Abstract
The inhibitor of growth (ING) family proteins have been defined as candidate tumor suppressors. ING4 as a novel member of the ING family has potential tumor-suppressive effects. In this study, we explored the combined effect of adenovirus-mediated ING4 (Ad-ING4) gene transfer plus chemotherapy drug cisplatin (CDDP) on SMMC-7721 human hepatocarcinoma cells in vitro and in vivo, and its underlying mechanism. We demonstrated that Ad-ING4 plus CDDP induced synergistic growth inhibition, enhanced apoptosis, and had an additive effect on upregulation of Fas, Bax, Bak, cleaved Bid, cleaved caspase-8, caspase-9, caspase-3 and cleaved PARP, and on downregulation of Bcl-2 and Bcl-XL in SMMC-7721 hepatocarcinoma cells. Moreover, Ad-ING4 plus CDDP synergistically suppressed in vivo SMMC-7721 hepatocarcinoma subcutaneous (s.c.) xenografted tumor growth and reduced tumor vessel CD34 expression and microvessel density (MVD) in athymic nude mice. Most importantly, Ad-ING4 plus CDDP did not have overlapping toxicities in HL-7702 normal human liver cells and normal liver tissues of mice. The in vitro and in vivo enhanced antitumor effect elicited by Ad-ING4 plus CDDP was closely associated with the cooperative regulation of extrinsic and intrinsic apoptotic pathways and synergistic inhibition of tumor angiogenesis. Thus, our results indicate that Ad-ING4 plus CDDP is a potential combined treatment strategy for hepatocarcinoma.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common cancer in the world, and is the third highest cause of cancer-related mortality.1 The incidence is increasing worldwide because of the dissemination of hepatitis B and C virus infection.2, 3 Surgical resection is the mainstay of curative treatment for early HCC, but prognosis remains unsatisfactory because of frequent recurrence.4 Liver transplantation is another potentially curative treatment for HCC, but its application is limited by the shortage of grafts.5 For unresectable HCC, various locoregional therapies may be used to palliate symptoms and prolong survival.6 Furthermore, conventional chemotherapy has not been shown to be effective in HCC, and there is no proven effective systemic therapy for HCC patients with metastatic disease.7 Hence, the search for novel therapeutic modalities for HCC is of paramount importance.
Cancer gene therapy represents a new and promising therapeutic modality for cancers, which is based on the introduction of genetic material into cells to generate a curative biological effect. A variety of gene therapy-based anticancer strategies have been effective in animal tumor models, including replacement of tumor suppressor genes, selective activation of prodrugs, genetic immunotherapy and antiangiogenic actions. Inhibitor of growth 4 (ING4), a novel member of the ING tumor suppressor family, was first isolated and characterized by Shiseki et al.8 Recently, ING4 has attracted much attention as a strong candidate tumor suppressor that has an important role in oncogenesis, DNA repair, tumor growth, angiogenesis, migration and gene transcription regulation. ING4 has a functionally conserved plant homeodomain-finger motif in the COOH-terminal region involved in chromatin remodeling and subsequent gene transcriptional regulation by its interaction with histone acetyltransferase and histone deacetylase complexes.9, 10, 11 It also has a potential bipartite nuclear localization signal domain in the middle region, which is essential for nuclear localization of ING4 and its binding and functional interaction with p53.12 Previous studies showed that ING4 was dramatically downregulated in glioblastoma,13 head and neck carcinoma,14 HCC,15 melanoma16, 17 and gastric carcinoma,18 which was closely associated with tumor grade, metastasis and prognosis. ING4 can significantly inhibit tumor cell growth and induce cell cycle alteration and apoptosis in different tumor types8, 13, 16, 17, 19, 20, 21, 22 such as colorectal, glioblastoma, melanoma, hepatocellular, myeloma, lung and pancreatic carcinomas, and enhance chemosensitivity to doxorubicin and etoposide in HepG2 hepatocarcinoma cells.19 ING4 can also suppress the activity of NF-κB and HIF-1α, leading to inhibition of tumor angiogenesis.13, 20 In addition, ING4 can suppress the loss-of-contact inhibition elicited by MYCN or MYC.23 More recently, it has been reported that ING4 can exhibit a marked inhibitory effect on tumor cell spreading, migration and invasion.16, 21, 24 Therefore, ING4 is a potent tumor suppressor that exerts its tumor-suppressive effect via multiple pathways in a variety of tumors.
Chemotherapy is one of the most conventional therapeutic strategies for human cancers. Conventional chemotherapy drugs include cisplatin, also named cis-diamminedichloroplatinum (CDDP), adriamycin and 5-fluorouracil. CDDP is deemed to be the ‘penicillin of cancer drugs’ because of its universal, early and effective treatment for many cancers.25 Unlike many anticancer drugs, CDDP is an inorganic molecule with a simple structure that is often used as an attractive chemotherapy drug and broadly used for the treatment of various forms of malignant tumors. Although the mechanism has not yet been fully understood, CDDP is generally believed to kill cancer cells by binding to DNA and interfering with the cell’s repair mechanism, which eventually leads to cell death.26 Despite these merits, severe toxic side effects and drug resistance that limit its efficacy are major clinical obstacles associated with CDDP-based chemotherapy.27, 28 Thus, it is urgent to explore novel approaches to reduce drug dosage, minimize side effects and enhance therapeutic efficacy to promote the application of CDDP in cancer chemotherapy.
Combination therapy with multiple drugs or modalities such as the combined treatment of gene therapy and conventional chemotherapy (chemo-gene therapy) or radiotherapy is a common practice in the treatment of cancers, which can achieve greater therapeutic benefit and reduce the side effects and resistance to drugs.29, 30 Interestingly, the tumor suppressor ING4 can sensitize HepG2 hepatocarcinoma cells to DNA-damaging agents such as doxorubicin and etoposide,19 suggesting that it may be used as a chemosensitive modulator in the combination therapy with chemotherapy drugs for cancers. Therefore, we hypothesized that a combination of adenovirus-mediated ING4 (Ad-ING4) gene transfer and chemotherapy drug CDDP would exhibit an enhanced antitumor activity for human cancers. To date, the therapeutic effect of the conjugation of Ad-ING4 with CDDP on human cancers has not been reported. To enhance the therapeutic efficacy and develop a novel combination therapeutic modality for HCC, in this study, we investigated the potential combined effect of Ad-ING4 plus CDDP against SMMC-7721 human hepatocarcinoma cells in vitro and in vivo in an athymic nude mouse model, and also elucidated its underlying molecular mechanism.
Materials and methods
Adenoviruses, cell lines, reagents and mice
The Ad-ING4 and Ad-green fluorescent protein (GFP) replication-incompetent Ad5E1- and E3-deleted adenoviruses were constructed in our laboratory,21 Cell and Molecular Biology Institute, College of Medicine, Soochow University (Suzhou, China). The QBI-293A human embryonic kidney cell line was kindly provided by Prof. Jiang Zhong, Fudan University (Shanghai, China). The SMMC-7721 and HepG2 human hepatocarcinoma cell lines and HL-7702 normal human liver cells were purchased from the American Type Culture Collection (ATCC) (Shanghai, China). The QBI-293A, SMMC-7721, HepG2 and HL-7702 cells were cultured in RPMI1640 (GIBCO, Shanghai, China) supplemented with 10% fetal bovine serum (Hyclone, Shanghai, China), respectively. Trizol was purchased from Invitrogen (Shanghai, China). The reverse transcriptase polymerase MuMLV was purchased from MBI (Shanghai, China). The polyclonal goat anti-ING4 antibody was purchased from Abcam (Shanghai, China). The CDDP was kindly provided by Dr Yehan Zhu, the first hospital affiliated to Soochow University (Suzhou, China). The 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) kit was purchased from Sigma (Shanghai, China). The Annexin V-PE/7-AAD apoptosis detection kit was purchased from BD Biosciences (Shanghai, China). The antibodies specific for Fas, Bcl-2, Bcl-XL, Bax, Bak, β-actin and CD34 were purchased from Santa Cruz (Shanghai, China). The antibodies specific for Bid, caspase-3, caspase-8, caspase-9 and PARP were purchased from Cell Signaling (Shanghai, China). The SuperEnhanced chemiluminescence detection kit was purchased from Applygen Technologies Inc. (Beijing, China). The UltraSensitiveTM SP kit was purchased from Maixin (Fuzhou, China). The mouse alanine aminotransferase (ALT) and aspartate aminotransferase (AST) enzyme-linked immunosorbent assay (ELISA) kits were purchased from Uscn Life Science (Wuhan, China). The female athymic nude mice were purchased from Shanghai Experimental Animal Center (Shanghai, China) and maintained in the animal facility at Soochow University according to the animal research committee's guidelines of Soochow University.
