Abstract
Nilotinib is a second-generation tyrosine kinase inhibitor, designed to specifically inhibit break-point cluster region (BCR)-Abelson (ABL) and developed to treat chronic myeloid leukemia (CML) in patients showing a resistance to imatinib. We previously demonstrated that nilotinib-induced apoptosis was reduced by stem cell factor (SCF) addition. Here, the SCF-activated survival pathway was investigated. BCR-ABL expression was accompanied by the activation of the SCF receptor: c-KIT. Nilotinib inhibited this activation that was restored by SCF binding. Parallel variations were observed for mammaliam target of rapamycin (mTOR) kinase and mTOR complex 1 substrate S6K. The inhibition of mTORC1 restored the response of BCR-ABL cell lines to nilotinib in the presence of SCF. PI3K inhibition restored nilotinib-induced apoptosis. On hematopoietic progenitors from CML patient’s bone marrows, mTORC1 inhibition also restored nilotinib sensitivity in the presence of SCF, confirming its involvement in SCF-activated survival pathway. However, this pathway seems not to be involved in the nilotinib-induced resistance of the CML stem cell population. Conversely, PI3K inhibition sensitized both CML progenitors and stem cells to nilotinib, suggesting that, downstream PI3K, two different kinase pathways are activated in CML progenitor and stem cell populations.
Similar content being viewed by others
Introduction
Chronic myeloid leukemia (CML) is a hematopoietic stem cell disease characterized by the presence of the chimeric break-point cluster region (BCR)-Abelson (ABL) gene, encoding a fusion protein with prominent tyrosine kinase activity.1 BCR-ABL has been identified as responsible for the leukemogenesis, leading to the development of a specific tyrosine kinase inhibitor (TKI): imatinib mesylate. In vitro, it induces apoptosis in CML cells, without affecting normal cells.2 In vivo, imatinib had totally revolutionized the treatment of CML patients, resulting in more than 80% of event-free survival after 8 years.3, 4 It currently constitutes the first-line treatment for CML patients.
Despite this efficiency, some cases of resistances appeared. Twenty per cent of them were due to a mutation in the BCR-ABL tyrosine kinase domain, resulting in imatinib inefficiency.5 To counter this resistance, nilotinib, a second-generation TKI, has been developed.6 Imatinib and nilotinib are able to inhibit specifically the ABL kinase activity, but both drugs also target other tyrosine kinases such as c-KIT (the stem cell factor (SCF) receptor) and platelet-derived growth factor receptor.7 Nilotinib is more efficient than imatinib to inhibit the BCR-ACL activity as its IC50 is 10 times lower. It is also more specific as the nilotinib concentration required to block the BCR-ABL activity, that is, 20 nM, is not sufficient to inhibit c-KIT and platelet-derived growth factor receptor, conversely to imatinib.8
In a previous in vitro study, we demonstrated that the apoptosis induced by nilotinib concentrations close to the BCR-ABL IC50 (20 nM) was reduced following SCF addition.9 The paradigm of CML cell dependence on BCR-ABL activity is questioned by these results: CML cells are able to survive after BCR-ABL inhibition if another survival pathway is activated. In addition to our work, other groups have reported that oncogenic addiction (BCR-ABL dependence) could be modified by external factors such as the microenvironment.10 In vivo, nilotinib plasmatic concentrations are 100 times higher than those necessary to inhibit the BCR-ABL activity, and probably affect other kinases such as cytokines or growth factor receptors.11 These observations promote the idea that what leads to the loss of the targeted therapy could be the key component of nilotinib success and indicate the important role of the c-KIT pathway in the response of CML cells to TKI.
The mTOR (mammalian target of rapamycin) pathway is one of the multiple signaling pathways activated by BCR-ABL in CML cells.12 mTOR is a serine/threonine kinase that forms two different complexes. The most studied complex, mTORC1, results from the binding of mTOR to Raptor, mLST8 and PRAS40. mTORC1 positively regulates the biosynthesis of proteins necessary for cell growth and proliferation. One of its main substrate is the p70-S6K. It is also known to inhibit the autophagy process. The other complex, mTORC2, is formed by the binding of mTOR to Rictor, mSIN1 and mLST8, and it is a critical regulator of AKT.13 mTOR is usually described as a member of the canonical PI3K/AKT/mTOR pathway. In CML, mTORC1 inhibition has been shown to synergize with imatinib to induce apoptosis.14 Moreover, it recently appeared that simultaneous mTORC1 and mTORC2 inhibitions could induce apoptosis in cells expressing the T315I-mutated BCR-ABL gene.15
In this study, we investigated the survival pathway activated by SCF, leading to a decrease in nilotinib-induced apoptosis. The accumulation of the pro-apoptotic protein BIM, and the decrease in the antiapoptotic protein BCL-xL, usually associated with TKI-induced apoptosis in CML cells,16, 17 were not modified after SCF addition. We observed the constitutive activation of c-KIT in BCR-ABL-expressing cell lines that was inhibited by nilotinib and restored by SCF. Parallel variations were observed for the mTOR kinase activity. Its role on SCF-activated pathway was confirmed by using RAD-001 (Everolimus), a mTORC1 inhibitor that restores nilotinib sensitivity on CML cell lines and hematopoietic progenitors (CD34+/CD38+). mTOR inhibition showed no effect on CML stem cells (CD34+/CD38−). However, PI3K inhibition restored CML cell line sensitivity to nilotinib in the presence of SCF, and this beneficial effect was also observed in both progenitors and stem cells (CD34+/CD38−).
