Abstract
We examined possible combinatory antitumor effects of replication-competent type 5 adenoviruses (Ad) lacking E1B-55kDa molecules (Ad-delE1B55) and chemotherapeutic agents in nine human esophageal carcinoma cells. Ad-delE1B55 produced cytotoxic effects on all the carcinoma cells and the cytotoxicity is not directly linked with the p53 status of the tumors or with the infectivity to respective tumors. A combinatory treatment with Ad-delE1B55 and an anticancer agent, 5-fluorouracil (5-FU), mitomycin C or etoposide, produced greater cytotoxic effects than that with either the Ad or the agent. Administration of 5-FU could minimally inhibit the viral replication and a simultaneous treatment with the Ad and 5-FU achieved better cytotoxicity than sequential treatments. We also confirmed the antitumor effects by the combination of Ad-delE1B55 with 5-FU in vivo. Cisplatin, however, did not achieve the combinatory effects in most of the cells tested. These data indicate that the Ad-delE1B55 produce combinatory antitumor effects with a chemotherapeutic agent irrespective of the administration schedule, but the effects depend on an agent in esophageal carcinoma.
Similar content being viewed by others
Introduction
Esophageal carcinoma frequently develops in aged persons, and surgical procedures often decrease the quality of the patient’s life. Esophageal carcinoma in general responds to chemotherapy and radiotherapy but further improvement in prognosis is required.1 Gene therapy with replication-competent adenoviruses (Ad) is a possible strategy to improve the quality and prognosis of patients. Ad lacking the E1B-55kDa molecules (Ad-delE1B55) replicate preferentially in tumors,2 and a number of clinical trials have been conducted with the Ad to show acceptable safety profiles even in the systemic delivery.3, 4, 5 An advantage of such replication-competent Ad is a continuous spread of the virus progenies released from damaged tumors into neighboring uninfected tumor cells, which enhances antitumor effects even if the initial transduction efficiency to tumors may not be great. Ad-delE1B55 was originally hypothesized to target only tumors deficient of functional p53 by virtue of the inability to express the p53-inactivating E1B-55kDa protein2 and in fact showed greater cytotoxicity to p53-mutated tumors than wild-type (WT) p53 tumors.6 Further investigations, however, did not support the direct correlation between the cytotoxicity and the p53 status in target cells.7 In addition, recent studies revealed a novel function of E1B-55kDa molecules in viral mRNA transport into cytoplasm.8 The study showed efficient Ad-delE1B55 mRNA transport in tumor cells but not in normal cells, which resulted in preferential cell lysis of tumors. Precise mechanisms of the preferential replication in tumors in fact remain uncharacterized; however, clinical studies empirically demonstrated the enhanced tumor cell death by Ad-delE1B55 and the potential therapeutic potential for cancer treatment.3, 4, 5, 9
The majority of Ad-delE1B55 sequences including the fiber-knob regions is derived from type 5 Ad, which use primarily the coxsackievirus and Ad receptor as the primary receptors for binding to target cells.10 Efficacy of Ad-delE1B55-mediated cytotoxicity is influenced by the infectivity and the replication ability. The coxsackievirus and Ad receptor expression level therefore has a crucial role in the cytotoxicity. Head and neck cancer is a major target of Ad-delE1B55 in clinical settings, and in particular a combinatory administration with an anticancer agent has been investigated.9, 11 A few studies, however, have studied efficacy of the replication-competent Ad in esophageal carcinoma,12 most of which are pathologically the same squamous cell carcinoma as head and neck cancer. Moreover, the efficacy of Ad-delE1B55 in esophageal carcinoma was not analyzed from the standpoint of the p53 status or the Ad infectivity, and combinatory effects of the replication-competent Ad with chemotherapeutic agents have not been well studied. Efficacy of replication-competent Ad-mediated cytotoxicity can partly depend on the productivity of the viral progenies, and anticancer agents might be inhibitory to the viral protein syntheses. The combination therefore could impair the Ad production and subsequently decrease the antitumor effects. An administration schedule of the Ad and chemotherapeutics might also be influential to the combinatory cytotoxicity, and these issues have not been well investigated particularly with esophageal carcinoma.
In this study, we examined the cytotoxicity of Ad-delE1B55 with a panel of human squamous esophageal carcinoma cells and sought to find any correlation between the cytotoxicity and the p53 status or the infectivity. We also analyzed the effects of an anticancer agent on the viral replication and further tested possible combinatory antitumor effects of Ad-delE1B55 and 5-fluorouracil (5-FU), mitomycin C (MMC), etoposide (VP-16) or cisplatin (CDDP), some of which are commonly used for esophageal carcinoma treatments.
