Abstract
Peroxisome proliferator-activated receptors (PPARs) participate in energy homeostasis and play essential roles in diabetes therapy through their effects on non-pancreas tissues. Pathological microenvironment may influence the metabolic requirements for the maintenance of stem cell differentiation. Accordingly, understanding the mechanisms of PPARs on pancreatic β-cell differentiation may be helpful to find the underlying targets of disrupted energy homeostasis under the pancreatic disease condition. PPARs are involved in stem cell differentiation via mitochondrial oxidative phosphorylation, but the subtype member activation and the downstream regulation in functional insulin-positive (INS+) cell differentiation remain unclear. Here, we show a novel role of PPARβ/ δ activation in determining INS+ cell differentiation and functional maturation. We found PPARβ/δ expression selectively upregulated in mouse embryonic pancreases or stem cells-derived INS+ cells at the pancreatic mature stage in vivo and in vitro. Strikingly, given the inefficiency of generating INS+ cells in vitro, PPARβ/ δ activation displayed increasing mouse and human ES cell-derived INS+ cell numbers and insulin secretion. This phenomenon was closely associated with the forkhead box protein O1 (Foxo1) nuclear shuttling, which was dependent on PPARβ/ δ downstream PI3K/Akt signaling transduction. The present study reveals the essential role of PPARβ/ δ activation on p-Foxo1/Foxo1 status, and in turn, determining INS+ cell generation and insulin secretion via affecting pancreatic and duodenal homeobox-1 expression. The results demonstrate the underlying mechanism by which PPARβ/δ activation promotes functional INS+ cell differentiation. It also provides potential targets for anti-diabetes drug discovery and hopeful clinical applications in human cell therapy.
Similar content being viewed by others
Main
Differentiation of embryonic stem (ES) cells into insulin-positive (INS+) cells offers an innovative approach to screen anti-diabetes drugs, supply donor β-cell sources for cell therapy of diabetes and reveal underlying mechanisms for induced pluripotent stem cell researches.1, 2, 3 However, the spontaneous generation of INS+ cells from ES cells happens at a low rate, and most of these induced cells show limited glucose-stimulated insulin secretion (GSIS), which is limited in basic and clinical applications.4, 5 Consequently, seeking crucial targets and related signaling pathway in functional INS+ cell differentiation has become an important and urgent topic.
Peroxisome proliferator-activated receptors (PPARs) are nuclear receptors that participate in lipid metabolism, mitochondrial function and cell differentiation. PPARs may be involved in maintaining successful pregnancy, and also play essential roles in diabetes therapy via their effects on non-pancreas tissues.6, 7, 8, 9, 10, 11 Although PPAR functioning as the sensor in fatty acid oxidation12 and mitochondrial oxidative phosphorylation is required for stem cell differentiation,13 the link between PPARs and INS+ cell differentiation is still unclear. Three PPAR subtypes, PPARα, PPARβ/δ and PPARγ, have diverse expression profiles and biochemical characteristics in different tissues.8, 9 In mature pancreatic β-cells, PPARβ/δ is highly expressed, whereas the levels of PPARα and PPARγ are relatively lower.14, 15 Functionally, both PPARα and PPARβ/δ display a protective effect against metabolic stress in β-cells;15, 16 PPARγ is required to maintain glucose metabolism, because PPARγ reduction leads to abnormal glucose metabolism in islets.17 To date, little is known about PPAR expression and activation in the differentiation process of ES cell into INS+ cells. Thus, we hypothesize that PPAR activation might be required for the differentiation of pluripotent stem cell into INS+ cells through affecting related signaling transduction.
Forkhead box protein O1 (Foxo1) is a negative regulator of pancreatic and duodenal homeobox-1 (Pdx-1) in adult β-cells.18 Deficiency of Foxo1 improves glucose tolerance and β-cell neogenesis in high-fat high-sucrose feeding mice.19 Foxo1 protects against stress-induced β-cell failure through the induction of two insulin transcription factors—neurogenic differentiation 1 (NeuroD1) and v-maf musculoaponeurotic fibrosarcoma oncogene family, protein A (avian) (Mafa).20 Ablation of Foxo1 in β-cells leads to impaired insulin secretion19 and β-cell dedifferentiation21 under metabolic stress. These reports indicate that Foxo1 possesses diverse functions in pancreas at physiological or pathological conditions. Considering Pdx-1 is required for β-cell generation and maturation at embryonic period,22 we further assume that Foxo1 probably participates in the differentiation of ES cells into functional INS+ cells. PPARs are associated with Akt signaling23, 24, 25 and also interact with Foxo1 in various tissues.26, 27, 28, 29 Oppositely, in the regulation of muscle oxidative metabolism, PPARβδδ induces Foxo1 transcription without the involvement of PI3K pathway.29 Exogenous Pdx-1 expression in ES cells improves pancreatic cell lineage differentiation.30 To date, the possible signaling transduction of PPARs/Foxo1/Pdx-1 pathway has not been defined. On the basis of these observations, therefore, clarifying the specific network will help us to understand how PPARs may affect INS+ cell differentiation.
Both PPARα and PPARγ enhance Pdx-1 expression, but the outcome seems different. For example, PPARαδPdx-1 displays an protecting effect against GSIS insult in rat isolated pancreatic islets and rat insulinoma cells.31, 32 However, PPARγ improves Pdx-1 transcription accompanied by reducing insulinoma cell numbers without affecting Pdx-1 protein expression and GSIS function.31, 32 It implies that diverse regulating links may exist between different PPAR subtypes and Pdx-1. To date, it has not yet been revealed whether PPARβ/δ activation-induced Foxo1 shuttling associates with Pdx-1 in INS+ cell differentiation. PPARβ/δ modulates mitochondrial biogenesis and function,7 and Pdx-1 repression also results in mitochondrial dysfunction.33 We therefore explored the potential link of PPARβ/δδFoxo1 and Pdx-1 in modulating INS+ cell differentiation.
Here, we demonstrate that PPARβ/δ activation is essential for modulating p-Foxo1/Foxo1 status, which contributes to the differentiation of ES cells into INS+ cells and insulin secretion. These results highlight the crucial aspects of PPARβ/δ/Foxo1 on the generation of functional INS+ cells. Therefore, the data may provide new insights into the underlying mechanisms by which PPARβ/δ modulates functional INS+ cell differentiation from induced pluripotent stem cells. These results may also help the development of anti-diabetes drugs.34, 35
Results
PPARβ/δ are highly expressed in mouse ES cell-derived INS+ cells
To evaluate the expression of PPARs in INS+ cell differentiation, we first compared their expressions in mouse embryonic pancreas in vivo (Figure 1a). PPARβ/δ displayed a robust increase from embryonic day E12 to E18 of gestation, and remained almost the same level to newborn pancreas. PPARα only showed a slow upregulation. PPARγ expression descended from E12 to E16 and then tuned to a higher expression level at E18. The results implied that PPARs might be important regulators in mouse embryonic β-cell development.