Analysis of adenoviral infection efficiency and ING4 transgene expression
The recombinant replication-incompetent Ad5E1- and E3-deleted adenovirus with two independent cytomegalovirus promoters driving ING4 and GFP expression, Ad-ING4 and its control adenovirus Ad-GFP expressing GFP under the control of cytomegalovirus promoter were prepared as described previously.21 The titer of Ad-ING4 and Ad-GFP adenoviruses was determined using the gene transfer unit (GTU) method by calculating the number of the reporter gene GFP-expressing QBI-293A cells under fluorescence microscopy within 18 h after adenoviral infection. To assess the optimal ratio of infectious adenovirus (GTU) to target cells, called multiplicity of infection (MOI), for a maximal infection and transgene expression in SMMC-7721, HepG2 and HL-7702 cells, the SMMC-7721 and HepG2 human hepatocarcinoma cells and HL-7702 normal human liver cells were infected with Ad-GFP and Ad-ING4 at various MOIs (0, 1, 10, 25, 50, 100 and 200), respectively. The adenoviral infection efficiency was examined according to GFP expression by fluorescence microscopy. Furthermore, the ING4 transgene expression mediated by adenoviral infection in SMMC-7721 and HepG2 human hepatocarcinoma cells and HL-7702 normal human liver cells was determined by reverse transcriptase-PCR and western blot analysis. Total cellular RNAs were extracted from Ad-ING4- or Ad-GFP-infected and uninfected SMMC-7721, HepG2 and HL-7702 cells using Trizol, and first-strand complementry DNA was reversely transcribed with RNA as template and oligo d(T)18 as primer. The PCR reaction was carried out using complementry DNA as template and ING4-F (5′-GCGTCGACATGGATGATGGGATGTATTTGGAAC-3′) and ING4-R (5′-GCAAGCTTCTATTTCTTCTTCCGTTCTTGGGAG-3′) as primers under the conditions 1 cycle at 94 °C (2 min) and then 72 °C (10 min) followed by 35 cycles at 94 °C (50 s), 58 °C (50 s) and 72 °C (55 s). All PCR reaction products were analyzed on 1% agarose gel electrophoresis with ethidium bromide staining. Total cellular lysates derived from Ad-ING4 or Ad-GFP-infected and uninfected SMMC-7721, HepG2 and HL-7702 cells were resolved by 12% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and subsequently transferred onto a polyvinylidene difluoride membrane. The membrane was blocked by incubation with 5% (w/v) non-fat dry milk in Tris-buffered saline containing 0.05% Tween 20 (TBST) for 1 h at 37 °C. For western blot analysis, the membrane was incubated with primary antibody polyclonal goat anti-ING4 (1:1000) in blocking solution for 1 h at 37 °C. The membrane was washed with TBST and incubated with peroxidase horseradish peroxidase-conjugated secondary antibody rabbit anti-goat IgG (1:3000) in blocking solution for another 1 h at 37 °C. The membrane was then washed and developed by use of a SuperEnhanced chemiluminescence detection kit. The protein bands were visualized after exposure of the membranes to Kodak X-ray film.
Cell viability assay
To assess the cytotoxic effect of Ad-ING4 or CDDP alone on SMMC-7721, HepG2 and HL-7702 cells, the SMMC-7721 and HepG2 human hepatocarcinoma cells and HL-7702 normal human liver cells were dispensed in a 96-well culture plate at a density of 1 × 104 cells per well, respectively, and incubated at 37 °C. After 24-h incubation, the SMMC-7721, HepG2 and HL-7702 cells were treated with Ad-ING4 at the optimal MOIs, 50 (SMMC-7721), 25 (HepG2) and 25 (HL-7702), or various doses of CDDP (0.75, 1.5, 3, 6 or 12 μg ml−1) for 3 days, respectively. The medium containing Ad-GFP was used as a blank adenovirus control, whereas the medium containing phosphate-buffered saline (PBS) without Ad-ING4, Ad-GFP or CDDP was used as a cell control (PBS control). At 3 days after treatment, the SMMC-7721, HepG2 and HL-7702 cells were incubated with 10 μl MTT (5 mg ml−1) for 4 h at 37 °C. The formazan crystals in the cells were solubilized with stop solution and the plate was then read at 570 nm using a Microplate Reader Model 550 (BIO-RAD, Shanghai, China). To further determine the combined effect of Ad-ING4 and CDDP on hepatocarcinoma cells, the SMMC-7721 hepatocarcinoma cells, a relatively non-sensitive hepatocarcinoma cell line to chemotherapy drug CDDP, and an optimal dose of 1.5 μg ml−1 of CDDP were employed in the in vitro combination therapy studies. Briefly, the SMMC-7721 human hepatocarcinoma cells were dispensed in a 96-well culture plate at a density of 1 × 104 cells per well and incubated at 37 °C. After 24-h incubation, the SMMC-7721 hepatocarcinoma cells were treated with Ad-ING4 (50 MOI), Ad-GFP (50 MOI) or CDDP (1.5 μg ml−1) alone, Ad-ING4 (50 MOI) plus CDDP (1.5 μg ml−1), or Ad-GFP (50 MOI) plus CDDP (1.5 μg ml−1) for the indicated time periods (0–4 days). The medium containing PBS without Ad-ING4, Ad-GFP, CDDP, Ad-ING4 plus CDDP, or Ad-GFP plus CDDP was used as a cell control (PBS control). To investigate whether Ad-ING4 combined with CDDP exhibits overlapping inhibitory effect on normal liver cells, the HL-7702 normal human liver cells were used as a normal liver cell control by treatment with Ad-ING4 (25 MOI), Ad-GFP (25 MOI) or CDDP (1.5 μg ml−1) alone, Ad-ING4 (25 MOI) plus CDDP (1.5 μg ml−1), Ad-GFP (25 MOI) plus CDDP (1.5 μg ml−1), or PBS. Before treatment and at different time points after treatment, the viability of HL-7702 normal liver cells was assessed by MTT assay as described above.
Flow-cytometric analysis of apoptosis
Ad-ING4 plus CDDP-induced apoptosis in SMMC-7721 human hepatocarcinoma cells was assessed by flow cytometric analysis using Annexin V-PE/7-AAD double staining following the manufacturer's instructions. Briefly, the SMMC-7721 tumor cells (1 × 106) were treated with Ad-ING4 (50 MOI), Ad-GFP (50 MOI) or CDDP (1.5 μg ml−1) alone, Ad-ING4 (50 MOI) plus CDDP (1.5 μg ml−1), or Ad-GFP (50 MOI) plus CDDP (1.5 μg ml−1). The medium containing PBS without Ad-ING4, Ad-GFP, CDDP, Ad-ING4 plus CDDP, or Ad-GFP plus CDDP was used as a cell control (PBS control). After 24 h, the treated and untreated SMMC-7721 tumor cells were collected and washed with cold PBS, respectively. Then the cells (1 × 105) were suspended in 100 μl of 1 × binding buffer and incubated with 5 μl Annexin V-PE and 5 μl 7-AAD at room temperature. After 15-min incubation, 400 μl of 1 × binding buffer was added and the apoptotic cells were analyzed by flow cytometry.