Materials and methods
Cells and mice
Human esophageal carcinoma cells, TE-1, TE-2, TE-10, TE-11 YES-2, YES-4, YES-5, YES-6 and T.Tn, were cultured with RPMI 1640 medium supplemented with 10% fetal calf serum. Paired human fibroblasts HFF cells and their immortalized IF cells,13 which were generated by expressing E6/E7 of type 16 papilloma viruses, were cultured with RPMI 1640 medium with 10% fetal calf serum. BALB/c nu/nu mice (6-week-old females) were purchased from Japan SLC (Hamamatsu, Japan).
Anticancer reagents
5-FU (Wako, Osaka, Japan), MMC (Wako), VP-16 (Sigma-Aldrich, St Louis, MO) and CDDP (Wako) were dissolved with dimethyl sulfoxide or phosphate-buffered saline.
Ad preparation
Ad-delE1B55, in which the 55kDa-encoding E1B region and a part of the E3 region are deleted,2 and replication-incompetent type 5 Ad expressing green fluorescence protein gene (Ad-GFP) or β-galactosidase gene (Ad-LacZ), in which the cytomegalovirus promoter was used, were prepared with an Adeno-X expression system (Takara, Shiga, Japan). Ad titers were determined with tissue culture infectious dose (TCID50) with HEK293 cells.
PCR to detect viral replication
Cells were infected with Ad-delE1B55 at 50 multiplicity of infection (MOI) for 3 h and were washed to remove the Ad. Cellular DNA was then extracted from the supernatants. Wild-type Ad (Ad-WT) DNA was also used as a control. PCRs were conducted with the following primers and conditions: For outside of the E1B-55kDa region, 5′-GTCCTGTGTCTGAACCTGAG-3′ (primer A, forward) and 5′-CACAATGCTTCCATCAAACG-3′ (primer A, reverse), and 10 s at 95 °C for denaturation/20 s at 56 °C for primer annealing/for 35 cycles; for inside of the E1B55kDa region, 5′-AGATACGGAGGATAGGGTGGC-3′ (primer B, forward) and 5′-TTACCCAAATGCAAGGAACAGC-3′ (primer B, reverse), and 10 s at 95 °C/20 s at 58 °C/30 cycles; for glyceraldehydes 3-phosphate dehydrogenase (GAPDH) gene, 5′-ACCACAGTCCATGCCATCAC-5′ (forward) and 5′-TCCACCACCCTGTTGCTGTA-3′ (reverse), and 15 s at 94 °C/15 s at 60 °C/25 cycles.
Infectivity with Ad-GFP
Cells were infected with Ad-GPF (MOI=30) for 30 min and were washed to remove Ad. They were cultured for 2 days and were analyzed for the GFP-positive cell populations with FACScan and CellQuest software (BD Biosciences, San Jose, CA). Cell populations that showed fluorescence greater than the brightest 5% of uninfected cells were judged as positively stained.
In vitro cytotoxicity and viral production
Cells (5 × 103/well) were seeded in 96-well plates and were cultured for 5 days with Ad at different MOIs and/or an anticancer agent at various concentrations. Cell viability was determined with a cell-counting WST kit (Wako) and the relative viability was calculated based on the absorbance without any treatments. For the amounts of viral progenies, cell lysate after treatments was examined for the TICD50 with HEK293 cells.
Annexin V staining and cell cycle analysis
Cells were treated with Ad-delE1B55 and/or 5-FU in different administration schedules as shown in Table 3, and then stained with fluorescein isothiocyanate-conjugated Annexin V (BD Biosciences) and propidium iodide. For cell cycle analysis, treated cells were fixed in ice-cold 70% ethanol, incubated with RNase (50 μg ml−1) and stained with propidium iodide. The staining profiles were analyzed with FACScan and CellQuest software.
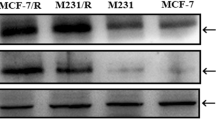
Western blot analysis
Cells were treated with Ad-delE1B55 and/or either 5-FU or VP-16, and the cell lysate were subjected to SDS-polyacrylamide gel electrophoresis. The protein was transferred to a nylon filter and was hybridized with antibodies against Ad E1A (Santa Cruz Biotech, Santa Cruz, CA), Ad hexon (Abcam, Cambridge, UK) or GAPDH (Abcam) as a control. The membranes were developed with the ECL system (GE Healthcare, Buckinghamshire, UK).
Animal experiments
TE-11 cells (1 × 106) were subcutaneously injected into BALB/c nu/nu mice. Tumor volume was calculated according to the formula (1/2 × length × width2). The tumor volumes reached about 75 mm3 on day 8, and mice were randomly assigned into four groups for treatments as follows. Mice were intratumorally injected with culture medium or Ad-delE1B55 (108 plaque forming units (p.f.u.)) four times every other day (days 8–14), intraperitoneally administered with 5-FU (30 mg kg−1) three times every other day (days 9–13), or administered everyday with either 5-FU (30 mg kg−1, three times in total) intraperitoneally or Ad-delE1B55 (108 p.f.u., four times) intratumorally (days 8–14). The animal experiments were performed according the guideline on animal experiments of Chiba University.