PPARs expressions at pancreatic mature stage in vivo and in vitro. (a) PPAR protein expressions in pancreas at embryonic days E12, 14, 16, 18 of gestation and newborn mouse, n=3. (b) PPARs expressed during INS+ cell differentiation stage, n=3. (c) Co-expressions of PPARs with insulin at terminal day (left panel), and insulin expression in mouse isolated islets (right panel) were determined by Immunofluorescence staining. Bar=50 μm. (d) Flow cytometry assay demonstrated the PPARs were co-expressed with insulin at the terminal differentiation, n=4. Values represent mean ±S.D.
We further explore the presence of PPARs in ES cell-derived INS+ cell differentiation in vitro. Differentiated INS+ cells from mouse ES cells were harvested according to the three-stage protocol of Schroeder et al.36 The mRNA levels of the islet precursor cell marker Neurogenin 3 (Ngn3), the β-cell differentiation markers NeuroD1, Paired box 4 (Pax4) and NK6 homeobox 1 (Nkx6.1), and the β-cell maturation markers Glucose transporter 2 (Glut-2) and Zinc transporter 8 (ZnT8) were confirmed at each differentiation stage. As shown in Supplementary Figure S1, Ngn3 exhibited a peak expression at the initiation of the third stage; NeuroD1, Pax4, Nkx6.1, Glut-2 and ZnT8 expressions were gradually increased following the Ngn3 expression (Supplementary Figure S1). Meanwhile, the insulin content of induced cells was glucose concentration-dependent (Supplementary Figure S2). All these data suggested that the mature INS+ cells were generated from mouse ES cells. Expressions of PPARs were detected at the third INS+ cell differentiation stage. Western blot indicated that PPARβ/δ expression was increased in a time-dependent manner. However, PPARα expression was sustained at a relatively steady level, whereas PPARγ expression showed a decrease in levels (Figure 1b).
Immunofluorescence imaging analysis showed that insulin expressed at the terminal day of differentiation, in a manner similar to that of mouse isolated islets (Figure 1c). Each PPAR subtype was expressed in induced cells, PPARβδδ was well co-expressed with insulin (Figure 1c). Flow cytometry assay confirmed the co-expression rates in parallel, the ratios of PPARα, PPARβ/δ and PPARγ with insulin were 11.67%, 16.05% and 7.65% at terminal differentiation, respectively (Figure 1d). These results suggested that PPARβ/δ may play a more important role than the other two members in INS+ cell differentiation.
PPARβ/δ/Pdx-1 promoted functional INS+ cell differentiation
We next investigated whether the activation of PPARs could affect INS+ cell differentiation. Treatment with the PPARβ/δ agonist L165041 considerably increased the ratio of differentiated INS+ cells by twofold, raising the ratio from 16.93 to 33.43%. In contrast, treatment with the antagonist GSK0660 decreased the ratio to 9.74%. In contrast, neither PPARα agonist/antagonist, nor PPARγ agonist affected INS+ cell formation (Figure 2a). Immunofluorescence morphological analysis showed that PPARβ/δ activation increased the number of INS+ cells (Figure 2b). Considering that PPARβ/δ is correlated with mitochondrial function in ES cell differentiation,37 we detected the change of mitochondrial membrane potential (ΔΨm) in PPARβ/δ-mediated INS+ cell differentiation. As a result, PPARβ/δ activation was involved in maintaining mitochondrial ΔΨm. The red fluorescence was enhanced by L165041 but attenuated by GSK0660 (Figure 2b).
PPARβ/δ determined Pdx-1 expression and functional INS+ cell generation from mouse ES cells. Cells were treated with PPARs agonists, antagonists from day 5+9, or transfected with sh-PPARβ/δ or sh-NC at day 5+9 and collected at day 5+28 for further detection. PPARα agonist: WY14643; PPARα antagonist: GW6471; PPARβδδ agonist: L165041; PPARβδδ antagonist: GSK0660; PPARγ agonist: GW1929. (a, i) Ratios of INS+ cells at day 5+28 were detected by flow cytometry analysis. (a, n=3, i, n=4.) (b) PPARβδδ changed the insulin-staining area and ΔΨm. Bar=100 μm. (c) Released insulin of induced cells and isolated mouse islets were analyzed. Values were normalized with total protein contents, n=3. (d, l) Insulin secretion level of INS+ cells was measured at terminal day of differentiation. (d, n=5, l, n=3). (e, k) Pancreatic specific gene expressions were detected by quantitative RT-PCR. n=3. (f, h) Western blot analyzed Pdx-1 protein expression at day 5+28, n=3. (g) PPARβδδ protein expression was receded till day 5+28 after sh-PPARβ/δ transfection, n=3. (j) Insulin staining area was reduced after transfected with sh-PPARβ/δ. Bar=100 μm. Values represent mean ±S.D. Statistical significance was set as *P<0.05, **P<0.01 versus DMSO control, +P<0.05, ++P<0.01 versus sh-NC control
Meanwhile, we analyzed the GSIS function of induced cells. Insulin release stimulated by glucose was increased in PPARβ/δ-activated cells, which resembled that of isolated mouse islets (Figure 2c). Although GSK0660-treated cells were still glucose-responsive, they presented impaired insulin secretion function by releasing insulin at a lower efficiency (Figure 2c). Considering the discrepancy in INS+ cell populations among these groups, we also evaluated insulin secretion level of INS+ cells, which was defined as the ratio of released insulin to INS+ cell rates. As a result, insulin secretion level was increased by L165041 but declined by GSK0660 after glucose stimulation (Figure 2d). Meanwhile, PPARα or PPARγ activation did not affect the GSIS function of induced INS+ cells (Supplementary Figure S3a). In addition, insulin-1 and insulin-2 expressions were considerably elevated by L165041 but repressed by GSK0660. In contrast, the expressions of α cell marker glucagon, δ cell marker somatostatin and PP cell marker pancreatic polypeptide were not affected by PPARβ/δ activation (Figure 2e). These data suggested that PPARβ/δ activation may increase INS+ cell generation and insulin secretion accompanied by affecting the ΔΨm and insulin transcription.
We next examined the effect of PPARβ/δ activation on the expression of Pdx-1, the regulator of β-cell generation and function.22, 33 As shown in Figure 2f, PPARβ/δ agonist L165041 increased Pdx-1 expression, whereas the antagonist GSK0660 repressed its expression, indicating that PPARβ/δ may be the upstream event of Pdx-1. In contrast, neither PPARα nor PPARγ activation affected the expression level of Pdx-1 during the differentiation (Supplementary Figure S3b).