Western blot analysis
The SMMC-7721 human hepatocarcinoma cells were treated with Ad-ING4 (50 MOI), Ad-GFP (50 MOI) or CDDP (1.5 μg ml−1) alone, Ad-ING4 (50 MOI) plus CDDP (1.5 μg ml−1) or Ad-GFP (50 MOI) plus CDDP (1.5 μg ml−1). The medium containing PBS without Ad-ING4, Ad-GFP, CDDP, Ad-ING4 plus CDDP or Ad-GFP plus CDDP was used as a cell control (PBS control). After 24-h treatment, the treated and untreated SMMC-7721 tumor cells were collected, washed with cold PBS and lysed in lysis buffer (1 × 107 cells per 1 ml lysis buffer). Total cellular proteins were extracted and the protein concentration was determined by BCA protein assay using a spectrophotometer. To elucidate the molecular mechanism involved in Ad-ING4 plus CDDP-induced enhancement of growth inhibition and apoptosis in SMMC-7721 hepatocarcinoma cells, the cellular lysates containing 100 μg of total protein were subjected to western blot analysis as described above using primary antibodies specific for Fas, caspase-8, Bid, Bcl-2, Bcl-XL, Bax, Bak, caspase-9, caspase-3 and PARP, respectively.
Animal studies
Female athymic nude mice were subcutaneously (s.c.) inoculated on the armpits of their right anterior limbs with 2 × 106 SMMC-7721 human hepatocarcinoma cells, and then monitored daily for tumor growth. Tumor volume was measured with a caliper and calculated by the formula, tumor size=ab2/2, where a is the larger and b is the smaller of the two dimensions. When the tumors grew up to a mean tumor volume of around 0.2–0.3 cm3, SMMC-7721 human hepatocarcinoma s.c. xenografted tumor-bearing mice were subjected to in vivo CDDP-dose-finding study and Ad-ING4 plus CDDP combination treatment, respectively. In the CDDP-dose study, tumor-bearing mice (three mice each group) were intraperitoneally (i.p.) injected with various doses of CDDP (1, 3, 5 or 10 mg kg−1 body weight) or PBS every other day for a total of five times. Tumor volume and body weight were monitored over time. According to the preliminary CDDP-dose pilot study, an optimal dose of 1 mg kg−1 of CDDP was selected for the subsequent Ad-ING4 plus CDDP in vivo combination treatment. In the in vivo combination treatment, tumor-bearing mice were randomly divided into six groups (six mice each group) and intratumorally injected with Ad-ING4 (1 × 108 GTU), Ad-GFP (1 × 108 GTU) or PBS alone, or i.p. injected with CDDP (1 mg kg−1) alone or plus Ad-ING4 (1 × 108 GTU) or Ad-GFP (1 × 108 GTU) by intratumoral injection every other day for a total of five times, respectively. Tumor progression and body weight were monitored daily. In addition, the tumor-bearing mice were killed 3 weeks after single or combination treatment, and the SMMC-7721 hepatocarcinoma s.c. xenografted tumors and normal liver tissues of mice were removed, weighted, fixed by 10% neutral formalin and embedded in paraffin for hematoxylin and eosin staining and immunohistochemistry analysis, respectively. On the day of euthanization, blood samples were also collected by tail veil breeding for measurement of liver serum enzymes such as ALT and AST by ELISA using mouse ALT and AST ELISA kits according to the manufacturer’s instructions.
CD34 immunostaining and microvessel density (MVD) counting
The expression of CD34 in SMMC-7721 human hepatocarcinoma xenografted tumors was tested by immunohistochemistry analysis using an UltraSensitiveTM SP kit. The presence of buffy or brown diaminobenzidine precipitates is indicative of positive reactivity for CD34. MVD, detected by immunostaining for CD34, was determined as previously described by Weidner et al.31 Any endothelial cell cluster immunoreactive for CD34 clearly separated from adjacent microvessels was considered as a single countable vessel. Each value represents the number of vessels counted at a high-power view ( × 400) by microscopy. The mean value represents the average number derived from five high-power fields of each case.
Calculation of synergistic indexes
The interactive effects of Ad-ING4 and CDDP were evaluated by combination index (CI) calculated by the formula as described previously,32 CI=FuAFuB/Fu(A+B), where FuA represents the fraction unaffected by Ad-ING4 alone compared with the untreated control group, FuB represents the fraction unaffected by CDDP alone, and Fu(A+B) represents the fraction unaffected by Ad-ING4 plus CDDP. A value of CI >1 indicates a synergistic effect between Ad-ING4 and CDDP, and CI <1 indicates a less than additive effect.
Statistical analysis
All data are presented as the mean±s.d. The significance of the difference between groups was evaluated by one-way and two-way repeated-measures analysis of variance (ANOVA), multiple comparisons and Student's t test with SPSS 10.0 software. A value of P<0.05 was considered statistically significant.
Results
Ad-ING4 transgene expression
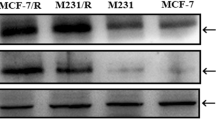
To determine the optimal MOI for a maximal infection and transgene expression, the SMMC-7721 and HepG2 hepatocarcinoma cells and HL-7702 normal liver cells were infected with Ad-GFP and Ad-ING4 at various MOIs (0, 1, 10, 25, 50, 100 and 200), respectively, and examined by fluorescence microscopy. More than 90% of GFP expression was found in the Ad-GFP- or Ad-ING4-infected SMMC-7721, HepG2 and HL-7702 cells at MOIs of 50, 25 and 25 or above, respectively, whereas the GFP expression was not found in the uninfected SMMC-7721, HepG2 and HL-7702 control cells (data not shown). Therefore, we selected an MOI of 50, 25 and 25, respectively, as an optimal dose for adenoviral infection of SMMC-7721, HepG2 and HL-7702 cells in the following experiments. To assess Ad-ING4 transgene expression, the total cellular RNAs and lysates extracted from Ad-ING4- or Ad-GFP-infected and uninfected SMMC-7721, HepG2 and HL-7702 cells were subjected to reverse transcriptase-PCR and western blot analysis. As shown in Figure 1, a significant amount of ING4 expression was found in the Ad-ING4-infected SMMC-7721, HepG2 and HL-7702 cells, but not in the Ad-GFP-infected and uninfected SMMC-7721, HepG2 and HL-7702 control cells, indicating that transgene ING4 mediated by adenovirus is expressed in Ad-ING4-infected SMMC-7721, HepG2 and HL-7702 cells at both the transcriptional and translational levels. In addition, chemotherapy with CDDP did not affect adenoviral infection and Ad-ING4 expression in the combination treatment (data not shown).
Transgene ING4 expression in Ad-ING4-infected SMMC-7721, HepG2 and HL-7702 cells. (a) Ad-ING4 transcriptional expression by reverse transcriptase-PCR analysis. Total cellular RNAs were obtained from Ad-ING4-infected SMMC-7721 and HepG2 hepatocarcinoma cells and HL-7702 normal liver cells, Ad-GFP-infected SMMC-7721, HepG2 and HL-7702 cells served as a blank adenovirus control, or uninfected SMMC-7721, HepG2 and HL-7702 control cells, respectively. The first-strand complementry DNA was synthesized from RNAs using reverse transcriptase; PCRs were conducted using primer sets specific for ING4 and housekeep gene β-actin used as an internal control. (b) Ad-ING4 translational expression by western blot analysis. Total cellular lysates of Ad-ING4- or Ad-GFP-infected SMMC-7721, HepG2 and HL-7702 cells and uninfected control cells were analyzed by immunoblotting with anti-ING4 and anti-β-actin (an internal control) antibody, respectively. Data shown are representative of three independent experiments.