IC50 and statistical analysis
IC50 was analyzed with a program related to nonlinear least squares in FORTRAN77 Version 3.5 developed by Dr Yamaoka (Kyoto University, Kyoto, Japan, http://www.pharm.kyoto-u.ac.jp/byoyaku/Kinetics/program/manual.htm). Statistical analyses were performed with analysis of variance and correlation coefficient.
Results
Replication of Ad-delE1B55 in the infected cells
We examined release of Ad-delE1B55 from infected TE-1 and YES-4 cells with PCR using primer sets that were designed to cover the whole E1B region (Figure 1a). The expected E1B-55kDa-deleted DNA was amplified from the culture supernatants and the amount increased after the infection (Figure 1b). Accompanied amplification of GAPDH bands showed increased cell destruction by Ad-delE1B55. We further confirmed the deleted E1B55kDa region with two kinds of primer sets that distinguished the deletion and Ad-WT DNA (Figure 1c). These data showed that Ad-delE1B55 destroyed the infected cells, and the progenies were released without producing Ad-WT.
Detection of Ad-delE1B55 DNA and the viral replication in tumor cells. (a) Diagram of primer A and B sets to amplify the outside and inside of the E1B55-kDa-encoding region. An expected size of the PCR product with primer A sets is 2412 bp for Ad-WT and 1585 bp for Ad-delE1B55, and that with primer B sets is 569 bp for Ad-WT and none for Ad-delE1B55. (b) Sequential increase of PCR products. DNA was extracted from the same volume of culture supernatants from Ad-delE1B55-infected TE-1 and YES-4 cells on the indicated day. (c) Deletion of the E1B-55kDa region in DNA extracted from the infected cells. Ad-WT DNA was used as a control.
Cytotoxicity of Ad-E1B55kDa to esophageal carcinoma
We examined cytotoxic activity of Ad-delE1B55 in nine kinds of squamous esophageal carcinoma cells (Figure 2a) and found that all the cells were susceptible to Ad-delE1B55. T.Tn cells were exceptionally sensitive to Ad-LacZ at a high MOI, but others were insensitive to the control. We then examined the correlation between the Ad-delE1B55-mediated cytotoxicity and the Ad infectivity, which was evaluated with Ad-GFP (Table 1). We used two indicators, mean GFP fluorescence intensity and percentage of GFP-positive cells, both of which showed Ad infectivity, although the former indicator was also influenced by a cytomegalovirus promoter-mediated transcriptional activity in the cells. We calculated IC50 values of Ad-delE1B55 to respective cells to represent the susceptibility (Table 1) and found that the IC50 values did not correlate with the mean fluorescence intensity (P=0.44) or percentages of the positive cells (P=0.38), suggesting that the Ad-delE1B55 cytotoxicity was not directly linked with the infectivity but depended on the cell type.
We also examined the correlation between the Ad-delE1B55 cytotoxicity and the endogenous p53 status. A direct sequencing technique revealed that four cell lines had the WT p53 gene and five lines had the mutation that induced amino-acid changes (Table 1). Although the tumors with p53 mutations were more susceptible to Ad-delE1B55 (average IC50: 27.8±7.1(s.e.)) than those with the WT p53 (average IC50: 56.6±16.4), correlation studies revealed that the p53 status was not associated with the IC50 values (P=0.13). The p53 status was not linked with the Ad infectivity, the mean fluorescence intensity (P=0.53) or percentage of positive cells (P=0.37). These data collectively suggest that the infectivity and the endogenous p53 status are not a marker to predict the Ad-delE1B55-mediated cytotoxicity. In order to confirm that Ad-delE1B55 preferentially induced cytotoxicity in cells devoid of functional p53, we examined the susceptibility with a paired fibroblasts, parental HFF normal fibroblasts and HFF-derived IF cells that were immortalized by the papilloma E6/E7 gene.13 Our previous study also showed that Ad-GFP infectivity was not different between HFF and IF cells and that the p53 expression was induced by CDDP in HFF but not in IF cells, showing that the p53 function was lost in IF cells.14 We found that the cytotoxicity of Ad-delE1B55 was greater in IF than in HFF cells (Figure 2b, P<0.05). HFF and IF cells were relatively resistant to type 5 Ad infection, and high MOIs were required for the cytotoxicity compared with the esophageal carcinoma cells tested. These data collectively suggest that Ad-delE1B55-mediated cytotoxicity was greater in cells with loss of p53 functions, but was more dependent on cell-type difference in esophageal carcinoma.