Results
SCF inhibits nilotinib-induced apoptosis independently of BCL-2 family proteins
We previously demonstrated that SCF was able to inhibit nilotinib-induced apoptosis on BCR-ABL-expressing cells when nilotinib was used at concentrations targeting the BCR-ABL tyrosine kinase but was unable to inhibit the c-KIT tyrosine kinase.9 These results were confirmed on Figure 1a, where apoptosis induced in 24 h by 20 nM nilotinib was reduced by at least 50% in two BCR-ABL-positive cell lines and fresh CD34+cells from CML patient’s bone marrows. Moreover, the nilotinib-induced BIM accumulation and BCL-xL downregulation were not modified by the addition of SCF, whereas the cleavage of caspase 3, specific of apoptosis, was partly inhibited (Figure 1b). Similarly, ERK1/2 (extracellular signal-regulated kinases) phosphorylation, responsible for BIM degradation, was not completely restored in the presence of SCF, explaining the sustained accumulation of BIM (Figure 1c). Thus, although TKI-induced imbalance between the BCL-2 family proteins was necessary for apoptosis,16 it was not sufficient for the completion of this cell death, suggesting the inhibition of other antiapoptotic signals activated by BCR-ABL.
SCF inhibits nilotinib-induced apoptosis independently of BCL-2 family proteins. (a) Apoptosis was measured by flow cytometry using DiOC6(3) as a probe for K562 and LAMA-84 cell lines and FITC-annexin V for CML bone marrow CD34+ cells. Cells were incubated for 24 h in the presence or absence of 100 ng/ml SCF and 20 nM nilotinib. Drug-induced apoptosis was calculated as described in Materials and Methods and corrected for spontaneous apoptosis. Results are expressed as mean +/− S.D. of three experiments for the cell lines and seven experiments for the CML CD34+ cells. (b and c) K562 and LAMA-84 cells were treated with 20 nM nilotinib in the presence or absence of SCF, and the expression of BIM, BCL-xL and cleaved caspase 3 (b) or phospho-ERK1/2 and ERK (c) were analyzed by western blot. Anti-tubulin antibody was used to verify the loading homogeneity. The figure shows one representative experiment of three performed
SCF maintains the activation of the mTOR pathway without restoring the global tyrosine phosphorylation state
We first studied the effect of SCF addition on tyrosine phosphorylation. As shown in figures 2a and b, SCF could only partly restore the level of tyrosine phosphorylation after nilotinib treatment. In the same time, as expected, the SCF did not modifiy the BCR-ABL dephosphorylation induced by nilotinib. The SCF receptor c-KIT was constitutively activated in both BCR-ABL-expressing cell lines (Figure 2b). Nilotinib treatment, using low concentration (i.e., 20 nM) specific to BCR-ABL inhibition, was associated with a loss of c-KIT constitutive activation, restored in a large part after c-KIT binding by SCF (Figure 2b). Altogether, these results suggest that c-KIT constitutive phosphorylation resulted from BCR-ABL activity.
SCF maintains the activation of the mTOR pathway without restoring the global tyrosine phosphorylation state. (a) Global tyrosine phosphorylation state was measured by flow cytometry in K562 and LAMA-84 cells treated or not with 20 nM nilotinib and/or 100 ng/ml SCF for 24 h. Results are expressed in percentage of the control value. (b and c) K562 and LAMA-84 cell lysates were analyzed by western blot after treatment with nilotinib and/or SCF as described above. The blots were probed with anti-phosphotyrosine and anti-phospho-c-kit (b) or anti-phospho-c-kit, anti-phospho-mTOR and anti-phospho-S6K (c). Anti-tubulin antibody was used to verify the loading homogeneity
Among the survival pathways, putatively activated by c-KIT, mTOR has not been studied extensively. Here, we observed a constitutive mTOR phosphorylation, reduced by nilotinib and completely restored after SCF addition (Figure 2c). In the same conditions, the p70-S6K kinase completely recovered its phosphorylation state after SCF addition to nilotinib, testifying of the involvement of mTOR Complex 1 (Figure 2c). A prosurvival mechanism, activated by SCF binding to its receptor c-KIT was thus able to overcome the deleterious effect of BCR-ABL inhibition. If this mechanism is activated by the mTOR pathway, a pharmacological inhibition would restore nilotinib-induced apoptosis in the presence of SCF.
mTOR inhibitor alleviates SFC-induced resistance to nilotinib and cooperates with BCR-ABL inhibition to induce apoptosis in SCF-treated cell lines
mTORC1 inhibition was performed using RAD-001. Figure 3a shows that, in the presence of SCF, the IC50 of nilotinib was increased by a fourfold in K562 and more than seven times in LAMA-84 cell lines (dotted lines). This differential effect could be due to the higher expression of c-KIT in LAMA-84 as compared with K562 cells (supplementary Figure S1). Although RAD-001 alone had no effect (data not shown), it restored in part the IC50 of nilotinib in the presence of SCF. Similarly, SCF inhibited nilotinib-induced apoptosis more efficiently in LAMA-84 than in K562 cells (Figure 3b) and, although this inhibition was completely abolished by the mTOR inhibitor in K562 cells, it was only reduced in LAMA-84 cells. Again, this result can be related to the relative expression of c-KIT in the two cell lines (Supplementary Figure S1). Thus, it seems that in the presence of SCF, the cell lines necessitate a further inhibition of the mTOR pathway to undergo apoptosis. To support this result, we used LAMA-84 cells transduced with vector coding for shBCR-ABL and GFP or control vector (GFP alone).9 SCF addition maintained a cell survival that was inhibited in part by RAD-001 (Supplementary Figure S2). However, it is not clear from these results whether SCF-induced c-KIT activation is directly responsible for mTOR activation or whether an alternative pathway is also activated.