To further confirm the effects of PPARβ/δ in INS+ cell differentiation, PPARβ/δ was inhibited by shRNA at the indicating stage. PPARβ/δ expression dropped to 46% in shRNA interfered cells (Figure 2g). Knockdown of PPARβ/δ also decreased Pdx-1 expression (Figure 2h) followed by a decrease in INS+ cells ratio from 16.85 to 8.16% (Figure 2i), and a reduced insulin staining area (Figure 2j). Moreover, knockdown of PPARβ/δ reduced insulin-1 and insulin-2 transcriptions by 48 and 59% (Figure 2k), respectively, and impaired GSIS function of INS+ cells (Figure 2l). Taken together, these results suggest that PPARβ/δ may play an important role in promoting functional INS+ cell differentiation, which might be mediated by Pdx-1 expression.
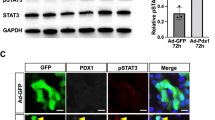
PPARβ/δ activation affected Foxo1 status, Gsk3β and their upstream signaling molecules
Given the observation that Pdx-1 may mediate the effect of PPARβ/δ in INS+ cell differentiation, we next analyzed the expressions and distribution of its negative regulator Foxo1 and Gsk3β.38 We also explored the network of PPARβ/δ with the upstream signaling of Foxo1 and Gsk3β, PI3K/Akt, during pancreatic differentiation stage. Phosphorylated Foxo1 (p-Foxo1) is a nucleocytoplasmic shuttling protein, and we found that the expression levels of cytosolic p-Foxo1, p-Gsk3β, PI3K and p-Akt were all affected by PPARβ/δ activation (Figure 3a). In contrast, the nuclear Foxo1 level displayed the opposite phenomenon after PPARβ/δ activation (Figure 3a). The knockdown of PPARβ/δ in the cells was consistent with the treatments of PPARβ/δ antagonist. Expressions of PI3K, p-Akt, p-Gsk3β, and cytosolic p-Foxo1 were all downregulated after transfection with sh-PPARβ/δ, whereas the nuclear Foxo1 level was increased (Figure 3b).
Foxo1, Gsk3β and PI3K/Akt signaling were associated with PPARβδδ activation. (a) Protein expressions at day 5+15 and day 5+28 were detected after L165041 or GKS0660 treatment from day 5+9. (b) Protein expressions at day 5+28 were analyzed after PPARβδδ shRNA transfection from day 5+9. Values represent mean ±S.D., n =3. Statistical significance was set as *P<0.05, **P<0.01 versus DMSO control, +P<0.05, ++P<0.01 versus sh-NC
All these results indicate that PPARβ/δ activation could regulate the p-Foxo1/Foxo1 status, Gsk3β phosphorylation and PI3K/Akt signaling pathway, which might serve as a switch in controlling INS+ cell differentiation and insulin secretion.
Knockdown of Foxo1 improved PPARβ/δ-mediated cell differentiation
To elucidate the mechanisms underlying PPARβ/δ-mediated INS+ cell differentiation, we further investigated the roles of Foxo1 and Gsk3β at the pancreatic differentiation stage. Foxo1 expression dropped by 52% in shRNA-interfered cells (Figure 4a). Flow cytometry analysis showed that sh-Foxo1 transfection increased the ratio of INS+ cells from 16.83 to 24.3% (Figure 4b). Meanwhile, in sh-PPARβ/δ-transfected cells, Foxo1 knockdown reversed the inhibitory effect on INS+ cell generation from 9.14 to 19.7% (Figure 4b). In addition, sh-Foxo1 increased Pdx-1 expression. Even in the PPARβ/δ knockdown cells, the decreased Pdx-1 was upregulated by transfection of sh-Foxo1 (Figures 4c and d). ELISA demonstrated that sh-Foxo1 resulted in enhanced INS+ cell insulin secretion. Knockdown of Foxo1 improved the sh-PPARβ/δ -induced low insulin levels after incubation with glucose (Figure 4e). The data suggest that Foxo1 regulates the insulin secretory ability of PPARβ/δ-induced INS+ cells.
Knockdown of Foxo1 improved PPARβ/δ-mediated cell differentiation. Cells were transfected with shRNA against PPARβ/δ, Foxo1 and Gsk3β from day 5+9 and harvested at day 5+28. (a, f) Protein expressions of Foxo1 (a) and Gsk3β (f) were repressed till 5+28 after transfection by targeted shRNA. (b, g) Ratios of INS+ cells after transfection were determined by flow cytometry. (c, d and h) Pdx-1 expression was determined by western blot (c, h) and immunofluorescence analysis (d, Bar= 100 μm). (e) Insulin secretion levels of INS+ cells detected by ELISA. Values represent mean ±S.D., n=3. Statistical significance was set as +P<0.05, ++P<0.01 versus sh-NC, *P<0.05, **P<0.01 versus sh-PPARβ/δ
In contrast, although Gsk3β expression was reduced to 51% in sh-Gsk3β-treated cells (Figure 4f), neither INS+ cell population nor Pdx-1 expression was altered after sh-Gsk3β transfection (Figures 4g and h). We therefore confirm that it might be Foxo1 rather than Gsk3β that participated in PPARβ/δ-mediated differentiation of INS+ cells.
Foxo1 modulated two β-cell development regulators NeuroD1 and Mafa;20, 39 therefore, we further explored whether PPARβ/δ activation was associated with the mRNA expression levels of these two factors during differentiation. As a result, neither NeuroD1 nor Mafa was altered by PPARβ/δ activation or inhibition (Supplementary Figure S4). Thus, it implied that PPARβ/δ activation controlled p-Foxo1/Foxo1 status, which regulated INS+ cell differentiation through Pdx-1 signaling without the involvement of NeuroD1 or Mafa signaling.
PI3K/Akt pathway is involved in PPARβ/δ/Foxo1δPdx-1-mediated cell differentiation
To identify how PPARβ/δ regulated Foxo1 expression, we investigated the role of PI3K/Akt pathway in INS+ cell differentiation. Cells were treated with PI3K inhibitor LY294002 in the presence of PPARβ/δ agonist L165041 at the indicating stage. As a result, phosphorylation of Akt was remarkably decreased after PI3K inhibition by LY294002 (Figure 5a). Flow cytometry demonstrated that PI3K/Akt inhibition reduced the ratio of INS+ cells from 16.86 to 9.84% compared with DMSO control, and significantly blocked the promoting effect of PPARβ/δ activation by reducing the percentage of INS+ cells from 32.23 to 18.63% (Figure 5b). Importantly, the suppression of PI3K/Akt pathway decreased the cytosolic p-Foxo1 level accompanied by increased nuclear Foxo1 levels in both DMSO- and L165041-treated cells, indicating that PI3K/Akt pathway may be involved in the regulation of p-Foxo1/Foxo1 status by PPARβ/δ activation during INS+ cell differentiation (Figure 5c), in turn influencing Pdx-1 expression and function (Figure 5d). It implies that, unlike the regulation in muscle oxidative metabolism,29 p-Foxo1/Foxo1 status plays a role in the regulation of PPARβ/δ/Pdx-1 for INS+ cell generation via PI3K/Akt signaling transduction. In contrast, neither PPARα nor PPARγ activation influenced the p-Foxo1/Foxo1 status and PI3K/Akt pathway (Supplementary Figure S5), which therefore further confirmed that it was the PPARβ/δ isoform that has a role in promoting functional INS+ cell generation.