Influence of 5-FU to Ad-delE1B55-mediated cytotoxicity
We first examined whether an anticancer agent influenced the expression levels of viral protein, as the agents inhibit protein synthesis of host cells. We investigated expressions of E1A and hexon proteins, which represent early and late viral gene products, respectively (Figure 3a). E1A protein was produced as early as 12 h after the infection and the production reached to the maximum at 48 h, whereas hexon protein became detectable after 36 h and peaked at 48 h. We then examined the influence of anticancer agents, 5-FU and VP-16, to viral protein synthesis at 48 h in three different administration schedules, Ad administration followed by the agent, the agent followed by Ad and a simultaneous treatment with Ad and the agent (Figure 3b). Production of hexon protein was inhibited by either 5-FU or VP-16 irrespective of the treatment procedures. In contrast, E1A production was downregulated by 5-FU administered before the Ad and by VP-16 after the Ad, but was relatively maintained in other treatment schedules. These data suggest that an anticancer agent suppressed synthesis of viral structure proteins but was less inhibitory to that of viral transcriptional factors. We also examined the p53 expression in TE-11 cells bearing the WT p53 and found that Ad-delE1B55 or 5-FU alone and any combinations did not upregulated p53 (data not shown).
(a) Sequential expression of hexon, E1A and GAPDH in TE-11 cells after Ad-delE1B55 infection (MOI=10). (b) Expression of hexon, E1A and GAPDH in TE-11 cells treated with three different schedules. Ad → 5-FU or VP-16, Ad-delE1B55 (MOI=10, day 1) followed by 5-FU (1.25 μM, day 2) or VP-16 (1.25 μM, day 2); 5-FU or VP-16 → Ad, 5-FU or VP-16 (day 1) followed by Ad-delE1B55 (day 2); Ad+5-FU or VP-16, Ad-delE1B55 plus 5-FU or VP-16 at the same time (day 1). The cells treated with the agent only or infected with the Ad only were also tested. Cell lysates were prepared 2 days after Ad-delE1B55 infection. (c) TE-1 or TE-11 cells were treated with Ad-delE1B55 (MOI=10) and/or 5-FU (10 μM) according to the schedule indicated in (b), and cell cycle was analyzed on day 4 (TE-1) or day 6 (TE-11). Respective cell populations showed the average of three samples. (d) Cytotoxic activity of the combination of Ad-delE1B55 (MOI=10) and anticancer agents (5-FU, 10 μM; MMC, 0.625 μM; VP-16, 2.5 μM; CDDP, 10 μM) to TE-1 cells with different treatment schedules. Asterisks show P<0.05.
We next examined the production of the Ad progenies with different treatment schedules (Table 2). Although 5-FU suppressed the production irrespective of the schedules, the total amounts of Ad progenies produced were not statistically different among any groups (P>0.06 in any combinations). The simultaneous 5-FU treatment was less influential to the viral production compared with the sequential treatments. We also examined the cell death with flow cytometry and analyzed Annexin V-positive populations in the combination treatments (Table 3). The Annexin V-positive cell population irrespective of propidium iodide staining profiles was the greatest when TE-11 cells were simultaneously treated with Ad-delE1B55 and 5-FU. As exposure times to Ad-delE1B55 and 5-FU were different, it could not be appropriate to compare apoptotic cell percentages among the treatment groups. Nevertheless, the simultaneously treated group was significantly greater in the cytotoxicity than other groups. Interestingly, Ad-delE1B55 treatment after 5-FU enhanced the 5-FU-mediated cytotoxicity (P<0.01), but Ad-delE1B55 followed by 5-FU did not increase the Ad-delE1B55-mediated cytotoxicity (P>0.4). The mechanism of differential cytotoxicity regarding the administration order of Ad and 5-FU is currently unknown. Cell cycle analyses with TE-1 cells demonstrated that the simultaneous treatment induced more sub-G1 fractions than other administration schedules and that 5-FU or Ad-delE1B55 treatment alone increased S and G2/M phases (Figure 3c). The sub-G1 population of TE-11 cells was also the highest when they were simultaneously treated with VP-16 and Ad-delE1B55 compared with other treatment schedules (Figure 3c) and with 5-FU with Ad-delE1B55 (data not shown). These data collectively suggest that simultaneous administration produced the maximal cytotoxicity in these combinations. We then examined whether cytotoxic effects to TE-1 cells were influenced by treatment sequences in the case of other chemotherapeutic agents, CDDP, MMC and VP-16 (Figure 3d). We found that simultaneous administration was the most effective compared with the other schedules in 5-FU-, VP-16- and MMC-treated cases, but not in CDDP-treated cases.
Combinatory cytotoxic effects of Ad-delE1B55 and anticancer agents
We further examined the cytotoxicity by the combination of Ad-delE1B55 and anticancer agents, 5-FU, MMC, VP-16 or CDDP, in six esophageal carcinoma cells. Cells were treated with Ad-delE1B55 or an anticancer agent alone, or simultaneously with the Ad and the agent (Figures 4a–d). The combination with 5-FU, MMC or VP-16 produced greater cytotoxic effects than the treatment with Ad or the agent alone in all the carcinoma cells tested (P<0.05). In contrast, the combination with CDDP did not increase the cytotoxicity except in T.Tn cells, which were more susceptible to the combinatory use (P<0.05). We calculated respective IC50 values in the cytotoxicity test when the cells were treated with the anticancer agent alone or the combination of Ad-delE1B55 and the agent (Table 4). These esophageal carcinoma cells showed differential sensitivity to respective agents, but all the cells became more susceptible to the combination than to the agent alone in the case of 5-FU, MMC or VP-16. The combination with CDDP, however, rather decreased or did not improve the cytotoxicity except in the case of T.Tn cells.