mTOR inhibition alleviates SFC-induced resistance to nilotinib and cooperates with BCR-ABL inhibition to induce apoptosis in SCF-treated cell lines. (a) K562 and LAMA-84 cells were seeded at 103 cells/well in 96-well plates. They were treated with increasing concentrations of nilotinib in the presence or absence of 200 nM RAD-001 and/or 100 ng/ml SCF alone or in combination as indicated. The number of viable cells was 2 evaluated after 3 days of culture on the basis of the ATP content. Results are displayed as the percentage of the untreated control value as a function of nilotinib concentration. (b) K562 and LAMA-84 cells were treated for 24 h in the presence or absence of 200 nM RAD-001Rad-001, 20 nM nilotinib, 100 ng/ml SCF alone or in combination as indicated. Apoptosis was measured by flow cytometry using DiOC6(3) as a probe. Drug-induced apoptosis was calculated as described in Materials and Methods and corrected for spontaneous apoptosis. Results are expressed as mean +/− S.D. of three experiments. (c and d) K562 (c) and LAMA-84 (d) cells were treated with 20 nM nilotinib alone or in the presence of 100 ng/ml SCF and/or 200 nM RAD-001 as indicated for 24 h. Cell lysates were then analyzed by western blot and probed with anti-phospho-c-kit, anti-phospho-mTOR and anti-phospho-S6K or anti-LC3b and anti-cleaved caspase 3 antibodies. Anti-tubulin antibody was used to verify the loading homogeneity
We analyzed the phosphorylation of c-KIT and mTOR after the inhibition of either BCR-ABL, mTOR or both (Figures 3c and d). In K562 and LAMA-84 cells, BCR-ABL inhibition resulted in the complete inhibition of c-KIT phosphorylation, whereas mTOR phosphorylation was only reduced (Figure 3c). The level of S6K phosphorylation testified of a residual mTORC1 activity. The c-KIT phosphorylation loss after the BCR-ABL inhibition was partly restored by SCF addition, whereas mTOR phosphorylation and activity were completely recovered. When both nilotinib and the mTORC1 inhibitor were used in the presence of SCF, both c-KIT and mTOR were completely unphosphorylated. Taken together, these results suggest that BCR-ABL activates c-KIT in one hand and that c-KIT and mTOR are implied in a cross-talk on the other hand.
The inhibition of mTORC1 is known to force the cells toward autophagy that can ultimately lead to cell death.18 We explored the autophagic and apoptotic cell death mechanisms by analyzing the post-translational events on the respective specific proteins LC3b and cleaved caspase 3. As shown in Figure 3d, BCR-ABL inhibition induced apoptosis, as testified by the caspase 3 cleavage and the absence of LC3b II accumulation. The simultaneous BCR-ABL/mTORC1 inhibition definitively turned the cells toward an apoptotic cell death with a caspase 3 cleavage and not toward an autophagic cell death.
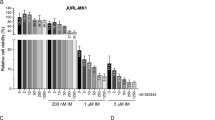
PI3K inhibitors cooperate with BCR-ABL inhibition to induce apoptosis in BCR-ABL-expressing cells
In order to identify the mechanism leading to mTOR activity, we analyzed the PI3K pathway described as the canonical pathway responsible for both AKT and mTOR activation.19 Conversely to mTOR, AKT was not dephosphorylated after BCR-ABL inhibition or phosphorylated by SCF addition (Figure 4a). However, the upstream inhibition of the PI3K using LY294002 cooperated with BCR-ABL inhibition to restore the apoptosis in the cell lines (Figure 4b). When BCR-ABL expression is inhibited by RNA interference, LY294002 addition blocked the cell rescue by SCF (Supplementary Figure S2). Moreover, PI3K and BCR-ABL inhibitors cooperated to inhibit mTOR phosphorylation and mTORC1 activity (Figure 4c), suggesting that both these pathways participated to mTOR activation. As LY294002 is not a clinically used PI3K inhibitor, we tested other PI3K inhibitors, currently involved in clinical trials. CAL-101 is a specific inhibitor of the PI3Kγ, GDC-0491 is able to inhibit the four PI3K isoforms and BEZ-235 is a dual PI3K/mTOR inhibitor. CAL-101 was not able to restore CML cell sensitivity to nilotinib in the presence of SCF (Figure 4d), conversely to GDC-0491 and BEZ-235 which induced apoptosis in a dose-dependent effect (Supplementary Figure S23).