Ad-ING4 or CDDP alone inhibits in vitro hepatocarcinoma cell growth
Before initiating the experiment involving a combination of Ad-ING4 and CDDP, we assessed the effect of Ad-ING4 or CDDP alone on the viability of SMMC-7721 and HepG2 hepatocarcinoma cells and HL-7702 normal liver cells, respectively. The SMMC-7721, HepG2 and HL-7702 cells were treated with Ad-ING4 at the optimal MOIs of 50, 25 and 25, respectively, or various doses of CDDP (0.75, 1.5, 3, 6 or 12 μg ml−1), and the cell growth was examined at day 3 after treatment using MTT assay. As shown in Figure 2a, Ad-ING4 treatment significantly inhibited SMMC-7721 hepatocarcinoma cell growth (35% reduction compared with viability of control cells), whereas it moderately inhibited HepG2 hepatocarcinoma cell growth (21% reduction), compared with the Ad-GFP- and PBS-treated control group (P<0.05). However, Ad-ING4 had minimal effect on HL-7702 normal liver cells (7% reduction). These results indicated that ING4 transgene overexpression exerts selective killing activity for tumor cells such as hepatocarcinoma cells. Treatment of SMMC-7721 and HepG2 hepatocarcinoma cells and HL-7702 normal liver cells with various concentrations of CDDP resulted in a dose-dependent reduction in the number of viable cells (Figure 2b). Furthermore, SMMC-7721 and HepG2 hepatocarcinoma cells and HL-7702 normal liver cells are different in their sensitivity to chemotherapy drug CDDP. The moderate reduction in SMMC-7721 hepatocarcinoma cell viability was observed at 1.5 μg ml−1 of CDDP (19% reduction), and significant reduction was observed starting at 3 μg ml−1 (37% reduction), with maximum reduction observed at 12 μg ml−1 (69% reduction). Unexpectedly, the significant reduction in HepG2 hepatocarcinoma cell viability was observed starting at the lowest concentration of CDDP (0.75 μg ml−1) (49% reduction), with maximum reduction observed at 12 μg ml−1 (89% reduction). However, the significant reduction in HL-7702 normal liver cell viability was observed at 6 (29% reduction) and 12 μg ml−1 (47% reduction), with slight reduction observed at 3 μg ml−1 (14% reduction). These results indicated that HepG2 hepatocarcinoma cells are much more sensitive to chemotherapy drug CDDP than SMMC-7721 hepatocarcinoma cells, and only a higher concentration of CDDP ranging from 6 to 12 μg ml−1 exhibits significant cytotoxic effect on HL-7702 normal liver cells. Therefore, we selected the relatively non-sensitive hepatocarcinoma cell line to CDDP, SMMC-7721 and the optimal dose of 1.5 μg ml−1 of CDDP in the in vitro combination treatment to minimize toxicity to normal cells and elicit only modest antitumor activity when used as single therapy, while leaving a window for observation of the additive or synergistic effects of Ad-ING4 plus CDDP combination therapy.
Ad-ING4 or CDDP alone suppresses in vitro hepatocarcinoma cell growth. (a) The cytotoxic effect of Ad-ING4 on SMMC-7721 and HepG2 hepatocarcinoma cells and HL-7702 normal liver cells. The SMMC-7721, HepG2 and HL-7702 cells were treated with Ad-ING4 at MOI of 50, 25 and 25 or with Ad-GFP blank adenovirus or PBS served as controls for 3 days, respectively. The survival cells were evaluated at day 3 point after treatment by using MTT assay. The in vitro growth of SMMC-7721 and HepG2 tumor cells treated with Ad-ING4 was significantly or moderately inhibited after infection, whereas Ad-ING4 had minimal effect on HL-7702 normal liver cells (*P<0.05, compared with Ad-GFP and PBS group, one-way repeated measures ANOVA and multiple comparisons, n=4 replicates per condition). (b) The cytotoxic effect of CDDP on SMMC-7721 and HepG2 hepatocarcinoma cells and HL-7702 normal liver cells. The SMMC-7721, HepG2 and HL-7702 cells were treated with various doses of CDDP (0.75, 1.5, 3, 6 or 12 μg ml−1) for 3 days, respectively. The survival cells were evaluated at day 3 point after treatment by using MTT assay. CDDP inhibits in vitro growth of SMMC-7721 and HepG2 hepatocarcinoma cells and HL-7702 normal liver cells in a dose-dependent manner (*P<0.05, compared with PBS group, Student t test, n=4 replicates per condition). Data shown are representative of three independent experiments.
Ad-ING4 plus CDDP synergistically suppresses in vitro and in vivo SMMC-7721 hepatocarcinoma cell growth
To investigate whether Ad-ING4 plus CDDP elicits enhanced cytotoxicity to hepatocarcinoma cells in vitro, the SMMC-7721 human hepotacarcinoma cells were cultured in the presence of Ad-ING4 (50 MOI), Ad-GFP (50 MOI) or CDDP (1.5 μg ml−1) alone, Ad-ING4 (50 MOI) plus CDDP (1.5 μg ml−1), or Ad-GFP (50 MOI) plus CDDP (1.5 μg ml−1). The tumor cell viability was examined daily for 4 days using MTT assay. As shown in Figure 3a, Ad-ING4 plus CDDP combination treatment synergistically inhibited in vitro SMMC-7721 hepatocarcinoma cell growth in a time-dependent manner, compared with single Ad-ING4- and CDDP-treated group (P<0.05; CI>1), whereas the phenomenon did not occur in the Ad-GFP plus CDDP combination treatment, indicating that it is Ad-ING4 expression that contributes to the combined suppressive effect on SMMC-7721 hepatocarcinoma cells. Moreover, Ad-ING4 plus CDDP exhibited minimal cytotoxic effect on HL-7702 normal liver cells, equal to that of CDDP (Figure 3a). The result further indicated that Ad-ING4 plus CDDP combination treatment selectively exerts synergistic antitumor activity in SMMC-7721 hepatocarcinoma cells but not in HL-7702 normal liver cells. To determine the optimal dose of CDDP employed in vivo in an athymic nude mouse animal model combination treatment, a dose-finding study was performed in which SMMC-7721 human hepatocarcinoma s.c. xenografted tumor-bearing mice (three mice each group) were treated with a range of CDDPs (1, 3, 5 or 10 mg kg−1) by i.p. injection. Tumor volume and body weight were monitored over time. Mice treated with higher doses of CDDP (5 or 10 mg kg−1) resulted in a significant loss of body weight and had to be euthanized within a week, whereas those treated with 1 or 3 mg kg−1 of CDDP showed no significant body weight losses with only minimal toxicity (data not shown). Compared with the PBS-treated control group, tumor progression was significantly retarded in the mice treated with 3 mg kg−1 of CDDP, but moderately retarded in those treated with 1 mg kg−1 of CDDP (date not shown). Therefore, an optimal dose of 1 mg kg−1 of CDDP was selected for the Ad-ING4 plus CDDP in vivo combination treatment. To further explore whether the combination of Ad-ING4 with CDDP would result in in vivo-enhanced antitumor effect, the athymic nude mice (six mice each group) bearing SMMC-7721 human hepatocarcinoma s.c. xenografted tumors were intratumorally injected with Ad-ING4 (1 × 108 GTU), Ad-GFP (1 × 108 GTU) or PBS alone, or i.p. injected with CDDP (1 mg kg−1) alone or plus Ad-ING4 (1 × 108 GTU) or Ad-GFP (1 × 108 GTU) by intratumoral injection every other day for a total of five times. The tumor growth in vivo was monitored daily and tumor volume and weight were measured. As shown in Figure 3b, the tumor growth was more significantly retarded in the Ad-ING4 plus CDDP group, compared with the single Ad-ING4- and CDDP-treated group (P<0.05; CI>1), indicating that Ad-ING4 plus CDDP combination treatment also remarkably suppresses in vivo SMMC-7721 hepatocarcinoma s.c. xenografted tumor growth in an athymic nude mouse model with synergistic effect. To assess Ad-ING4 plus CDDP-mediated in vivo toxicity, body and liver weight were investigated. As shown in Figures 3c and d, there was no difference in body and liver weight among various groups. Histological sections of liver in different groups also showed no significant hepatic damage (data not shown). In addition, ELISA analysis of liver serum enzymes (Figure 3e) showed a slight increase in ALT and AST elicited by CDDP, but no additive effect in the Ad-ING4 plus CDDP group. These results indicated that the combination of Ad-ING4 and CDDP also exhibits minimal toxicity in vivo without overlapping effect.