Inhibition of PI3K disturbed the effects of PPARβδδ on INS+ cell differentiation. Cells were treated with L165041 and LY294002 from day 5+9, and harvested at day 5+28 for further analysis. (a) LY294002 inhibited p-Akt expression. (b) The ratios of INS+ cells were determined by flow cytometry. (c) Expressions of cytosolic p-Foxo1 and nuclear Foxo1 were changed after treatment with LY294002. (d) Protein expression of Pdx-1 was analyzed by western blot. Values represent mean ±S.D., n =3. Statistical significance was set as *P<0.05, **P<0.01 versus control, #P<0.05, ##P<0.01 versus L165041-treated groups. (e) Schematic diagram of the signaling pathways involved in PPARβδδ-mediated INS+ cell differentiation of mouse ES cells
Human ES cell-derived functional INS+ cells share the PPARβ/δ pathway during differentiation
To explore whether the PPARβ/δ pathway was involved in the differentiation process of human ES cell-derived INS+ cells, the human cell line H9 was employed and evaluation was performed according to a previous protocol.40 At the terminal differentiation day, immunofluorescence analysis showed that PPARβ/δ was well co-expressed with insulin in the cells (Figure 6a). Additionally, flow cytometry assay demonstrated that the co-expression ratio of PPARβ/δ and insulin was 14.4%, indicating that more than 93% INS+ cells expressed PPARβ/δ at the terminal differentiation (Supplementary Figure S6).
Human ES cell-derived INS+ cells share the same function and signaling pathway of PPARβ/δ activation. (a) Co-expressions of PPARβ/δ with insulin in human ES cell-derived INS+ cells at the terminal differentiation day. Bar=25 μm. Human ES cells were treated with PPARβ/δ agonist L65041 or antagonist GSK0660 at INS+ cell differentiation stage, and the results shown on the terminal day are as follows. (b) The INS+ cells were quantified by flow cytometry assay. (c) Expression of insulin mRNA was detected by quantitative RT-PCR. (d) Insulin secretion level of INS+ cells was measured. (e, f) The molecular events in the PPARβ/δ signaling pathway demonstrated similar characteristics as those in mouse-ES cell-derived INS+ cells, n=3. Values represent mean±S.D. Statistical significance was set as *P<0.05, **P<0.01 versus DMSO control
We then investigated whether PPARβ/δ activation could also promote human ES cells to differentiate into functional INS+ cells during the differentiation period. As a result, PPARβ/δ agonist L165041 increased the ratio of differentiated INS+ cells from 15.2 to 26.17%; conversely, treatment with PPARβδδ antagonist GSK0660 decreased the ratio to 8.32% (Figure 6b). Insulin mRNA expression was also upregulated in PPARβ/δ-mediated human ES cell differentiation (Figure 6c). Meanwhile, insulin secretion level was increased by L165041 but reduced by GSK0660 after glucose stimulation (Figure 6d). In addition, Pdx-1 expression was modulated by PPARβδδ activation as well (Figure 6e). All these results implied that human ES cell-derived INS+ cells shared PPARβ/δ signaling pathway with mouse ES cells in differentiation. Moreover, expression levels of all the events in the pathway, PI3K, p-Akt and cytosolic p-Foxo1, were increased in PPARβδδ-mediated differentiation, while the nuclear Foxo1 was decreased after PPARβδδ activation (Figure 6f). As shown in Figure 6, p-Foxo1/Foxo1 status was also involved in the regulating effect of PPARβ/δ on human ES cell-derived INS+ cells.
Discussion
The present study demonstrates that PPARβ/δ activation plays a crucial role in controlling the differentiation of ES cells into functional INS+ cells. The time-dependent increase in PPARβ/δ suggests that PPARβ/δ may be a major player in functional INS+ cell development during the third INS+ cell differentiation stage. During this period, the highly expressed islet precursor marker was decreased, β-cell differentiation and maturation markers were in turn expressed, indicating that the islet progenitor cells gradually develop into INS+ cells and are ready to secrete insulin. The increased expression tendency of PPARβ/δ is well matched with that in mouse embryonic pancreas at the late development stage in the present study. High expression of PPARβ/δ in embryonic pancreas and mouse ES cells-induced INS+ cells might be essential for INS+ cell differentiation in vivo and in vitro. Our results indicate that PPARβ/δ acts as a unique promoter for INS+ cell differentiation. In contrast, this novel phenomenon is opposite to what happens in mice with mature pancreas. Knockdown of PPARβ/δ in epithelial compartment of the mouse pancreas increased islet numbers and enhanced insulin secretion in the mutant mice after weaning.41 We consider that the differences between ES cells and cells in mature pancreas are partly due to the difference in the mitochondrial-dependent energy generation during developmental embryonic period. Increased mitochondrial oxidative phosphorylation is required for pluripotent stem cell differentiation.12, 13 PPARs regulate transcription of target genes related to mitochondrial biogenesis and oxidative phosphorylation at ES cell differentiation course.13, 42 Mitochondrial ΔΨm status reflects the oxidative phosphorylation function in stem cells. Our results demonstrate that PPARβ/δ activation maintains higher mitochondrial ΔΨm state in differentiated INS+ cell, thereby promoting the INS+ cell maturation at pancreatic differentiation stage.
Foxo1 negatively regulated Pdx-1, and a gain-of-function Foxo1 mutation resulted in impaired β-cell compensation owing to decreased Pdx1 expression.43 Foxo1 displayed distinct effects on pancreas in diverse genetic conditions, and the discrepancy was due to the difference in basal Pdx-1 expression levels.19 In db/db mice, Pdx-1 expression was well maintained, Foxo1 ablation impaired insulin secretion.19 On the contrary, in IRS2 KO mice, Pdx-1 expression was reduced, Foxo1 haploinsufficiency reversed β-cell failure by increasing Pdx-1 expression.44 Moreover, Foxo1 is associated with β-cell dedifferentiation under physiologic stress, however, these effects are due to Foxo1 nuclear localization in β-cells under metabolic stress.21 While in basal condition, Foxo1 deletion does not impair β-cell morphology or function.21 Here, we demonstrated that PPARβ/δ regulated p-Foxo1/Foxo1 status during INS+ cell differentiation. PPARβ/δ activation increased cytosolic p-Foxo1, which resulted in the decrease of nuclear Foxo1, thereby leading to the inactivation of Foxo1. Furthermore, Foxo1 protected against β-cell failure through its upregulating effect on NeuroD1 and MafA, however, the effect occured only under the condition that Foxo1 translocated to nucleus in response to β-cell oxidative stress.20 Conversely, Foxo1 knockin mice with specific activation in both the hypothalamus and pancreas showed decreased NeuroD1 and Mafa expression in islets.39 Here we found that neither NeuroD1 nor Mafa was associated with PPARβ/δ activation-controlled p-Foxo1/Foxo1 status, suggesting that Foxo1 regulated INS+ cell differentiation without the involvement of NeuroD1 or Mafa. In the regulation of muscle oxidative metabolism, PPARβ/δ induces Foxo1 transcription without the involvement of PI3K pathway.29 However, in INS+ cell differentiation process, we have found that PPARβ/δ-activated PI3K/Akt pathway phosphorylated cytosolic Foxo1, thus disturbing the translocation of Foxo1 to nucleus. On the basis of these observations, we conclude that PPARβ/δ activation negatively modulates Foxo1 through PI3K/Akt signaling pathway during INS+ cell differentiation.