Representative cytotoxicity data of an anticancer agent, Ad-delE1B55 and the combination tested in six esophageal carcinoma cells. A concentration of the agents was selected at the point that gave the most significant cytotoxicity in the combination. (a) Ad-delE1B55 (MOI=10). Concentrations of 5-FU were different among the cells (0.625–10 μM). (b) Ad-delE1B55 (MOI=2). MMC concentrations (1.25–10 μM). (c) Ad-delE1B55 (MOI=10). VP-16 concentrations (0.625–5 μM). (d) Ad-delE1B55 (MOI=10). CDDP concentrations (3–100 μM).
In vivo antitumor effects by the combination
We investigated whether the combinatory effects were also produced in a TE-11 xenograft model (Figure 5). The mice were started to receive treatment on day 8 with intratumoral Ad-delE1B55 injection, intraperitoneal 5-FU injection or the combination. The tumor growth was retarded with 5-FU or Ad-delE1B55 administration alone, but the combination produced greater therapeutic effects than the monotherapy until day 28 (P<0.05). The antitumor effects in the combination group were significantly greater than those in the 5-FU group after day 28 (P<0.05). No systemic toxicity such as body weight loss was observed during the experiment.
In vivo antitumor effects by the combination of Ad-delE1B55 and 5-FU. TE-11 tumors developed in nude mice were treated from days 8 to 14 with culture medium (days 8, 10, 12 and 14), 5-FU (days 9, 11 and 13), Ad-delE1B55 (days 8, 10, 12 and 14) or Ad-delE1B55 (days 8, 10, 12 and 14) plus 5-FU (days 9, 11 and 13). Data show the mean tumor volumes with s.e. in each group (n=8).
Discussion
In this study, we investigated cytotoxic activity of Ad-delE1B55 with a panel of esophageal squamous cell carcinoma cells and showed that the susceptibility was not related with the p53 status or the Ad infectivity. Previous studies suggest that the Ad-delE1B55-mediated cytotoxicity was greater in p53-mutated tumors than those with WT p53, but was not always directly linked to the endogenous p53 status.7 In this study with isogeneric paired cells that could be equally infected with type 5 Ad, we showed that Ad-delE1B55 produced greater cytotoxicity in p53-inactivated cells than in the parental cells. Discrepant results regarding the relationship between the endogenous p53 status and the susceptibility to Ad can be attributable to the extent of property changes caused by loss of p53 functions. As p53-mediated signal cascades are responsible for a number of cellular properties, such as the proliferation rate, it could be difficult to evaluate all the p53-mediated effects, which are also regulated by other factors and eventually influence Ad-mediated cytotoxicity. Extensive clinical studies are required to understand the linkage because numerous clinical cases can minimize such cell-type differences relevant to the p53 status.
Ad infectivity was subjected to the expression level of the cellular receptor complexes and influences the gene expression. We used Ad-GEP to examine the infectivity and demonstrated that the infectivity did not affect the Ad-delE1B55-mediated cytotoxicity. Cellular factors such as those responsible for viral replication and for activation of apoptosis pathways could be involved in the cytotoxicity. In particular, the transcriptional activity of the AdE1A promoter, which has a pivotal role in initiating the viral replication, could be different among infected cells.15 In addition, cyclin E and E2F are cellular factors to regulate the E1A expression level, and subsequently the level affects the production of Ad-delE1B55 progenies.16, 17 Recently, Royds et al.18 reported that expression of WT p53 enhanced replication of Ad-delE1B55 and favored cell death by increasing late viral protein synthesis. On the other hand, Ad-delE1B55 induced enhanced p53 protein expression and activated the p53 pathways in cells with the WT p53 gene.19 These data indicate that Ad-delE1B55 infection and p53 expression coordinately activate apoptotic pathways. Our data, however, showed that Ad-delE1B55 infection did not upregulate p53 expression in esophageal carcinoma cells with the WT p53 (data not shown). The Ad-induced cytotoxicity therefore may not be directly attributable to the p53-mediated pathways in esophageal carcinoma, although the present data showed that Ad-delE1B55 produced relatively greater cytotoxicity to the p53-mutated tumors than those of the WT p53. Interestingly, Zheng et al.17 also suggested that Ad-delE1B55-induced p53 may not function to activate the downstream pathways. These data collectively suggest that the Ad-delE1B55-mediated cytotoxicity are subjected to multiple cellular factors and further investigations are required for better understanding of the cytotoxicity.
