast cytosine deaminase for intratumoral conversion of 5-fluorocytosine to 5-fluorouracil. Cancer Res 2001; 61: 5447–5452.
Kettleborough CA, Ansell KH, Allen RW, Rosell-Vives E, Gussow DH, Bendig MM . Isolation of tumor cell-specific single-chain Fv from immunized mice using phage-antibody libraries and the re-construction of whole antibodies from these antibody fragments. Eur J Immunol 1994; 24: 952–958.
Nakamura T, Peng KW, Harvey M, Greiner S, Lorimer IA, James CD et al. Rescue and propagation of fully retargeted oncolytic measles viruses. Nat Biotechnol 2005; 23: 209–214.
Bucheit AD, Kumar S, Grote DM, Lin Y, von Messling V, Cattaneo RB et al. An oncolytic measles virus engineered to enter cells through the CD20 antigen. Mol Ther 2003; 7: 62–72.
Schmitt M, Pawlita M . High-throughput detection and multiplex identification of cell contaminations. Nucleic Acids Res 2009; 37: e119.
Duprex WP, McQuaid S, Hangartner L, Billeter MA, Rima BK . Observation of measles virus cell-to-cell spread in astrocytoma cells by using a green fluorescent protein-expressing recombinant virus. J Virol 1999; 73: 9568–9575.
Radecke F, Spielhofer P, Schneider H, Kaelin K, Huber M, Dotsch C et al. Rescue of measles viruses from cloned DNA. EMBO J 1995; 14: 5773–5784.
Calain P, Roux L . The rule of six, a basic feature for efficient replication of Sendai virus defective interfering RNA. J Virol 1993; 67: 4822–4830.
Ravindranath NM, Shuler C . Expression of complement restriction factors (CD46, CD55 & CD59) in head and neck squamous cell carcinomas. J Oral Pathol Med 2006; 35: 560–567.
Chung-Faye GA, Chen MJ, Green NK, Burton A, Anderson D, Mautner V et al. In vivo gene therapy for colon cancer using adenovirus-mediated, transfer of the fusion gene cytosine deaminase and uracil phosphoribosyltransferase. Gene Ther 2001; 8: 1547–1554.
Galanis E . Therapeutic potential of oncolytic measles virus: promises and challenges. Clin Pharmacol Ther 2010; 88: 620–625.
Rubin Grandis J, Chakraborty A, Melhem MF, Zeng Q, Tweardy DJ . Inhibition of epidermal growth factor receptor gene expression and function decreases proliferation of head and neck squamous carcinoma but not normal mucosal epithelial cells. Oncogene 1997; 15: 409–416.
Bernier J, Bentzen SM, Vermorken JB . Molecular therapy in head and neck oncology. Nat Rev Clin Oncol 2009; 6: 266–277.
Zhang SW, Xiao SW, Liu CQ, Sun Y, Su X, Li DM et al. [Treatment of head and neck squamous cell carcinoma by recombinant adenovirus-p53 combined with radiotherapy: a phase II clinical trial of 42 cases]. Zhonghua Yi Xue Za Zhi 2003; 83: 2023–2028.
Hu JC, Coffin RS, Davis CJ, Graham NJ, Groves N, Guest PJ et al. A phase I study of OncoVEXGM-CSF, a second-generation oncolytic herpes simplex virus expressing granulocyte macrophage colony-stimulating factor. Clin Cancer Res 2006; 12: 6737–6747.
Xu F, Li S, Li XL, Guo Y, Zou BY, Xu R et al. Phase I and biodistribution study of recombinant adenovirus vector-mediated herpes simplex virus thymidine kinase gene and ganciclovir administration in patients with head and neck cancer and other malignant tumors. Cancer Gene Ther 2009; 16: 723–730.
Garber K . China approves world's first oncolytic virus therapy for cancer treatment. J Natl Cancer Inst 2006; 98: 298–300.
Acknowledgements
We thank Jessica Albert and Stefanie Sawall for their excellent technical assistance. We thank Dr Roberto Cattaneo (Mayo Clinic) for continuous support of our work. We are grateful to Dr Christel C Herold-Mende (University Hospital Heidelberg) and Dr Daniel Herr (University Hospital Ulm, Germany) for providing the HNSCC and MCF-7 cell lines. We thank Dr Michaela Arndt (University Hospital Heidelberg) for the FACS analyses and the Light Microscopy Facility at the DKFZ including Manuela Brom and Felix Bestvater for their technical support. This work was supported by the German Cancer Aid grant 108828 (CS), and by the German Cancer Aid, Max Eder grant 108307 (GU).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Zaoui, K., Bossow, S., Grossardt, C. et al. Chemovirotherapy for head and neck squamous cell carcinoma with EGFR-targeted and CD/UPRT-armed oncolytic measles virus. Cancer Gene Ther 19, 181–191 (2012). https://doi.org/10.1038/cgt.2011.75
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cgt.2011.75
Keywords
This article is cited by
-
Synergism of rMV-Hu191 with cisplatin to treat gastric cancer by acid sphingomyelinase-mediated apoptosis requiring integrity of lipid raft microdomains
Gastric Cancer (2021)
-
Nucleic acid targeting: towards personalized therapy for head and neck cancer
Oncogene (2016)
-
An armed oncolytic measles vaccine virus eliminates human hepatoma cells independently of apoptosis
Gene Therapy (2013)
-
Chemovirotherapy of Malignant Melanoma with a Targeted and Armed Oncolytic Measles Virus
Journal of Investigative Dermatology (2013)