Pancreatic islet contains α, β, δ and PP cells. We found that only β-cell-specific genes insulin1 and insulin2 were exclusively modulated by PPARβ/δ. Pdx-1 is a pancreas-specific homeoprotein, specifically localizing to pancreatic progenitor cells and mature β-cells. It designates the pancreas location in early embryos, and acts as a definitive factor for proper differentiation and maturation of pancreatic β-cells by stimulating insulin gene transcription.22 Considering Pdx-1 is essential for functional β-cell generation,22, 45, 46 we hypothesize that Pdx-1 could be a key downstream regulator in PPARβ/δ-induced INS+ cell generation. The expression of Pdx-1 was increased after PPARβ/δ activation and decreased after PPARβ/δ suppression, which acted in accordance with the INS+ cell population and insulin secretion. The observation that Pdx-1 can be upregulated by PPARβ/δ activation has not been reported, and our results establish a novel signaling connection in the PPARβ/δ-induced INS+ cell differentiation. Foxo1 knockdown reversed the inhibitory effects on INS+ cell generation and insulin secretion caused by PPARβ/δ deficiency through the improvement of Pdx-1 expression, indicating that PPARβ/δ regulated Pdx-1 expression in functional INS+ cell differentiation via Foxo1 suppression. In addition, Gsk3β is another Pdx-1 negative regulator and inhibition of Gsk3β was reported to promote β-cell growth.38 However, in the present study, we did not find any effects on Pdx-1 expression or INS+ cell differentiation when Gsk3β is inhibited. Furthermore, neither PPARα nor PPARγ agonist affected the functional INS+ cell generation or the PI3K/Akt/Foxo1/Pdx-1 pathway activation, although PPARα showed a considerable level during differentiation. In conclusion, Foxo1 is a major signaling molecule involved in PPARβ/δ/Pdx-1-promoted functional INS+ cell generation.
Most importantly, we further revealed that PPARβ/δ activation also exhibited its promoting effect on human ES cell-derived INS+ cell differentiation and insulin secretion via the same signaling pathway in mouse ES cell differentiation. Thus, PPARβ/δ expression or activation can serve as a pathological event in the mechanism evaluation of diabetes.
In summary, our study demonstrates that PPARβ/δ plays a crucial role in promoting ES cell-derived INS+ cell differentiation and insulin secretory capacity via affecting p-Foxo1/Foxo1 status (Figure 5e). The new finding sheds light on potential molecular signaling that influences INS+ cell differentiation in pluripotent stem cell research, pathological evaluation, and suggests a potential target for anti-diabetic drug development and hopeful clinical applications in human cell therapy.
Materials and Methods
INS+ cell differentiation of mouse and human ES cells
A three-step protocol36 was applied to induce INS+ cells from mouse ES-D3 cells (CRL-1934, American Type Culture Collection, Manassas, VA, USA). Embryoid bodies were aggregated by ES cells for 5 days, spontaneously generated three germ layers for 9 days in differentiation medium I and then differentiated into pancreatic lineage for another 19 days in differentiation medium II. The differentiation medium I consists of Iscove’s modification of DMEM (IMDM, Life Technologies, Carlsbad, CA, USA), 20% FBS (Life Technologies), Glutamax (Life Technologies), non-essential amino acids (Life Technologies) and 450 μM monothioglycerol (Sigma Aldrich, St. Louis, MO, USA), and differentiation medium II consists of DMEM/F12 (Life Technologies), 10 mM nicotinamide (Sigma Aldrich), 1 μg/ml laminin (Sigma Aldrich), N2 media supplement (Life Technologies) and B27 media supplement (Life Technologies).
Human ES cell line H9 (from WiCell Research Insititute. Simple Letter Agreement: #10-W0353 to Yijia Lou) was differentiated into INS+ cells according to the protocol of Jiang et al.40 Human ES cells were plated into 1% Matrigel (BD Biosciences, San Jose, CA, USA)-coated dishes and cultured with chemically defined medium for 2 days. The chemically defined medium consists of 50% IMDM, 50% DMEM/F12, Insulin-Transferrin-Selenium-A (Life Technologies), 450 μM monothioglycerol and 5 mg/ml albumin fraction V (Sigma Aldrich). Then, cells were induced to generate definitive endoderm with chemically defined medium containing 50 ng/ml activin A (Life Technologies) for 4 days, and cultured with chemically defined medium containing 10−6 M RA (Sigma Aldrich) to generate pancreatic progenitors for another 4 days. Progenitors were then cultured to achieve mature islets with islet maturation medium: DMEM/F12, Insulin-Transferrin-Selenium-A and 2 mg/ml albumin fraction V with 10 ng/ml bFGF (Life Technologies) for 3 days, with 10 mM nicotinamide for the next 5 days, and transferred into Ultra Low Attachment culture dishes for another 5 days in suspension culture after digested by Accutase (Millipore, Billerica, MA, USA).
Chemicals treatments of cultures
Cells were treated with PPARα agonist WY14643 (10 μM, Sigma Aldrich), PPARα antagonist GW6471 (1 μM, Sigma Aldrich), PPARβδδ agonist L165041 (10 μM, Sigma Aldrich), PPARβδδ antagonist GSK0660 (1 μM, Sigma Aldrich), PPARγ agonist GW1929 (10 μM, Sigma Aldrich), PI3K inhibitor LY294002 (7.5 μM, Cell Signaling Technology, Danvers, MA, USA) from day 5+9 to day 5+28 during mouse ES cell differentiation. For human ES cells, PPARβδδ agonist L165041 or antagonist GSK0660 were treated with the same concentration in mouse ES cells from differentiation day 10 to day 23. All these chemicals were dissolved in DMSO (Sigma Aldrich). Control condition was treated with vehicle DMSO (final concentration 0.1%).
Fetal mouse pancreases obtain
ICR mice were obtained from the Experimental Animal Center, Zhejiang University, Hangzhou, Zhejiang, China (GradeI, Certificate No. 2007-0029). Ten-week-old ICR mice (4 female and 1 male) were housed together under a 12 h light/dark cycle. The day that vaginal sperm or a copulation plug was observed was defined as embryonic day 0 (E0) of gestation. Mouse embryonic pancreases were obtained at E12, E14, E16, E18 and from newborns.