Ad-ING4 plus CDDP elicits synergistic antitumor activity for SMMC-7721 hepatocarcinoma cells without overlapping toxicity. (a) The in vitro combined effect of Ad-ING4 plus CDDP on SMMC-7721 hepatocarcinoma cells or HL-7702 normal liver cells. The SMMC-7721 hepatocarcinoma cells and HL-7702 normal liver cells were treated with Ad-ING4 (50, 25 MOI), Ad-GFP (50, 25 MOI) or CDDP (1.5 μg ml−1) alone, Ad-ING4 (50, 25 MOI) plus CDDP (1.5 μg ml−1), Ad-GFP (50, 25 MOI) plus CDDP (1.5 μg ml−1), or PBS for the indicated time periods (0–4 days), respectively. The survival cells were evaluated at day 0, 1, 2, 3 and 4 point after treatment by using MTT assays. Ad-ING4 plus CDDP combination treatment synergistically inhibited in vitro SMMC-7721 hepatocarcinoma cell growth in a time-dependent manner (*P<0.05, compared with Ad-GFP and PBS group at day 1, 2, 3 and 4 after treatment, respectively, two-way repeated measures ANOVA and multiple comparisons, n=4 replicates per condition; # CI in the Ad-ING4 plus CDDP combination treatment >1). In addition, Ad-ING4 plus CDDP exhibited minimal cytotoxic effect on in vitro HL-7702 normal liver cells equal to that of CDDP. (b) The in vivo synergistic antitumor effect on SMMC-7721 hepatocarcinoma s.c. xenografted tumors by combining Ad-ING4 with CDDP. The athymic nude mice (six mice each group) bearing SMMC-7721 hepatocarcinoma s.c. xenografted tumors were intratumorally injected with Ad-ING4 (1 × 108 GTU), Ad-GFP (1 × 108 GTU) or PBS alone, or i.p. injected with CDDP (1 mg kg−1) alone or plus Ad-ING4 (1 × 108 GTU) or Ad-GFP (1 × 108 GTU) by intratumoral injection every other day for a total of five times. The SMMC-7721 hepatocarcinoma s.c. xenografted tumor volume was measured before and after treatment. Furthermore, the xenografted tumors were removed 3 weeks after treatment and tumor weight was measured. Ad-ING4 plus CDDP combination treatment also synergistically suppressed in vivo SMMC-7721 hepatocarcinoma s.c. xenografted tumor growth in an athymic nude mouse model (tumor weight, *P<0.05, compared with Ad-GFP and PBS group, one-way repeated measures ANOVA and multiple comparisons, n=6 mice per condition, and tumor volume, *P<0.05, compared with Ad-GFP and PBS group at week 1, 2 and 3 after treatment, respectively, two-way repeated-measures ANOVA and multiple comparisons, n=6 mice per condition; #CI in the Ad-ING4 plus CDDP combination treatment > 1). (c, d, e) Ad-ING4 plus CDDP-induced in vivo toxicity. On the day of the killing mice, body weight (c) and liver weight (d) of mice were measured, and blood samples were collected and the amounts of ALT and AST liver serum enzymes in serum (e) were assessed by ELISA. There was only a slight increase in ALT and AST derived from CDDP-induced in vivo toxicity (*P<0.05, compared with PBS group, Student t test, n=6 mice per condition, n=3 replicates per sample) without overlapping effect in Ad-ING4 plus CDDP group. Data shown are representative of three independent experiments.
Ad-ING4 plus CDDP enhances apoptosis in SMMC-7721 hepatocarcinoma cells
To examine whether Ad-ING4 plus CDDP combination treatment elicits enhanced apoptosis in hepatocarcinoma cells, the SMMC-7721 human hepatocarcinoma cells were treated with Ad-ING4 (50 MOI), Ad-GFP (50 MOI) or CDDP (1.5 μg ml−1) alone, Ad-ING4 (50 MOI) plus CDDP (1.5 μg ml−1), or Ad-GFP (50 MOI) plus CDDP (1.5 μg ml−1) for 24 h and harvested for staining with Annexin V-PE (early apoptotic marker) and 7-AAD (late apoptotic marker), and the apoptosis of SMMC-7721 tumor cells was then analyzed by flow cytometry. As shown in Figure 4a, Ad-ING4 plus CDDP combination treatment resulted in 32.8% Annexin V single-positive cells, indicating that these SMMC-7721 hepatocarcinoma cells are in early stage of apoptosis, whereas there was 1.9, 2.6, 17.5, 10.2 and 11.9% early apoptotic cells occurring in SMMC-7721 tumor cells grown in the medium with PBS, Ad-GFP, Ad-ING4, CDDP and Ad-GFP plus CDDP, respectively. Compared with the single Ad-ING4- and CDDP-treated group, the combination of Ad-ING4 with CDDP more efficiently induces SMMC-7721 hepatocarcinoma cell apoptosis with synergistic effect (P<0.05; CI>1), which closely correlates with the Ad-ING4 plus CDDP-mediated in vitro and in vivo synergistic growth inhibition of SMMC-7721 hepatocarcinoma cells.
Ad-ING4 plus CDDP enhances apoptosis by cooperatively regulating extrinsic and intrinsic apoptotic pathways. The SMMC-7721 hepatocarcinoma cells were treated with Ad-ING4 (50 MOI), Ad-GFP (50 MOI) or CDDP (1.5 μg ml−1) alone, Ad-ING4 (50 MOI) plus CDDP (1.5 μg ml−1), Ad-GFP (50 MOI) plus CDDP (1.5 μg ml−1), or PBS for 24 h, then the apoptotic cells and expression of apoptosis-related proteins in SMMC-7721 tumor cells were assessed by flow cytometric and western blot analysis, respectively. (a) Ad-ING4 plus CDDP enhances apoptosis in SMMC-7721 hepatocarcinoma cells. The apoptotic cells were analyzed using Annexin V-PE/7-AAD double staining by flow cytometry. The Annexin V single-positive cells (early apoptotic cells) in the total cell population represented apoptotic cells. Ad-ING4 plus CDDP enhanced apoptosis in SMMC-7721 tumor cells with synergistic effect (*P<0.05, compared with Ad-GFP and PBS group, one-way repeated measures ANOVA and multiple comparisons, n=3 replicates per condition; #CI in the Ad-ING4 plus CDDP combination treatment >1). (b) Ad-ING4 plus CDDP cooperatively regulates extrinsic and intrinsic apoptotic pathways. Total cellular lysates of treated and untreated SMMC-7721 tumor cells were analyzed by immunoblotting with a panel of antibodies specific for Fas, Caspase-8, Bid, Bcl-2, Bcl-XL, Bax, Bak, Caspase-9, Caspase-3, PARP and β-actin (an internal control). The quantities of protein expression were normalized to the internal control β-actin measured in the same samples. Ad-ING4 plus CDDP combination treatment elicited an additive effect on the altered expression of apoptosis-related proteins such as Fas, Caspase-8, Bid, Bcl-2, Bcl-XL, Bax, Bak, Caspase-9, Caspase-3 and PARP. Data shown are representative of three independent experiments.