PI3K inhibition cooperates with BCR-ABL inhibition to induce apoptosis in BCR-ABL-expressing cells. (a) K562 and LAMA-84 cells were treated or not with 20 nM nilotinib in the presence or absence of 100 ng/ml SCF for 24 h, and AKT phosphorylation was analyzed by western blot. (b and c) K562 and LAMA-84 cells were treated with nilotinib 20 nM in the presence or absence of 100 ng/ml SCF and 10 μM LY294002 as indicated. Induced apoptosis was measured and calculated as described in Figure 1a (b), and mTOR and S6K phosphorylation was analyzed by western blot (c). (d) K562 and LAMA-84 cells were treated with nilotinib 20 nM in the presence or absence of 100 ng/ml SCF and with 1 μM CAL-101 (dark grey bars) or 1 μM GDC-0491 (light grey bars) or 1 μM BEZ-235 (middle grey bars) or 10 μM LY294002 (white bars) as indicated. Induced apoptosis was measured and calculated as described in Figure 1a
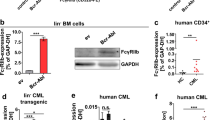
mTOR inhibitor and PI3K inhibitors cooperate with BCR-ABL inhibition to induce apoptosis in CML hematopoietic progenitors
The role of mTORC1 in the survival of BCR-ABL cells was also investigated on fresh stem/progenitor hematopoietic cells, from samples collected at the diagnosis. The analysis was gated on two distinct populations: CD34+/CD38+ and CD34+/CD38−, respectively, considered as leukemic progenitors and leukemic stem cells (Figure 5a). Nilotinib was able to significantly induce apoptosis in CD34+/CD38+ progenitor cells and this was inhibited by 60% after SCF addition (P<0.0001) (Figure 5b). As expected, nilotinib induced only a moderate apoptosis (P=0.005) on CD34+/CD38−that are more primitive cells and this effect was not inhibited by SCF (Figure 5b). In the presence of SCF, mTORC1 inhibition by RAD-001 restored in part the apoptotic response to nilotinib in CD34+/CD38+ cells (P=0.0009), whereas it failed to sensitize the CD34+/CD38−cells (Figure 5b). The combination treatment Nilo/RAD was more efficient than the sum of separate effects (calculated) for 6 on 9 samples (Supplementary Figure S4). Nilotinib and RAD-001 showed no cytotoxic effect on BCR-ABL-negative CD34+cells (Figure 5d and Supplementary Figure S5a). Thus, the mTORC1 pathway has a role in the survival of BCR-ABL-expressing cells and its inhibition partially overcomes the SCF-induced resistance to nilotinib. Conversely, the previously described resistance of primitive progenitor and stem cells to TKI10 is not dependent on mTORC1 activity. The ability of PI3K inhibition to restore CML cells sensitivity to nilotinib in the presence of SCF was confirmed in CML CD34+/CD38+cells in which LY294002-induced apoptosis was further increased when LY294002 was associated with nilotinib (P=0.001) (Figure 5e ). Contrary to CML cell lines, all the PI3K inhibitors tested are able to restore CML cells sensitivity to nilotinib in the presence of SCF. Interestingly, an apoptotic response was also induced in the primitive CD34+/CD38−population which has been found resistant to BCR-ABL inhibitors used alone or in combination with an mTOR inhibitor. This result suggests that a different signaling pathway is responsible for the survival in the different CD34+subpopulations. The PI3K inhibitor showed a cytotoxic effect on BCR-ABL-negative progenitors, but to a lesser extent than on their CML counterparts, and, as expected, did not synergize with nilotinib (Figure 5f and Supplementary Figure S5B).
mTOR inhibition and PI3K inhibition cooperates with BCR-ABL inhibition to induce apoptosis in hematopoietic progenitors. (a–d) Mononuclear cells from 15 CML bone marrows (a and b) and 7 BCR-ABL negative and 2 healthy donors (c and d) were treated for 24 h with 20 nM nilotinb and/or 200 nM RAD-001 in the presence or absence of 100 ng/ml SCF. Cells were then labeled with FITC-annexin V, PC5-anti CD34 and APC-anti CD38 and analyzed by flow cytometry (a). The percentage of apoptotic cells was measured as annexin V-binding cells after gating on CD34+/CD38+ (black bars) and CD34+/CD38− (grey bars) populations (b). For BCR-ABL-negative cells, the gating was performed on the whole-CD34+ cells (c). Charts represent the percentage of drug-specific apoptosis calculated as described in a Figure 1a (d). (e and f) Mononuclear cells from 10 CML bone marrows were treated with 1 μM CAL-101 (dark grey bars) or 1 μM GDC-0491 (light grey bars) or 1 μM BEZ-235 (middle grey bars) or 10 μM LY294002 (white bars) as indicated for 24 h and/or with20 nM nilotinb in the presence or absence of 100 ng/ml SCF. Cells were then labeled and analyzed by flow cytometry as described in Figure 5A. The percentage of apoptotic cells was measured as annexin V-binding cells after gating on CD34+/CD38+ and CD34+/CD38− populations (e). Mononuclear from 86 BCR-ABL-negative cells were treated or not with 20 nM nilotinib and/or 10 μM LY294002 for 24 h, in the presence of SCF at 100 ng/ml (f), the gating was performed on the whole-CD34+ cells
Discussion
In the current work, we confirmed that cytokines, and particularly the SCF, are able to counteract the pro-apoptotic effect induced by the BCR-ABL inhibition. We have investigated the survival pathways activated by the SCF receptor, c-KIT, to better understand this phenomenon. As mTOR complexes could be activated by c-KIT, and have already been reported to regulate cell growth and proliferation in CML cells, we focused our work on this pathway. Moreover, mTOR complexes could also be targeted by several small inhibitors in the development for cancer therapy.20, 21 We observed that mTORC1 inhibition restores nilotinib sensitivity in the presence of SCF, in both CML cell lines and progenitors. mTORC1 inhibitor did not induce any beneficial effect on CML stem cells and conversely to PI3K inhibitors that sensitize this TKI-resistant population to nilotinib.