Flow cytometry analysis
Mouse ES or human ES differentiated cells at terminal differentiation day were digested into single cells with Accutase. After being fixed in 4% paraformaldehyde for 1 h at 4 °C, cells were blocked with 3% BSA for another 1 h at room temperature. Then, the cells were incubated at 4 °C overnight with primary antibodies: anti-insulin (1 : 200, Cell Signaling Technology), anti-PPARα (1 : 200, Abcam, Cambridge, MA, USA), anti-PPARβδδ (1 : 200, Abcam) or anti-PPARγ (1 : 200, Abcam). After that, cells were incubated with the appropriate secondary antibodies (1 : 500) for 20 min at 4 °C. Cells were collected with a FACS flow cytometer (Beckman Coulter, Carlsbad, CA, USA). The results were expressed as the percentage of the fluorescence intensity.
Immunocytochemistry analysis
Isolated islets were obtained from 8–12-week-old male Balb/c mice (purchased from Experimental Animal Center, Zhejiang University, China, GradeI, Certificate No. 2008-0016) according to the protocol.47 After digesting from pancreases, islets were cultured on cover slips. Both ES cell lines on their terminal differentiation day and isolated islets were fixed with cold methanol for 10 min at −20 °C. Fixed cells were blocked with 10% FBS for 1 h at room temperature. After that, cells were incubated at 4 °C overnight with primary antibodies: anti-insulin (1 : 100), anti-PPARα (1 : 100), anti-PPARβδδ (1 : 100), anti-PPARγ (1 : 100) or anti-Pdx-1 (1 : 100, Cell Signaling Technology). Cultures were treated with appropriate secondary antibodies (1 : 400) for 2 h and DAPI (2 μg/ml, Sigma Aldrich) for 1 min at room temperature. Finally, differentiated cells were observed under Leica DMI3000B microscope (Leica, Mannheim, Germany), and isolated islets were observed under Olympus FV1000 confocal microscope (Olympus, Tokyo, Japan). The overlay images were merged by software Image-Pro Plus.
Western blot analysis
Total protein, cytosolic protein (exclusively for p-Foxo1) and nuclear protein (exclusively for Foxo1) from cells or tissues were harvested. Total proteins were obtained from samples by cell lysis buffer for western (Beyotime, Shanghai, China). Nuclear and cytoplasmic proteins were separated using Nuclear and Cytoplasmic Protein Extraction Kit (Beyotime) according to the manufacturer’s instructions. Cells were dissolved with cytoplasmic protein extraction agent A and were vortexed for 10 s. Then, the cytoplasmic protein extraction agent B was added into the samples. After 5 s vortex and 5 s incubation on ice, the cells were centrifuged for 5 min at 12 000 × g at 4 °C, and the supernatant containing the cytosolic fraction was collected. The pellet was resuspended with nuclear protein extraction agent. After 15–20 times of vortexing for 30 min, the cells were centrifuged for 10 min at 12 000 × g at 4 °C, and the supernatant containing the nuclear extracts was collected. An aliquot of 20 μg protein was loaded and separated on a SDS-polyacrylamide gel. After separation, proteins were transferred onto PVDF membranes. Then, the transferred membranes were blocked in 5% non-fat milk for 1 h and incubated at 4 °C overnight with primary antibodies: anti-PPARα (1 : 1000), anti-PPARβδδ (1 : 1000), anti-PPARγ (1 : 500), anti-Pdx-1 (1 : 1000), anti-Gsk3β (1 : 4000, Cell Signaling Technology), anti-p-Gsk3β (1 : 4000, Cell Signaling Technology), anti-p-Foxo1 (1 : 1000, Cell Signaling Technology), anti-Foxo1 (1 : 1000, Cell Signaling Technology), anti-GAPDH (1 : 5000, Santa Cruz Biotechnology, Santa Cruz, CA, USA), anti-PI3K (1 : 500, Santa Cruz Biotechnology), anti-lamin-B (1 : 500, Santa Cruz Biotechnology), anti-p-Akt (1 : 500, Santa Cruz Biotechnology), anti-Akt (1 : 1000, Santa Cruz Biotechnology). After three washes, the blots were incubated with secondary antibody (1 : 5000) for 1 h at room temperature. The proteins were visualized with an ECL (Pierce, Rockford, IL, USA). The density of the products was quantitated using image J software.
Quantitative real-time RT-PCR
Total RNA was isolated from cells by Trizol reagent (Invitrogen, Carlsbad, CA, USA). Then, 1 μg of RNA was treated by RT reagent kit (TAKARA, Dalian, China) according to the manufacturer’s instructions. Amplifications were performed using SYBR premix ex taq kit (TAKARA). The sense and antisense primers were as shown in Table 1. Each measurement was normalized to Gapdh for each sample. The relative gene expression was presented by comparative CT method.48
Insulin secretion determination
Differentiated cells at terminal day were cultured without insulin for 3 h and thoroughly washed prior to ELISA. Differentiated cells or Groups of 20 similar sized islets were pre-incubated in KRBH buffer for 1 h at 37 °C. The medium was replaced with KRBH buffer containing either 27.7 mM glucose or 5.5 mM glucose for 1 h, and then the supernatant and cells for the determination of insulin secretory ability were collected. Media samples were analyzed using Rat/Mouse insulin ELISA kit (Millipore) or human insulin ELISA kit (Millipore). Released insulin was normalized to total protein content. The insulin secretion level was presented as the ratio of insulin secretion value to INS+ cell rate. Cells were detected by flow cytometry to evaluate the ratio of INS+ cells.
Transfections with short hairpin RNAs (shRNA)
The shRNAs targeting mouse PPARβδδ, Gsk3β, Foxo1 mRNA and a negative control shRNA were purchased from Genpharma Corp (Shanghai, China) and are as follows: PPARβδδ: GGAGCATCCTCACCGGCAA and GCAGCTGGTCACTGAGCAT (1 : 1); Gsk3β: CATGAAAGTTAGCAGAGATAA; Foxo1: CGCCCCAGGTGGTGGAGAC; NC (Negative Control): GTTCTCCGAACGTGTCACGT. Digested cells at day 5+9 were transfected with either specific receptor shRNA or negative control shRNA at a final concentration of 1.6 μg/ml with Lipofectamine 2000 transfection agent (Life Technology) for 24 h according to the manufacturer's protocol. To confirm the long-term silencing effect, protein levels of PPARβδδ, Gsk3β and Foxo1 were determined by western blot at day 5+28.
Mitochondrial membrane potential (ΔΨm) assay
For the determination of ΔΨm, cells were incubated with 2 μg/ml JC-1 (5,5′,6,6′-tetrachloro-1,1′,3,3′-tetraethyl-benzimidazolylcarbocyanine iodide, Sigma Aldrich) for 30 min at 37 °C in the dark. Cells were then washed by PBS and observed under Leica DMI3000B microscope. The red fluorescent J-aggregate indicates normal ΔΨm, while the green monomer fluorescence demonstrates low ΔΨm.