We demonstrated combinatory cytotoxic effects of Ad-delE1B55 and anticancer agents. The mechanisms for the increased cytotoxicity have not been well analyzed but could be attributable to pathways that mediate Ad-induced cell death and drug-induced cytotoxicity.4, 20, 21 Expressed E1A can sensitize the infected cells to chemotherapeutic agents,20 but the E1A expression was rather inhibited by 5-FU in this study. As chemotherapeutics can inhibit protein synthesis of host cells, the treatment sequences of how the agent and Ad were used could influence the combination efficacy by impairing production of viral proteins and consequently the viral progenies. We therefore examined whether administration sequences affected the viral protein synthesis, production of the viral progeny and the cytotoxic activity. We investigated the effects of 5-FU as it is a representative inhibitor of DNA synthesis and is frequently used for esophageal cancer treatment. This study showed that 5-FU and VP-16 inhibited the production of hexon protein irrespective of the administration schedules at 48 h; however, production of viral progenies 5 days after the infection was not significantly impaired. Among the treatment sequences tested, the progeny production was less influenced in the simultaneous treatment compared with other sequential administrations. The increased Annexin V-positive populations and sub-G1 populations were the greatest in the simultaneous treatment among the other treatments, and the simultaneous treatment produced cytotoxic effects better than the others in combination with anticancer agents, except CDDP. The combinatory antitumor effects were also produced in six cell lines when they were tested with 5-FU, MMC or VP-16. The effects, however, were not achieved with CDDP except the case tested in T.Tn cells. IC50 values of the anticancer agents in respective cells were subsequently decreased by Ad-delE1B55 treatments, but those of CDDP were not.
Most of previous studies showed that combinatory effects of replication-competent viruses and anticancer agents were not affected by the treatment sequences,22, 23 as we showed in this study. Viral replication was not generally diminished by anticancer agents,4, 22, 23 and in some cases the agents even increased the viral replication partly because the agent increased Ad infectivity.24 Gutermann et al.23 also showed that the combination effects were independent of viral replication even if the replication was reduced by anticancer agents, and suggested that the antitumor effects depended on the agents but not on tumor cells used. Interestingly, Raki et al.25 reported that gemcitabine reduced viral replication at the initial phase, but the production of viral progenies in total was not affected just as we observed in this study. We examined six cell lines with four kinds of chemotherapeutic agents and confirmed that the combination did not inhibit Ad-induced cytotoxicity but produced greater antitumor effects, except CDDP, which was rather inhibitory to the Ad-mediated cytotoxicity. The discrete outcomes with CDDP could be linked with cell cycle progression by the combination. For example, when G1 phase-blocking erlotinib was administered before S phase-inducing pemetrexed, the combinatory cytotoxicity was reduced despite synergistic effects produced in other treatment schedules.26 Our study showed that 5-FU, VP-16 and MMC enhanced cell cycle at S phase and then induced G2/M phase entry, whereas CDDP induced G1 phase arrest (data not shown). As Ad-delE1B55 also induced S phase and G2/M phase, G1 phase arrest by CDDP was inhibitory to the Ad-mediate cell cycle progression and subsequently was unfavorable to Ad-mediated cytotoxicity. On the other hand, the Ad-induced S phase and G2/M phase could impede CDDP-mediated cytotoxicity and thus the cytotoxicity between Ad and CDDP may generate cross-resistance. In contrast, chemotherapeutics that induced S phase and G2/M phase could enhance replication of replication-competent Ad as the Ad showed greater cytotoxicity in S but not in G1 phase.27 Nevertheless, Yoon et al.28 reported that Ad-delE1B55 produced greater cytotoxicity in combination with CDDP and the cytoplasmic late viral mRNA level was greater when the infected cells were in G0/G1 phase rather than in S phase.29 A mechanism of inability to produce combinatory cytotoxicity with Ad-delE1B55 and CDDDP therefore might need further investigations.
In contrast to this study, previous clinical trials demonstrated that Ad-delE1A55 produced combinatory effects with CDDP and 5-FU to head and neck cancer.11 The reason of this discrepancy regarding combinatory effects with CDDP is also currently unknown, but additional mechanisms might operate in vivo settings. For example, viral infection enhanced production of cytokines including tumor necrosis factor-α and interferons. These molecules increased sensitivity to apoptosis directly or indirectly and can facilitate CDDP- or 5-FU-mediated apoptotic processes. In particular, Ad-delE1B55 lacks the E3 region, which resulted in higher production of tumor necrosis factor-α.30, 31
We also demonstrated the combinatory effects in a xenograft model. In a clinical setting, direct injection of Ad-delE1B55 can be replaced by local administration of carrier cells that were infected Ad-delE1B55. This viruses-loaded carrier cells could be beneficial because retention of the cells at the local tumor site is better than that of the viruses themselves and the viruses are constantly released from the cells. In fact, carrier cells producing replication-competent Ad achieved better therapeutic effects than the Ad themselves.32 A combination of chemotherapy and radiotherapy is a common treatment strategy for esophageal carcinoma in advanced cases, and the present data suggest that direct injections of replication-competent Ad into tumor masses with endoscopy and systemic administration of a chemotherapeutic agent are quite feasible. A number of agents including a molecular-targeted medicine can also be used in combination with other therapeutics, and a recent study showed that inhibitors of heat-shock protein 90, which are one of the candidates of anticancer agents, enhanced replication of Ad-delE1B55.33
In summary, this study with a panel of esophageal carcinoma and four different anticancer agents showed that combinatory antitumor effects produced by Ad-delE1B55 and chemotherapeutic agents were dependent on the agents and suggests that gene therapy with Ad-delE1B55 can be combined with the current standard chemotherapy for esophageal carcinoma. Endoscopy-mediated injection of Ad-delE1B55 can reduce the toxicity caused by anticancer agents and may improve the sensitivity of anticancer agents even in chemotherapy-resistant cases.