In a first set of experiments, we had reported that the SCF/c-KIT pathway must be inhibited to enable TKI-induced apoptosis in CML cells.9 The impact of external factors on TKI response must be highly considered. Similarly to our results, two studies have recently demonstrated that growth factors could confer a TKI resistance in other models and particularly in solid tumors such as melanomas or non-small cell lung cancer.22, 23 In addition, Corbin et al.10 have reported that cytokines, such as SCF, produced by the microenvironment, could counter the TKI inhibitory effects in CML cells.
We confirm in this study, that the c-KIT pathway is really a hindrance to the TKI inhibitory effect. The relevance of this data is supported by the constitutive activation of c-KIT observed in CML cell lines. A direct link between c-KIT and BCR-ABL had already been reported.24 Here, we confirm that BCR-ABL activates c-KIT, as BCR-ABL inhibition by low doses of nilotinib (20 nM) was associated with a loss of c-KIT phosphorylation. The binding of SCF to c-KIT restores in part its phosphorylation in the absence of BCR-ABL activity and this effect results in mTORC1 activation. mTORC1 activity is necessary to the anti-TKI effect of SCF, as it was abrogated after mTORC1 inhibition with RAD-001. In other words, the protective and restorative effect of SCF on nilotinib-induced apoptosis is lost after mTORC1 inhibition with RAD-001. Several studies have previously reported a role for the mTOR pathway in CML cells. It has recently been shown that the rapamycin-induced mTOR inhibition decreased the proliferation of K562 cell lines.25 Moreover, clinical and preclinical studies have demonstrated that mTORC1 inhibitors synergized with imatinib to increase apoptosis in CML cells26, 27 and restored the sensitivity to imatinib-resistant cells.14
We observed a link between the mTOR functional effect and c-KIT expression level, that is, in high c-KIT-expressing cell lines, the mTOR inhibition was less efficient (see Figures 3c and d and Supplementary Figure S1). Moreover, when BCR-ABL and mTOR inhibitors were used in combination, the phosphorylation of c-KIT and mTOR was more reduced than when each inhibitor was used separately (see Figures 4a and b). This result suggests that c-KIT and mTOR are engaged in a cross-talk.
The upstream events leading to mTOR activation, following SCF binding, were investigated and it was found that the PI3K activity was implied. The mTOR inhibition was sufficient to overcome the protective effect of SCF on nilotinib-induced apoptosis in both CML cell lines and progenitors. However, it was inefficient to induce apoptosis in CD34+/CD38− CML cells which were also resistant to BCR-ABL inhibition.10, 28 Conversely, the PI3K inhibitors alone were able to induce apoptosis in CD34+/CD38−CML stem cells, illustrating different survival mechanisms in progenitors and stem cells (Figure 6). We observed that all the PI3K inhibitors tested were able to induce apoptosis by themselves in CML stem cells and this was increased after nilotinib addition, except for the dual PI3K/mTOR inhibitor BEZ-235. This last result suggests that, in a population for which BCR-ABL activity is not required by itself for the survival, nilotinib indirectly inhibited the mTOR kinase, explaining its inability to synergize with a dual PI3K/mTOR inhibitor, whereas it did synergize with PI3K inhibitors.
Survival pathways in CML progenitors and stem cells. In Bcr-Abl-expressing cell lines and CML progenitors, the binding of SCF to its receptor activates the PI3K pathway resulting in mTOR and Akt activation. In the absence of Bcr-Abl activity, the inhibition of mTOR is sufficient to induce cell death. In stem cells, survival is less dependent on the Bcr-Abl activity and was not affected by the mTOR inhibition. The activation of the c-kit/PI3K pathway is sufficient to sustain cell survival
BCR-ABL is a ‘super-tyrosine kinase’ able to activate several survival signaling pathways. Its inhibition by imatinib or nilotinib results in a consecutive inhibition of downstream effectors like PI3K/mTOR pathway. In this study, we observed that despite BCR-ABL inhibition, SCF is able to maintain a survival in CML cells mediated by PI3K/mTOR pathway. Thus, it appears that SCF is able to overcome nilotinib-induced apoptosis through a BCR-ABL-independent mechanism, undermining the concept of oncogenic addiction.
It must be noticed that nilotinib is currently used to treat CML but that administrated doses lead to plasma concentrations able to inhibit c-KIT besides BCR-ABL, as shown already with the other TKI, that is, imatinib and dasatinib.29, 30, 31 This result questions the concept of the so-called ‘targeted therapy’ of CML, and suggests that TKI success could be the result of multiple kinase inhibitions, such as at least BCR-ABL and c-KIT, induced by high dose administrations. Finally, the mTORC1 inhibition could help in reducing nilotinib dosing at levels that only inhibit BCR-ABL with no effect on c-KIT, and it would be worth to test this combination in CML patients
However, nilotinib/RAD-001 association is not able to resolve one of the most important problems in CML therapy: the TKI resistance of leukemic stem cells. The inhibition of the PI3K/AKT pathway could thus be another promising strategy for this last purpose. Several studies have already shown a main role of PI3K in BCR-ABL-induced transformation.32 Here, we identified PI3K as a component of the CML stem cell resistance to TKI. This mechanism has to be taken into account to design a drug combination able to induce cell death on both CML progenitors and stem cells while sparing normal hematopoietic progenitors. Several strategies have already been proposed to target leukemic stem cells,33 and the combination of TKI and PI3K inhibitors should be considered if we want to cure CML and stop the treatment.