Statistical analysis
Data are expressed as mean values±standard deviation (S.D.). At least three independent experiments were carried out as repeats. Statistical analysis was performed by student t-test when two groups were compared. When multiple groups were compared, ANOVA were used (GraphPad Prism 6; GraphPad Software Inc., San Diego, CA, USA). A value of P<0.05 was considered to be significant.
Abbreviations
- ES:
-
embryonic stem
- INS+:
-
insulin-positive
- GSIS:
-
glucose-stimulated insulin secretion
- PPARs:
-
peroxisome proliferator-activated receptors
- Foxo1:
-
forkhead box protein o1
- Pdx-1:
-
pancreatic and duodenal homeobox-1
- PI3K:
-
Phosphoinositide 3-kinase
- ΔΨm:
-
mitochondrial membrane potential
- shRNA:
-
small hairpin RNA
- NC:
-
negative control
- Gsk3β:
-
glycogen synthase kinase 3β
- Ngn3:
-
Neurogenin 3
- NeuroD1:
-
Neurogenic differentiation 1
- Pax4:
-
Paired box 4
- Nkx6.1:
-
NK6 homeobox 1
- Glut-2:
-
Glucose transporter 2
- ZnT8:
-
Zinc transporter 8
- protein A (avian) Mafa:
-
v-maf musculoaponeurotic fibrosarcoma oncogene family
References
Rezania A, Bruin JE, Riedel MJ, Mojibian M, Asadi A, Xu J et al. Maturation of human embryonic stem cell-derived pancreatic progenitors into functional islets capable of treating pre-existing diabetes in mice. Diabetes 2012; 61: 2016–2029.
Docherty K, Bernardo AS, Vallier L . Embryonic stem cell therapy for diabetes mellitus. Semin Cell Dev Biol 2007; 18: 827–838.
Rezania A, Bruin JE, Xu J, Narayan K, Fox JK, O'Neil JJ et al. Enrichment of human embryonic stem cell-derived NKX6.1-expressing pancreatic progenitor cells accelerates the maturation of insulin-secreting cells in vivo. Stem Cells 2013; 31: 2432–2442.
Lumelsky N, Blondel O, Laeng P, Velasco I, Ravin R, McKay R . Differentiation of embryonic stem cells to insulin-secreting structures similar to pancreatic islets. Science 2001; 292: 1389–1394.
D'Amour KA, Bang AG, Eliazer S, Kelly OG, Agulnick AD, Smart NG et al. Production of pancreatic hormone-expressing endocrine cells from human embryonic stem cells. Nat Biotechnol 2006; 24: 1392–1401.
Feige JN, Gelman L, Michalik L, Desvergne B, Wahli W . From molecular action to physiological outputs: peroxisome proliferator-activated receptors are nuclear receptors at the crossroads of key cellular functions. Prog Lipid Res 2006; 45: 120–159.
Nakamura MT, Yudell BE, Loor JJ . Regulation of energy metabolism by long-chain fatty acids. Prog Lipid Res 2014; 53: 124–144.
Poulsen L, Siersbaek M, Mandrup S . PPARs: fatty acid sensors controlling metabolism. Semin Cell Dev Biol 2012; 23: 631–639.
Evans RM, Barish GD, Wang YX . PPARs and the complex journey to obesity. Nat Med 2004; 10: 355–361.
Wang H, Xie H, Sun X, Tranguch S, Zhang H, Jia X et al. Stage-specific integration of maternal and embryonic peroxisome proliferator-activated receptor delta signaling is critical to pregnancy success. J Biol Chem 2007; 282: 37770–37782.
Choi SS, Kim ES, Koh M, Lee SJ, Lim D, Yang YR et al. A novel non-agonist peroxisome proliferator-activated receptor gamma (PPARgamma) ligand UHC1 blocks PPARgamma phosphorylation by cyclin-dependent kinase 5 (CDK5) and improves insulin sensitivity. J Biol Chem 2014; 289: 26618–26629.
Ito K, Suda T . Metabolic requirements for the maintenance of self-renewing stem cells. Nat Rev Mol Cell Biol 2014; 15: 243–256.
Xu X, Duan S, Yi F, Ocampo A, Liu GH, Izpisua BJ . Mitochondrial regulation in pluripotent stem cells. Cell Metab 2013; 18: 325–332.
Dillon JS, Yaney GC, Zhou Y, Voilley N, Bowen S, Chipkin S et al. Dehydroepiandrosterone sulfate and beta-cell function: enhanced glucose-induced insulin secretion and altered gene expression in rodent pancreatic beta-cells. Diabetes 2000; 49: 2012–2020.
Ravnskjaer K, Frigerio F, Boergesen M, Nielsen T, Maechler P, Mandrup S . PPARdelta is a fatty acid sensor that enhances mitochondrial oxidation in insulin-secreting cells and protects against fatty acid-induced dysfunction. J Lipid Res 2010; 51: 1370–1379.
Hellemans K, Kerckhofs K, Hannaert JC, Martens G, Van Veldhoven P, Pipeleers D . Peroxisome proliferator-activated receptor alpha-retinoid X receptor agonists induce beta-cell protection against palmitate toxicity. FEBS J 2007; 274: 6094–6105.
So WY, Cheng Q, Chen L, Evans-Molina C, Xu A, Lam KS et al. High glucose represses beta-klotho expression and impairs fibroblast growth factor 21 action in mouse pancreatic islets: involvement of peroxisome proliferator-activated receptor gamma signaling. Diabetes 2013; 62: 3751–3759.
Kitamura T, Ido KY . Role of FoxO proteins in pancreatic beta cells. Endocr J 2007; 54: 507–515.
Kobayashi M, Kikuchi O, Sasaki T, Kim HJ, Yokota-Hashimoto H, Lee YS et al. FoxO1 as a double-edged sword in the pancreas: analysis of pancreas- and beta-cell-specific FoxO1 knockout mice. Am J Physiol Endocrinol Metab 2012; 302: E603–E613.
Kitamura YI, Kitamura T, Kruse JP, Raum JC, Stein R, Gu W et al. FoxO1 protects against pancreatic beta cell failure through NeuroD and MafA induction. Cell Metab 2005; 2: 153–163.
Talchai C, Xuan S, Lin HV, Sussel L, Accili D . Pancreatic beta cell dedifferentiation as a mechanism of diabetic beta cell failure. Cell 2012; 150: 1223–1234.
Ohlsson H, Karlsson K, Edlund T . IPF1, a homeodomain-containing transactivator of the insulin gene. EMBO J 1993; 12: 4251–4259.
Huang W, Andras IE, Rha GB, Hennig B, Toborek M . PPARalpha and PPARgamma protect against HIV-1-induced MMP-9 overexpression via caveolae-associated ERK and Akt signaling. FASEB J 2011; 25: 3979–3988.