Ad-ING4 plus CDDP cooperatively regulates extrinsic and intrinsic apoptotic pathways
To further address the underlying molecular mechanism by which Ad-ING4 plus CDDP combination treatment results in enhanced antitumor effect, the expression of apoptosis-related proteins such as Fas, caspase-8, Bid, Bcl-2, Bcl-XL, Bax, Bak, caspase-9, caspase-3 and PARP in SMMC-7721 human hepatocarcinoma cells with different treatments was determined by western blot analysis. As shown in Figure 4b, the expression of Fas, Bax and Bak in Ad-ING4, CDDP, Ad-GFP plus CDDP, and Ad-ING4 plus CDDP group was significantly increased, whereas the expression of Bcl-2 and Bcl-XL was decreased, compared with the Ad-GFP and PBS control group. The activation of caspase-8, Bid, caspase-9, caspase-3 and PARP was also found in Ad-ING4, CDDP, Ad-GFP plus CDDP, and Ad-ING4 plus CDDP groups, but not in the Ad-GFP and PBS control group. Moreover, Ad-ING4 plus CDDP combination treatment elicited an additive effect on the altered expression of apoptosis-related proteins involved in the activation of extrinsic and intrinsic apoptotic pathways, indicating that Ad-ING4 plus CDDP synergistically suppresses SMMC-7721 hepatocarcinoma cell growth and induces apoptosis closely associated with the cooperative regulation of extrinsic and intrinsic apoptotic pathways.
Ad-ING4 plus CDDP synergistically reduces tumor vessel CD34 expression and MVD
The positive expression of CD34 was mainly represented as brownish yellow or brownish granules in vascular endothelial cells. In all SMMC-7721 human hepatocarcinoma s.c. xenografted tumors collected, the CD34 expression of tumor vascular endothelial cells in the Ad-ING4 plus CDDP combination treatment group was weaker or less, compared with the single Ad-ING4- and CDDP-treated group (Figure 5a), indicating that Ad-ING4 plus CDDP additively or synergistically downregulates CD34 expression of SMMC-7721 human hepatocarcinoma xenografted tumor vessels. Furthermore, the MVD (Figure 5b) counted in the Ad-ING4 plus CDDP group was significantly lesser than that in the single Ad-ING4- and CDDP-treated group (P<0.05; CI>1), indicating that Ad-ING4 plus CDDP has an synergistic effect on reduction of MVD in SMMC-7721 hepatocarcinoma s.c. xenografted tumors, which may be another important mechanism responsible for the Ad-ING4 plus CDDP-mediated in vivo synergistic growth inhibition of SMMC-7721 hepatocarcinoma xenografted tumors in an athymic nude mouse model.
Synergistic inhibition of tumor angiogenesis in vivo. (a) Immunohistochemical detection for CD34 expression in SMMC-7721 hepatocarcinoma s.c. xenografted tumors. Representative pictures for different treatment groups are shown. The positive expression of CD34 was mainly represented as brownish yellow or brownish granules in tumor vascular endothelial cells. (b) The tumor MVD in different treatment groups. Ad-ING4 plus CDDP combination treatment synergistically inhibited in vivo angiogenesis of SMMC-7721 hepatocarcinoma s.c. xenografted tumors (*P<0.05, compared with Ad-GFP and PBS group, one-way repeated measures ANOVA and multiple comparisons, n=6 mice per condition, n=5 observations per representative section; #CI in the Ad-ING4 plus CDDP combination treatment >1). Data shown are representative of three independent experiments.
Discussion
Recent studies have shown that ING4 as a novel tumor suppressor is involved in a variety of processes including oncogenesis, cell cycle control, apoptosis, DNA repair, angiogenesis, migration and gene transcription regulation. ING4 can significantly inhibit tumor cell growth and induce cell cycle alteration and apoptosis in a variety of tumors. ING4 can also suppress brain-tumor angiogenesis by inhibiting the activity of NF-κB leading to transcriptional repression of NF-κB-responsive genes such as IL-6, IL-8 and Cox-2 by physically interacting with the p65 subunit of NF-κB.13 Nozell et al.33 further confirmed that ING4 can specifically regulate the activity of NF-κB molecules that are bound to target gene promoters. Furthermore, Colla et al.20 reported that ING4 can suppress HIF-1a activity and its target gene NIP-3 expression in myeloma cells under hypoxic condition and consequently inhibit tumor angiogenesis. In addition, ING4 can suppress tumor-cell spreading, migration and invasion by colocalizing and interacting with liprin α1 at the lamellipodia and downregulating the expression and activity of MMP-2 and MMP-9.16, 21, 34 These findings revealed that ING4 as a potent tumor suppressor negatively modulates tumor growth via multiple pathways.
Chemotherapy is one of the commonly used strategies in HCC treatment, especially for unresectable patients. Conventional chemotherapy drugs often have severe side effects that limit their efficacy. Moreover, tumor cells are able to acquire resistance to chemotherapy. The increased dose of chemotherapy drug that is necessary to overcome resistance of tumor cells, even a small increase, may result in severe cytotoxicity to normal cells. Therefore, it is urgent to explore novel approaches to broaden the application of the chemotherapy drug in cancer therapy. To enhance therapeutic effect, eliminate drug resistance and reduce side effects, several conjugated strategies such as the combined treatment of gene therapy and conventional chemotherapy (chemo-gene therapy) have been applied successfully in cancer chemotherapy. Our previous studies demonstrated that Ad-ING4 gene transfer can induce growth inhibition and apoptosis in human lung and pancreatic carcinoma cells.21, 22 A recent study has shown that ING4 can enhance chemosensitivity to doxorubicin and etoposide in HepG2 hepatocarcinoma cells,19 suggesting that it may be used as a chemosensitive modulator in the combination therapy with chemotherapy drugs. However, the combined effect of Ad-ING4 gene therapy and CDDP, an attractive chemotherapy drug, on human cancers, is still unknown. Therefore, in this study, we were interested in addressing the therapeutic effect of chemo-gene therapy by combining Ad-ING4 with CDDP on human hepatocarcinoma cells in vitro and in vivo in an athymic nude mouse model and its potential mechanism.