Materials and methods
Cell lines
K562 and LAMA-84 cell lines were cultured in RPMI 1640 supplemented with 10% v/v fetal calf serum, 1 mM glutamine, 25 mM Hepes, 100 units/ml penicillin, 50 μg/ml streptomycin in a humidified atmosphere containing 5% v/v CO2 at 37 °C. Exponentially growing cells were used in all experiments.
Bone marrow samples
After informed consent was obtained, bone marrow samples obtained from patients with myeloproliferative disorders that were received in the laboratory for BCR-ABL analysis were separated by Ficoll sedimentation (PAN Biotech GmbH, Aidenbach, Germany). The CML samples have been collected at the time of diagnosis, before any treatment. Copland et al.34 have shown that at diagnosis, around 93% of CD34+ cells and 96% of CD34+CD38− expressed BCR-ABL. Moreover, normal bone marrow samples were taken from non-hematological patients after informed consent. The mononuclear cell layer was washed and resuspended in culture medium in the presence of the drugs.
Reagents
Nilotinib (AMN107, Tasigna) was kindly provided by Novartis Pharma (Bâle, Switzerland) and used at 20 nM. RAD-001 (Everolimus, Novartis), CAL-101 (Calistoga/Gilead, Foster City, CA, USA), BEZ-253 (Novartis), GDC-0491 (Roche, Meylan, France) were purchased to Selleck (Munich, Germany) and used at 200 nM for RAD-001 and 1 μM for the others. LY294002 (Cell Signaling Technology, Danvers, MA, USA) was used at 10 μM. The SCF was purchased from Peprotech (Neuilly sur Seine, France) and used at 100 ng/ml, as usually added for in vitro experimentation.35
Apoptosis in K562 and LAMA-84 cell lines
Apoptosis was detected using DiOC6(3) (100 ng/ml) as a probe for mitochondrial membrane potential as previously described.36 Samples were analyzed with an Epics XL cytometer (Beckman Coulter, Villepinte, France).
Apoptosis in primary bone marrow cells
After a 24-h incubation with the indicated drugs, mononuclear cells, from CML patient bone marrows or BCR-ABL-negative bone marrows, were labeled with anti CD34-APC, anti CD38-PC5 and Annexin V-FITC. Samples were analyzed by multivariate flow cytometry (Navios, Beckman Coulter). Percentages of annexin V-positive cells were quantified on the gated CD34+/CD38+ or CD34+/CD38 populations, and considered as apoptotic.
Cell viability
Cells were seeded at 25 000 cells/well in a 96-well plate and cultured for 3 days with increasing concentrations of nilotinib in the presence or absence of SCF (100 ng/ml) and RAD-001 (200 nM). Viable cells were evaluated on the basis of their ATP content. The CellTiter-Glo luminescent viability assay (Promega, Charbonnières, France) was used according to the supplier’s instructions. The bioluminescence was read using a Wallac 1420 Victor luminometer (Perkin Elmer, Courtaboeuf, France).
Western blot
After SDS-PAGE electrophoresis, proteins were transferred onto a PVDF membrane (Biorad, Marnes-la-Coquette, France). Membranes were saturated with 5% (w/v) fat-free dry milk or 5% (w/v) bovine albumin in Tris-buffered saline containing 0.1% (v/v) Tween-20 (Sigma, Lyon, France). Membranes were then probed with primary antibodies: mouse monoclonal for BCL-xL (Santa Cruz Biotech, Dallas, TX, USA) and phospho-tyrosine (P-Tyr-100) (Cell Signaling Technology), rabbit monoclonal for cleaved caspase 3, phospho-AKT (Thr308), phospho-AKT (Ser473), p44/42 MAPK (Erk1/2), phospho-p44/42 MAPK (Erk1/2) (Thr202/204) (Cell Signaling Technology Inc.), and phospho-S6K (Thr389) (Abcam, Cambridge, UK) and rabbit polyclonal for: Tubulin, BIM, LC3B (Sigma), phospho-c-KIT (Abcam) and phospho-mTOR (Ser2448) (Invitrogen, Saint-Aubin, France).
All antibodies were used at a 1/1000 dilution. After secondary antibody labeling, peroxidase activity was revealed using the western Lightning Plus-ECL kit (Perkin Elmer) and band intensity was quantified using a Kodak Imager.
Assessment of tyrosine phosphorylations by flow cytometry
CML cell lines were resuspended at 250 000 cells/ml in culture medium and untreated (control cells) or treated with nilotinib (20 nM), SCF (100 ng/ml) or both. After a 24-h incubation at 37 °C, cells were washed with PBS and fixed with 4% formaldehyde. Permeabilization was performed using methanol 50% in PBS. After washing, the cells were labeled with the desired phospho-specific antibody and an Alexa-647-coupled secondary antibody (Invitrogen). A negative control was performed for each experiment by using an unrelated primary antibody.
Statistical analysis
All experiments performed on cell lines were carried out in triplicate and results expressed as the mean±S.D. The paired Student’s t-test was used to analyze the data. Considering the wide range of spontaneous apoptosis occurring during the culture of patient samples, drug-induced apoptosis was calculated as the percentage of drug-specific apoptosis: (apoptosis in treated sample−apoptosis in control) × 100 divided by (100−apoptosis in control). Experiments performed on patient samples were analyzed for significance using the Wilcoxon test for paired samples.