References
Siersema PD, van Hillegersberg R . Treatment of locally advanced esophageal cancer with surgery and chemoradiation. Curr Opin Gastroenterol 2008; 24: 535–540.
Bischoff J, Kirn D, Williams A, Heise C, Horn S, Muna M et al. An adenovirus mutant that replicates selectively in p53 deficient human tumor cells. Science 1996; 274: 373–376.
Reid T, Galanis E, Abbruzzese J, Sze D, Wein LM, Andrews J et al. Hepatic arterial infusion of a replicationselective oncolytic adenovirus (dl1520): Phase II viral, immunologic, and clinical endpoints. Cancer Res 2002; 62: 6070–6079.
Chu RL, Post DE, Khuri FR, Van Meir EG . Use of replicating oncolytic adenoviruses in combination therapy for cancer. Clin Cancer Res 2004; 10: 5299–5312.
Lin E, Nemunaitis J . Oncolytic viral therapy. Cancer Gene Ther 2004; 11: 643–664.
You L, Yang C-T, Jablons DM . ONYX-015 works synergistically with chemotherapy in lung cancer cell lines and primary cultures freshly made from lung cancer patients. Cancer Res 2000; 60: 1009–1013.
Rothmann T, Hengstermann A, Whitaker NJ, Scheffner A, Hausen H . Replication of ONYX-015, a potential anticancer adenovirus, is independent of p53 status in tumor cells. J Virol 1998; 72: 9470–9478.
O’Shea CC, Johnson L, Bagus B, Choi S, Nicholas C, Shen A et al. Late viral RNA export, rather than p53 inactivation, determines ONYX-015 tumor selectivity. Cancer Cell 2004; 6: 611–623.
Yu W, Fang H . Clinical trials with oncolytic adenovirus in China. Curr Cancer Drug Targets 2007; 7: 141–148.
Shayakhmetov DM, Papayannopoulou T, Stamatoyannopoulos G, Lieber A . Efficient gene transfer into human CD34+ cells by a retargeted adenovirus vector. J Virol 2000; 74: 2567–2583.
Khuri FR, Nemunaitis J, Ganly I, Arseneau J, Tannock IF, Romel L et al. A controlled trial of intratumoral ONYX-015, a selectively-replicating adenovirus, in combination with cisplatin and 5-fluorouracil in patients with recurrent head and neck cancer. Nat Med 2000; 6: 879–885.
Fujiwara T, Kagawa S, Kishimoto H, Endo Y, Hioki M, Ikeda Y et al. Enhanced antitumor efficacy of telomerase-selective oncolytic adenoviral agent OBP-401 with docetaxel: preclinical evaluation of chemovirotherapy. Int J Cancer 2006; 119: 432–440.
Compton T . An immortalized human fibroblast cell line is permissive for human cytomegalovirus infection. J Virol 1993; 67: 3644–3648.
Ma G, Kawamura K, Li Q, Suzuki N, Liang M, Namba M et al. Cytotoxicity of adenoviruses expressing the wild-type p53 gene to esophageal carcinoma cells is linked with the CAR expression level and indirectly with the endogenous p53 status. Cancer Gene Ther 2009; 16: 832–840.
Zheng X, Rao XM, Snodgrass C, Wang M, Dong Y, McMasters KM et al. Adenoviral E1a expression levels affect virus-selective replication in human cancer cells. Cancer Biol Ther 2005; 4: 1255–1262.
Zheng X, Rao XM, Snodgrass CL, McMasters KM, Zhou HS . Selective replication of E1B55K-deleted adenoviruses depends on enhanced E1A expression in cancer cells. Cancer Gene Ther 2006; 13: 572–583.
Zheng X, Rao XM, Gomez-Gutierrez JG, Hao H, McMasters KM, Zhou HS . Adenovirus E1B55K region is required to enhance cyclin E expression for efficient viral DNA replication. J Viol 2008; 82: 3415–3427.