Before initiating in vitro combination therapy, we first assessed the cytotoxic effect of Ad-ING4 or CDDP alone on SMMC-7721 and HepG2 hepatocarcinoma cells and HL-7702 normal liver cells. We found that Ad-ING4 significantly inhibited SMMC-7721 human hepatocarcinoma cell growth, whereas it moderately inhibited HepG2 hepatocarcinoma cell growth. However, Ad-ING4 had only a minimal effect on HL-7702 normal human liver cells, indicating that transgene ING4 overexpression exerts selective tumor-killing activity in hepatocarcinoma cells. In addition, chemotherapy drug CDDP induced a dose-dependent growth inhibition in SMMC-7721 and HepG2 hepatocarcinoma cells or HL-7702 normal liver cells. Furthermore, the HepG2 hepatocarcinoma cells were more sensitive to CDDP than SMMC-7721 hepatocarcinoma cells. Different tumor cell lines are different in their susceptibility to drugs. In this study, the HepG2 and SMMC-7721 hepatocarcinoma cell lines are both adherent and epithelial-like cells, but from different origins. The former was established from the tumor tissue of a 15-year-old Argentine boy with HCC in 1975, which was reported to produce a variety of proteins such as alpha-fetoprotein, albumin, alpha2-macroglobulin, alpha1-antitrypsin and transferrin. The latter was established from the tumor tissue of a 56-year-old Chinese man with HCC in 1980. The different origins and different biological activities may be one of the reasons for the different susceptibility to Ad-ING4 and CDDP. In addition, higher concentration of CDDP (6 or 12 μg ml−1) exhibited significant growth-suppressive effect on HL-7702 normal liver cells, while 3 μg ml−1 of CDDP only induced slight cytotoxicity. To minimize toxicity to normal cells and produce only modest antitumor efficacy when used as monotherapy, while leaving a window for observation of additive or synergistic effects of Ad-ING4 plus CDDP combination therapy, we selected the relatively non-sensitive hepatocarcinoma cell line to CDDP, SMMC-7721, and the optimal dose of 1.5 μg ml−1 of CDDP in the in vitro combination treatment. We demonstrated that Ad-ING4 plus CDDP combination treatment selectively exerted in vitro synergistic therapeutic activity in SMMC-7721 hepatocarcinoma cells, but not in HL-7702 normal liver cells. Moreover, treatment of SMMC-7721 hepatocarcinoma cells with Ad-ING4 plus CDDP resulted in enhancement of apoptosis. To further address the underlying mechanism involved in Ad-ING4 plus CDDP-induced enhanced antitumor activity, the expression of apoptosis-related proteins such as Fas, caspase-8, Bid, Bcl-2, Bcl-XL, Bax, Bak, caspase-9, caspase-3 and PARP in different treatments of SMMC-7721 hepatocarcinoma cells was assessed by western blot analysis. Fas as an important apoptotic marker has been shown to regulate FasL–Fas extrinsic apoptotic pathway.35 Associated with the increase in Fas expression is the cleavage of Caspase-8 and Bid, downstream targets of Fas, that have a important role in the extrinsic apoptotic pathway.35 Moreover, caspase-8-mediated cleavage of Bid, which translocates to the mitochondria, also results in the activation of intrinsic apoptotic pathway.36, 37 Bcl-2 protein family is known to be a key regulator of apoptosis and an important determinant of cell fate.38 The ratio of anti- to pro-apoptotic molecules (Bcl-2, Bcl-XL; Bax, Bak) constitutes a rheostat that sets the threshold of susceptibility to apoptosis for the intrinsic apoptotic pathway, which promotes pore formation in the mitochondrial outer membrane leading to loss of mitochondrial integrity and the release into the cytosol of cytochrome c followed by the activation of caspase-9, caspase-3 and cleavage of downstream substrate PARP.38, 39 Western blot results showed that Ad-ING4 plus CDDP combination treatment elicited an additive effect on the altered expression of apoptosis-related proteins, leading to the cooperative activation of extrinsic and intrinsic apoptotic pathways, which may closely account for the Ad-ING4 plus CDDP-mediated synergistic growth inhibition and apoptosis in SMMC-7721 hepatocarcinoma cells. In the in vivo combination treatment, a CDDP-dose-finding study was also primarily performed in SMMC-7721 human hepatocarcinoma s.c. xenografted tumor-bearing athymic nude mice by i.p. injection with various doses of CDDP. Mice treated with higher CDDP doses (5 or 10 mg kg−1) caused significant toxicity, while those treated with 1 or 3 mg kg−1 of CDDP showed only minimal toxicity. Moreover, tumor progression was significantly retarded in the mice treated with 3 mg kg−1 of CDDP, but moderately retarded in those treated with 1 mg kg−1 of CDDP. Therefore, an optimal dose of 1 mg kg−1 of CDDP was selected for the in vivo combination treatment. We demonstrated that Ad-ING4 plus CDDP also synergistically suppressed in vivo SMMC-7721 hepatocarcinoma s.c. xenografted tumor growth in an athymic nude mouse model without additive toxicity in vivo. The progressive growth and metastasis of solid tumors is dependent on the process of angiogenesis.40, 41 Tumor angiogenesis has a critical role in the development and progression of HCC. It has been shown that ING4 can suppress tumor angiogenesis by inhibiting the activity of NF-κB and HIF-1a.13, 20 It has also been demonstrated that CDDP can exert a potent antiangiogenic activity during CDDP-based cancer chemotherapy.42, 43 To explore the combined effect of Ad-ING4 plus CDDP on tumor angiogenesis in vivo, the MVD in SMMC-7721 hepatocarcinoma xenografted tumor tissues was determined by CD34 immunohistochemistry analysis. We further found that Ad-ING4 plus CDDP synergistically downregulated CD34 expression and suppressed angiogenesis in SMMC-7721 hepatocarcinoma s.c. xengrafted tumors, which may be another important mechanism involved in Ad-ING4 plus CDDP-mediated in vivo synergistic growth inhibition of SMMC-7721 hepatocarcinoma xenografted tumor in an athymic nude mouse model.
Taken together, Ad-ING4 plus CDDP combined treatment resulted in in vitro and in vivo synergistic growth inhibition, enhanced apoptosis, had an additive effect on upregulation of Fas, Bax, Bak, cleaved Bid, cleaved caspase-8, caspase-9, caspase-3 and cleaved PARP, and on downregulation of Bcl-2 and Bcl-XL in SMMC-7721 hepatocarcinoma cells, and synergistically reduced CD34 expression and MVD in SMMC-7721 hepatocarcinoma s.c. xenografted tumors. Most importantly, the combination of Ad-ING4 with CDDP did not have overlapping toxicities in in vitro HL-7702 normal liver cells and in vivo normal liver tissues of mice. The enhanced antitumor effect in vitro and in vivo elicited by Ad-ING4 plus CDDP was closely associated with the increased Fas expression and cleavage of Caspase-8 and Bid, and decrease in the ratio of anti to pro-apoptotic molecules (Bcl-2, Bcl-XL; Bax, Bak) followed by activation of Caspase-9 leading to Caspase-3 activation and apoptosis by cooperatively regulating extrinsic and intrinsic apoptotic pathways, and the in vivo synergistic inhibition of tumor angiogenesis. Thus, our results indicate that Ad-ING4 plus CDDP is a potential combined treatment strategy for hepatocarcinoma.
References
Parkin DM, Bray F, Ferlay J, Pisani P . Estimating the world cancer burden: Globocan 2000. Int J Cancer 2001; 94: 153–156.
Kamel IR, Kruskal JB, Raptopoulos V . Imaging for right lobe living donor liver transplantation. Semin Liver Dis 2001; 21: 271–282.
El-Serag HB, Davila JA, Petersen NJ, McGlynn KA . The continuing increase in the incidence of hepatocellular carcinoma in the United States: an update. Ann Intern Med 2003; 139: 817–823.
Poon RT, Fan ST, Lo CM, Ng IO, Liu CL, Lam CM et al. Improving survival results after resection of hepatocellular carcinoma: a prospective study of 377 patients over 10 years. Ann Surg 2001; 234: 63–70.
Poon RT, Fan ST . Resection prior to liver transplantation for hepatocellular carcinoma: a strategy of optimizing the role of resection and transplantation in cirrhotic patients with preserved liver function. Liver Transpl 2004; 10: 813–815.
Poon RT, Fan ST, Tsang FH, Wong J . Locoregional therapies for hepatocellular carcinoma: a critical review from the surgeon's perspective. Ann Surg 2002; 235: 466–486.
Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, Burroughs AK et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol 2001; 35: 421–430.
Shiseki M, Nagashima M, Pedeux RM, Kitahama-Shiseki M, Miura K, Okamura S et al. p29ING4 and p28ING5 bind to p53 and p300, and enhance p53 activity. Cancer Res 2003; 63: 2373–2378.
He GH, Helbing CC, Wagner MJ, Sensen CW, Riabowol K . Phylogenetic analysis of the ING family of PHD finger proteins. Mol Biol Evol 2005; 22: 104–116.
Aasland R, Gibson TJ, Stewart AF . The PHD finger: implications for chromatin-mediated transcriptional regulation. Trends Biochem Sci 1995; 20: 56–59.
Doyon Y, Cayrou C, Ullah M, Landry AJ, Cote V, Selleck W et al. ING tumor suppressor proteins are critical regulators of chromatin acetylation required for genome expression and perpetuation. Mol Cell 2006; 21: 51–64.
Zhang X, Wang KS, Wang ZQ, Xu LS, Wang QW, Chen F et al. Nuclear localization signal of ING4 plays a key role in its binding to p53. Biochem Biophys Res Commun 2005; 331: 1032–1038.
Garkavtsev I, Kozin SV, Chernova O, Xu L, Winkler F, Brown E et al. The candidate tumour suppressor protein ING4 regulates brain tumour growth and angiogenesis. Nature 2004; 428: 328–332.
Gunduz M, Nagatsuka H, Demircan K, Gunduz E, Cengiz B, Ouchida M et al. Frequent deletion and down-regulation of ING4, a candidate tumor suppressor gene at 12p13, in head and neck squamous cell carcinomas. Gene 2005; 356: 109–117.