Abbreviations
- CML:
-
chronic myeloid leukemia
- TKI:
-
tyrosine kinase inhibitor
- SCF:
-
stem cell factor
- BCR:
-
break-point cluster region
- ABL:
-
Abelson
- mTOR:
-
mammaliam target of rapamycin
- PDGFR:
-
platelet-derived growth factor receptor
- ERK:
-
extracellular signal-regulated kinases
References
Deininger MW, Goldman JM, Melo JV . The molecular biology of chronic myeloid leukemia. Blood 2000; 96: 3343–3356.
Deininger MW, Goldman JM, Lydon N, Melo JV . The tyrosine kinase inhibitor CGP57148B selectively inhibits the growth of BCR-ABL-positive cells. Blood 1997; 90: 3691–3698.
Druker BJ, Talpaz M, Resta DJ, Peng B, Buchdunger E, Ford JM et al. Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med 2001; 344: 1031–1037.
Deininger M, O'Brien SG, Guilhot F, Goldman JM, Hochhaus A, Hughes TP et al. International randomized study of interferon vs STI571 (IRIS) 8-year follow up: sustained survival and low risk for progression or events in patients with newly diagnosed chronic myeloid leukemia in chronic phase (CML-CP) treated with imatinib. ASH Annual Meeting Abstracts 2009; 114: 1126-.
Jabbour E, Kantarjian H, Jones D, Talpaz M, Bekele N, O'Brien S et al. Frequency and clinical significance of BCR-ABL mutations in patients with chronic myeloid leukemia treated with imatinib mesylate. Leukemia 2006; 20: 1767–1773.
Kantarjian HM, Giles F, Gattermann N, Bhalla K, Alimena G, Palandri F et al. Nilotinib (formerly AMN107), a highly selective BCR-ABL tyrosine kinase inhibitor, is effective in patients with Philadelphia chromosome-positive chronic myelogenous leukemia in chronic phase following imatinib resistance and intolerance. Blood 2007; 110: 3540–3546.
Buchdunger E, Cioffi CL, Law N, Stover D, Ohno-Jones S, Druker BJ et al. Abl protein-tyrosine kinase inhibitor STI571 inhibits in vitro signal transduction mediated by c-kit and platelet-derived growth factor receptors. J Pharmacol Exp Ther 2000; 295: 139–145.
Weisberg E, Manley PW, Breitenstein W, Bruggen J, Cowan-Jacob SW, Ray A et al. Characterization of AMN107, a selective inhibitor of native and mutant Bcr-Abl. Cancer Cell 2005; 7: 129–141.
Belloc F, Airiau K, Jeanneteau M, Garcia M, Guerin E, Lippert E et al. The stem cell factor-c-KIT pathway must be inhibited to enable apoptosis induced by BCR-ABL inhibitors in chronic myelogenous leukemia cells. Leukemia 2009; 23: 679–685.
Corbin AS, Agarwal A, Loriaux M, Cortes J, Deininger MW, Druker BJ . Human chronic myeloid leukemia stem cells are insensitive to imatinib despite inhibition of BCR-ABL activity. J Clin Invest 2011; 121: 396–409.
Deininger MW . Nilotinib. Clin Cancer Res: 2008; 14: 4027–4031.
Ly C, Arechiga AF, Melo JV, Walsh CM, Ong ST . Bcr-Abl kinase modulates the translation regulators ribosomal protein S6 and 4E-BP1 in chronic myelogenous leukemia cells via the mammalian target of rapamycin. Cancer Res 2003; 63: 5716–5722.
Gentzler RD, Altman JK, Platanias LC . An overview of the mTOR pathway as a target in cancer therapy. Expert Opin Ther Targets 2012 e-pub ahead of print 12 April 2012.
Sillaber C, Mayerhofer M, Bohm A, Vales A, Gruze A, Aichberger KJ et al. Evaluation of antileukaemic effects of rapamycin in patients with imatinib-resistant chronic myeloid leukaemia. Eur J Clin Invest 2008; 38: 43–52.
Carayol N, Vakana E, Sassano A, Kaur S, Goussetis DJ, Glaser H et al. Critical roles for mTORC2- and rapamycin-insensitive mTORC1-complexes in growth and survival of BCR-ABL-expressing leukemic cells. Proc Natl Acad Sci USA 2010; 107: 12469–12474.
Belloc F, Moreau-Gaudry F, Uhalde M, Cazalis L, Jeanneteau M, Lacombe F et al. Imatinib and nilotinib induce apoptosis of chronic myeloid leukemia cells through a Bim-dependant pathway modulated by cytokines. Cancer Biol Ther 2007; 6: 912–919.
Horita M, Andreu EJ, Benito A, Arbona C, Sanz C, Benet I et al. Blockade of the Bcr-Abl kinase activity induces apoptosis of chronic myelogenous leukemia cells by suppressing signal transducer and activator of transcription 5-dependent expression of Bcl-xL. J Exp Med 2000; 191: 977–984.
Kamada Y, Funakoshi T, Shintani T, Nagano K, Ohsumi M, Ohsumi Y . Tor-mediated induction of autophagy via an Apg1 protein kinase complex. J Cell Biol 2000; 150: 1507–1513.
Guertin DA, Sabatini DM . Defining the role of mTOR in cancer. Cancer Cell 2007; 12: 9–22.
Faivre S, Kroemer G, Raymond E . Current development of mTOR inhibitors as anticancer agents. Nat Rev Drug Discov 2006; 5: 671–688.
Fasolo A, Sessa C . Current and future directions in mammalian target of rapamycin inhibitors development. Expert Opin Investig Drugs 2011; 20: 381–394.
Straussman R, Morikawa T, Shee K, Barzily-Rokni M, Qian ZR, Du J et al. Tumour micro-environment elicits innate resistance to RAF inhibitors through HGF secretion. Nature 2012; 487: 500–504.