Yuan H, Lu J, Xiao J, Upadhyay G, Umans R, Kallakury B et al. PPARdelta induces estrogen receptor-positive mammary neoplasia through an inflammatory and metabolic phenotype linked to mTOR activation. Cancer Res 2013; 73: 4349–4361.
Pang M, de la Monte SM, Longato L, Tong M, He J, Chaudhry R et al. PPARdelta agonist attenuates alcohol-induced hepatic insulin resistance and improves liver injury and repair. J Hepatol 2009; 50: 1192–1201.
Fan W, Imamura T, Sonoda N, Sears DD, Patsouris D, Kim JJ et al. FOXO1 transrepresses peroxisome proliferator-activated receptor gamma transactivation, coordinating an insulin-induced feed-forward response in adipocytes. J Biol Chem 2009; 284: 12188–12197.
Qu S, Su D, Altomonte J, Kamagate A, He J, Perdomo G et al. PPAR{alpha} mediates the hypolipidemic action of fibrates by antagonizing FoxO1. Am J Physiol Endocrinol Metab 2007; 292: E421–E434.
Puigserver P, Rhee J, Donovan J, Walkey CJ, Yoon JC, Oriente F et al. Insulin-regulated hepatic gluconeogenesis through FOXO1-PGC-1alpha interaction. Nature 2003; 423: 550–555.
Nahle Z, Hsieh M, Pietka T, Coburn CT, Grimaldi PA, Zhang MQ et al. CD36-dependent regulation of muscle FoxO1 and PDK4 in the PPARδ/β-mediated adaptation to metabolic stress. J Biol Chem 2008; 283: 14317–14326.
Miyazaki S, Yamato E, Miyazaki J . Regulated expression of pdx-1 promotes in vitro differentiation of insulin-producing cells from embryonic stem cells. Diabetes 2004; 53: 1030–1037.
Sun Y, Zhang L, Gu HF, Han W, Ren M, Wang F et al. Peroxisome proliferator-activated receptor-alpha regulates the expression of pancreatic/duodenal homeobox-1 in rat insulinoma (INS-1) cells and ameliorates glucose-induced insulin secretion impaired by palmitate. Endocrinology 2008; 149: 662–671.
Moibi JA, Gupta D, Jetton TL, Peshavaria M, Desai R, Leahy JL . Peroxisome proliferator-activated receptor-gamma regulates expression of PDX-1 and NKX6.1 in INS-1 cells. Diabetes 2007; 56: 88–95.
Gauthier BR, Wiederkehr A, Baquie M, Dai C, Powers AC, Kerr-Conte J et al. PDX1 deficiency causes mitochondrial dysfunction and defective insulin secretion through TFAM suppression. Cell Metab 2009; 10: 110–118.
Rubin LL . Stem cells and drug discovery: the beginning of a new era? Cell 2008; 132: 549–552.
Ebert AD, Svendsen CN . Human stem cells and drug screening: opportunities and challenges. Nat Rev Drug Discov 2010; 9: 367–372.
Schroeder IS, Rolletschek A, Blyszczuk P, Kania G, Wobus AM . Differentiation of mouse embryonic stem cells to insulin-producing cells. Nat Protoc 2006; 1: 495–507.
Zhu DY, Wu JY, Li H, Yan JP, Guo MY, Wo YB et al. PPAR-beta facilitating maturation of hepatic-like tissue derived from mouse embryonic stem cells accompanied by mitochondriogenesis and membrane potential retention. J Cell Biochem 2010; 109: 498–508.
Liu Y, Tanabe K, Baronnier D, Patel S, Woodgett J, Cras-Meneur C et al. Conditional ablation of Gsk-3beta in islet beta cells results in expanded mass and resistance to fat feeding-induced diabetes in mice. Diabetologia 2010; 53: 2600–2610.
Kim HJ, Kobayashi M, Sasaki T, Kikuchi O, Amano K, Kitazumi T et al. Overexpression of FoxO1 in the hypothalamus and pancreas causes obesity and glucose intolerance. Endocrinology 2012; 153: 659–671.
Jiang W, Shi Y, Zhao D, Chen S, Yong J, Zhang J et al. In vitro derivation of functional insulin-producing cells from human embryonic stem cells. Cell Res 2007; 17: 333–344.
Iglesias J, Barg S, Vallois D, Lahiri S, Roger C, Yessoufou A et al. PPARbeta/delta affects pancreatic beta cell mass and insulin secretion in mice. J Clin Invest 2012; 122: 4105–4117.
Hock MB, Kralli A . Transcriptional control of mitochondrial biogenesis and function. Annu Rev Physiol 2009; 71: 177–203.
Nakae J, Biggs WR, Kitamura T, Cavenee WK, Wright CV, Arden KC et al. Regulation of insulin action and pancreatic beta-cell function by mutated alleles of the gene encoding forkhead transcription factor Foxo1. Nat Genet 2002; 32: 245–253.
Kitamura T, Nakae J, Kitamura Y, Kido Y, Biggs WR, Wright CV et al. The forkhead transcription factor Foxo1 links insulin signaling to Pdx1 regulation of pancreatic beta cell growth. J Clin Invest 2002; 110: 1839–1847.
Habener JF, Stoffers DA . A newly discovered role of transcription factors involved in pancreas development and the pathogenesis of diabetes mellitus. Proc Assoc Am Physicians 1998; 110: 12–21.
Stoffers DA, Thomas MK, Habener JF . Homeodomain protein IDX-1: a master regulator of pancreas development and insulin gene expression. Trends Endocrinol Metab 1997; 8: 145–151.
Li DS, Yuan YH, Tu HJ, Liang QL, Dai LJ . A protocol for islet isolation from mouse pancreas. Nat Protoc 2009; 4: 1649–1652.
Schmittgen TD, Livak KJ . Analyzing real-time PCR data by the comparative CT method. Nat Protoc 2008; 3: 1101–1108.
Acknowledgements
We are grateful to The Core Facilities of Zhejing University School of Medicine for flow cytometry analysis technical assistance. This work was supported by the National Natural Science Foundation of China (NSFC, No. 81173135, No. 91229124, No. 30973600), the Zhejiang Provincial Natural Science Foundation of China (No. LZ12H31001), and the Key Creative Team of Zhejiang Province (No. 2010R50047).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by D Aberdam
Supplementary Information accompanies this paper on Cell Death and Disease website
Supplementary information
Rights and permissions
Cell Death and Disease is an open-access journal published by Nature Publishing Group. This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Li, L., Li, T., Zhang, Y. et al. Peroxisome proliferator-activated receptorβ/δ activation is essential for modulating p-Foxo1/Foxo1 status in functional insulin-positive cell differentiation. Cell Death Dis 6, e1715 (2015). https://doi.org/10.1038/cddis.2015.88
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2015.88