Royds JA, Hibma M, Dix BR, Hananeia L, Russell IA, Wiles A et al. p53 promotes adenoviral replication and increases late viral gene expression. Oncogene 2006; 25: 1509–1520.
Cherubini G, Petouchoff T, Grossi M, Piersanti S, Cundari E, Saggio I . E1B55K-deleted adenovirus (ONYX-015) overrides G1/S and G2/M checkpoints and causes mitotic catastrophe and endoreduplication in p53-proficient normal cells. Cell Cycle 2006; 5: 2244–2252.
Ueno NT, Bartholomeusz C, Herrmann JL, Estrov Z, Shao R, Andreeff M et al. E1A-mediated paclitaxel sensitization in HER-2/neu-overexpressing ovarian cancer SKOV3.ip1 through apoptosis involving the caspase-3 pathway. Clin Cancer Res 2000; 6: 250–259.
Graat HC, Witlox MA, Schagen FH, Kaspers GJ, Helder MN, Bras J et al. Different susceptibility of osteosarcoma cell lines and primary cells to treatment with oncolytic adenovirus and doxorubicin or cisplatin. Br J Cancer 2006; 94: 1837–1844.
Yu DC, Chen Y, Dilley J, Li Y, Embry M, Zhang H et al. Antitumor synergy of CV787, a prostate cancer-specific adenovirus, and paclitaxel and docetaxel. Cancer Res 2001; 61: 517–525.
Gutermann A, Mayer E, von Dehn-Rothfelser K, Breidenstein C, Weber M, Muench M et al. Efficacy of oncolytic herpesvirus NV1020 can be enhanced by combination with chemotherapeutics in colon carcinoma cells. Hum Gene Ther 2006; 17: 1241–1253.
Cabrele C, Vogel M, Piso P, Rentsch M, Schröder J, Jauch KW et al. 5-Fluorouracil-related enhancement of adenoviral infection is Coxsackievirus-adenovirus receptor independent and associated with morphological changes in lipid membranes. World J Gastroenterol 2006; 12: 5168–5174.
Raki M, Kanerva A, Ristimaki A, Desmond RA, Chen DT, Ranki T et al. Combination of gemcitabine and Ad5/3-Delta24, a tropism modified conditionally replicating adenovirus, for the treatment of ovarian cancer. Gene Therapy 2005; 12: 1198–1205.
Li T, Ling YH, Goldman ID, Perez-Soler R . Schedule-dependent cytotoxic synergism of pemetrexed and erlotinib in human non-small cell lung cancer cells. Clin Cancer Res 2007; 13: 3413–3422.
Bernt KM, Steinwaerder DS, Ni S, Li ZY, Roffler SR, Lieber A . Enzyme-activated prodrug therapy enhances tumor-specific replication of adenovirus vectors. Cancer Res 2002; 62: 6089–6098.
Yoon AR, Kim JH, Lee YS, Kim H, Yoo JY, Sohn JH et al. Markedly enhanced cytolysis by E1B-19kD-deleted oncolytic adenovirus in combination with cisplatin. Hum Gene Ther 2006; 17: 379–390.
Goodrum FD, Ornelles DA . Roles for the E4 orf6, orf3, and E1B 55-kilodalton proteins in cell cycle-independent adenovirus replication. J Virol 1999; 73: 7474–7488.
Heise C, Lemmon M, Kirn D . Efficacy with a replication-selective adenovirus plus cisplatin-based chemotherapy: dependence on sequencing but not p53 functional status or route of administration. Clin Cancer Res 2000; 6: 4908–4914.
Ginsberg HS, Lundholm-Beauchamp U, Horswood RL, Pernis B, Wold WS, Chanock RM et al. Role of early region 3 (E3) in pathogenesis of adenovirus disease. Proc Natl Acad Sci USA 1989; 86: 3823–3827.
Hamada K, Desaki J, Nakagawa K, Zhang T, Shirakawa T, Gotoh A et al. Carrier cell-mediated delivery of a replication-competent adenovirus for cancer gene therapy. Mol Ther 2007; 15: 1121–1128.
O’Shea CC, Soria C, Bagus B, McCormick F . Heat shock phenocopies E1B-55K late functions and selectively sensitizes refractory tumor cells to ONYX-015 oncolytic viral therapy. Cancer Cell 2005; 8: 61–74.
Acknowledgements
This work was partly supported by Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan, the Grant-in-Aid for Cancer Research from the Ministry of Health, Labor and Welfare of Japan and a Grant-in-aid from the Nichias Corporation and the Futaba Electronics Memorial Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Ma, G., Kawamura, K., Li, Q. et al. Combinatory cytotoxic effects produced by E1B-55kDa-deleted adenoviruses and chemotherapeutic agents are dependent on the agents in esophageal carcinoma. Cancer Gene Ther 17, 803–813 (2010). https://doi.org/10.1038/cgt.2010.37
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cgt.2010.37