Fang F, Luo LB, Tao YM, Wu F, Yang LY . Decreased expression of inhibitor of growth 4 correlated with poor prognosis of hepatocellular carcinoma. Cancer Epidemiol Biomarkers Prev 2009; 18: 409–416.
Li J, Martinka M, Li G . Role of ING4 in human melanoma cell migration, invasion and patient survival. Carcinogenesis 2008; 29: 1373–1379.
Cai L, Li X, Zheng S, Wang Y, Li H, Yang J et al. Inhibitor of growth 4 is involved in melanomagenesis and induces growth suppression and apoptosis in melanoma cell line M14. Melanoma Res 2009; 19: 1–7.
Li M, Jin Y, Sun WJ, Yu Y, Bai J, Tong DD et al. Reduced expression and novel splice variants of ING4 in human gastric adenocarcinoma. J Pathol 2009; 219: 87–95.
Zhang X, Xu LS, Wang ZQ, Wang KS, Li N, Cheng ZH et al. ING4 induces G2/M cell cycle arrest and enhances the chemosensitivity to DNA-damage agents in HepG2 cells. FEBS Lett 2004; 570: 7–12.
Colla S, Tagliaferri S, Morandi F, Lunghi P, Donofrio G, Martorana D et al. The new tumor-suppressor gene inhibitor of growth family member 4 (ING4) regulates the production of proangiogenic molecules by myeloma cells and suppresses hypoxia-inducible factor-1 alpha (HIF-1alpha) activity: involvement in myeloma-induced angiogenesis. Blood 2007; 110: 4464–4475.
Xie Y, Zhang H, Sheng W, Xiang J, Ye Z, Yang J . Adenovirus-mediated ING4 expression suppresses lung carcinoma cell growth via induction of cell cycle alteration and apoptosis and inhibition of tumor invasion and angiogenesis. Cancer Lett 2008; 271: 105–116.
Xie YF, Sheng W, Xiang J, Zhang H, Ye Z, Yang J . Adenovirus-mediated ING4 expression suppresses pancreatic carcinoma cell growth via induction of cell-cycle alteration, apoptosis, and inhibition of tumor angiogenesis. Cancer Biother Radiopharm 2009; 24: 261–269.
Kim S, Chin K, Gray JW, Bishop JM . A screen for genes that suppress loss of contact inhibition: identification of ING4 as a candidate tumor suppressor gene in human cancer. Proc Natl Acad Sci USA 2004; 101: 16251–16256.
Unoki M, Shen JC, Zheng ZM, Harris CC . Novel splice variants of ING4 and their possible roles in the regulation of cell growth and motility. J Biol Chem 2006; 281: 34677–34686.
Kelland L . The resurgence of platinum-based cancer chemotherapy. Nat Rev Cancer 2007; 7: 573–584.
Rosenberg B, Vancamp L, Krigas T . Inhibition of Cell Division in Escherichia Coli by Electrolysis Products from a Platinum Electrode. Nature 1965; 205: 698–699.
Morton RP, Rugman F, Dorman EB, Stoney PJ, Wilson JA, McCormick M et al. Cisplatinum and bleomycin for advanced or recurrent squamous cell carcinoma of the head and neck: a randomised factorial phase III controlled trial. Cancer Chemother Pharmacol 1985; 15: 283–289.
Williams SD, Birch R, Einhorn LH, Irwin L, Greco FA, Loehrer PJ . Treatment of disseminated germ-cell tumors with cisplatin, bleomycin, and either vinblastine or etoposide. N Engl J Med 1987; 316: 1435–1440.
Yu DC, Chen Y, Dilley J, Li Y, Embry M, Zhang H et al. Antitumor synergy of CV787, a prostate cancer-specific adenovirus, and paclitaxel and docetaxel. Cancer Res 2001; 61: 517–525.
Chen Y, DeWeese T, Dilley J, Zhang Y, Li Y, Ramesh N et al. CV706, a prostate cancer-specific adenovirus variant, in combination with radiotherapy produces synergistic antitumor efficacy without increasing toxicity. Cancer Res 2001; 61: 5453–5460.
Weidner N . Current pathologic methods for measuring intratumoral microvessel density within breast carcinoma and other solid tumors. Breast Cancer Res Treat 1995; 36: 169–180.
Dings RP, Yokoyama Y, Ramakrishnan S, Griffioen AW, Mayo KH . The designed angiostatic peptide anginex synergistically improves chemotherapy and antiangiogenesis therapy with angiostatin. Cancer Res 2003; 63: 382–385.
Nozell S, Laver T, Moseley D, Nowoslawski L, De Vos M, Atkinson GP et al. The ING4 tumor suppressor attenuates NF-kappaB activity at the promoters of target genes. Mol Cell Biol 2008; 28: 6632–6645.
Shen JC, Unoki M, Ythier D, Duperray A, Varticovski L, Kumamoto K et al. Inhibitor of growth 4 suppresses cell spreading and cell migration by interacting with a novel binding partner, liprin alpha1. Cancer Res 2007; 67: 2552–2558.
Nagata S . Fas ligand-induced apoptosis. Annu Rev Genet 1999; 33: 29–55.
Luo X, Budihardjo I, Zou H, Slaughter C, Wang X . Bid, a Bcl2 interacting protein, mediates cytochrome c release from mitochondria in response to activation of cell surface death receptors. Cell 1998; 94: 481–490.
Li H, Zhu H, Xu CJ, Yuan J . Cleavage of BID by caspase 8 mediates the mitochondrial damage in the Fas pathway of apoptosis. Cell 1998; 94: 491–501.
Chao DT, Korsmeyer SJ . BCL-2 family: regulators of cell death. Annu Rev Immunol 1998; 16: 395–419.
Oltvai ZN, Milliman CL, Korsmeyer SJ . Bcl-2 heterodimerizes in vivo with a conserved homolog, Bax, that accelerates programmed cell death. Cell 1993; 74: 609–619.
Folkman J . Tumor angiogenesis: therapeutic implications. N Engl J Med 1971; 285: 1182–1186.
Carmeliet P, Jain RK . Angiogenesis in cancer and other diseases. Nature 2000; 407: 249–257.
Kong C, Zhu Y, Sun C, Li Z, Sun Z, Zhang X et al. Inhibition of tumor angiogenesis during cisplatin chemotherapy for bladder cancer improves treatment outcome. Urology 2005; 65: 395–399.
Tan GH, Tian L, Wei YQ, Zhao X, Li J, Wu Y et al. Combination of low-dose cisplatin and recombinant xenogeneic endoglin as a vaccine induces synergistic antitumor activities. Int J Cancer 2004; 112: 701–706.
Acknowledgements
This research work was supported by a grant from the National Natural Science Foundation of China (No. 81001016).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Xie, Y., Sheng, W., Miao, J. et al. Enhanced antitumor activity by combining an adenovirus harboring ING4 with cisplatin for hepatocarcinoma cells. Cancer Gene Ther 18, 176–188 (2011). https://doi.org/10.1038/cgt.2010.67
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cgt.2010.67
Keywords
This article is cited by
-
Efficacy of combining ING4 and TRAIL genes in cancer-targeting gene virotherapy strategy: first evidence in preclinical hepatocellular carcinoma
Gene Therapy (2018)
-
Adenovirus-mediated TIPE2 overexpression inhibits gastric cancer metastasis via reversal of epithelial–mesenchymal transition
Cancer Gene Therapy (2017)
-
Adenovirus-directed expression of TIPE2 suppresses gastric cancer growth via induction of apoptosis and inhibition of AKT and ERK1/2 signaling
Cancer Gene Therapy (2016)
-
Combination of bladder cancer-specific oncolytic adenovirus gene therapy with cisplatin on bladder cancer in vitro
Tumor Biology (2014)
-
Enhanced tumor suppression by adenoviral PTEN gene therapy combined with cisplatin chemotherapy in small-cell lung cancer
Cancer Gene Therapy (2013)