Wilson TR, Fridlyand J, Yan Y, Penuel E, Burton L, Chan E et al. Widespread potential for growth-factor-driven resistance to anticancer kinase inhibitors. Nature 2012; 487: 505–509.
Hallek M, Danhauser-Riedl S, Herbst R, Warmuth M, Winkler A, Kolb HJ et al. Interaction of the receptor tyrosine kinase p145c-kit with the p210bcr/abl kinase in myeloid cells. Br J Haematol 1996; 94: 5–16.
Li J, Xue L, Hao H, Han Y, Yang J, Luo J . Rapamycin provides a therapeutic option through inhibition of mTOR signaling in chronic myelogenous leukemia. Oncol Rep 2012; 27: 461–466.
Mohi MG, Boulton C, Gu TL, Sternberg DW, Neuberg D, Griffin JD et al. Combination of rapamycin and protein tyrosine kinase (PTK) inhibitors for the treatment of leukemias caused by oncogenic PTKs. Proc Natl Acad Sci USA 2004; 101: 3130–3135.
Mancini M, Corradi V, Petta S, Martinelli G, Barbieri E, Santucci MA . mTOR inhibitor RAD001 (Everolimus) enhances the effects of imatinib in chronic myeloid leukemia by raising the nuclear expression of c-ABL protein. Leukemia Res 2010; 34: 641–648.
Hamilton A, Helgason GV, Schemionek M, Zhang B, Myssina S, Allan EK et al. Chronic myeloid leukemia stem cells are not dependent on Bcr-Abl kinase activity for their survival. Blood 2012; 119: 1501–1510.
Apperley JF, Gardembas M, Melo JV, Russell-Jones R, Bain BJ, Baxter EJ et al. Response to imatinib mesylate in patients with chronic myeloproliferative diseases with rearrangements of the platelet-derived growth factor receptor beta. N Engl J Med 2002; 347: 481–487.
Akin C, Fumo G, Yavuz AS, Lipsky PE, Neckers L, Metcalfe DD . A novel form of mastocytosis associated with a transmembrane c-kit mutation and response to imatinib. Blood 2004; 103: 3222–3225.
Chen Z, Lee FY, Bhalla KN, Wu J . Potent inhibition of platelet-derived growth factor-induced responses in vascular smooth muscle cells by BMS-354825 (dasatinib). Mol Pharmacol 2006; 69: 1527–1533.
Skorski T, Bellacosa A, Nieborowska-Skorska M, Majewski M, Martinez R, Choi JK et al. Transformation of hematopoietic cells by BCR/ABL requires activation of a PI-3k/Akt-dependent pathway. EMBO J 1997; 16: 6151–6161.
Airiau K, Mahon FX, Josselin M, Jeanneteau M, Turcq B, Belloc F . ABT-737 increases tyrosine kinase inhibitor-induced apoptosis in chronic myeloid leukemia cells through XIAP downregulation and sensitizes CD34(+) CD38(-) population to imatinib. Exp Hematol 2012; 40: 367–78 e2.
Copland M, Hamilton A, Elrick LJ, Baird JW, Allan EK, Jordanides N et al. Dasatinib (BMS-354825) targets an earlier progenitor population than imatinib in primary CML but does not eliminate the quiescent fraction. Blood 2006; 107: 4532–4539.
Gidali J, Laszlo E, Halm G, Feher I . Blast colony-forming cell binding from CML bone marrow, or blood, on stromal layers pretreated with G-CSF or SCF. Cell Prolif 2002; 35: 1–7.
Vayssiere JL, Petit PX, Risler Y, Mignotte B . Commitment to apoptosis is associated with changes in mitochondrial biogenesis and activity in cell lines conditionally immortalized with simian virus 40. Proc Natl Acad Sci USA 1994; 91: 11752–11756.
Acknowledgements
We thank Novartis for providing Nilotinib. This work was supported by grants from BMS and la Ligue contre le cancer. Kelly Airiau received a grant from the French Ministry of Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by Y Shi
Supplementary Information accompanies this paper on Cell Death and Disease website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Airiau, K., Mahon, FX., Josselin, M. et al. PI3K/mTOR pathway inhibitors sensitize chronic myeloid leukemia stem cells to nilotinib and restore the response of progenitors to nilotinib in the presence of stem cell factor. Cell Death Dis 4, e827 (2013). https://doi.org/10.1038/cddis.2013.309
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2013.309
Keywords
This article is cited by
-
Multifaceted role of mTOR (mammalian target of rapamycin) signaling pathway in human health and disease
Signal Transduction and Targeted Therapy (2023)
-
Apatinib exhibits synergistic effect with pyrotinib and reverses acquired pyrotinib resistance in HER2-positive gastric cancer via stem cell factor/c-kit signaling and its downstream pathways
Gastric Cancer (2021)
-
Expression differences of miR-142-5p between treatment-naïve chronic myeloid leukemia patients responding and non-responding to imatinib therapy suggest a link to oncogenic ABL2, SRI, cKIT and MCL1 signaling pathways critical for development of therapy resistance
Experimental Hematology & Oncology (2020)
-
An in vivo genome-wide CRISPR screen identifies the RNA-binding protein Staufen2 as a key regulator of myeloid leukemia
Nature Cancer (2020)
-
DYRK2 controls a key regulatory network in chronic myeloid leukemia stem cells
Experimental & Molecular Medicine (2020)