Abstract
Inflammatory bowel disease (IBD), which consists of Crohn's disease (CD) and ulcerative colitis (UC), is a chronic, inflammatory disorder of the gastro-intestinal tract with unknown etiology. Current evidence suggests that intestinal epithelial cells (IECs) is prominently linked to the pathogenesis of IBD. Therefore, maintaining the intact of epithelium has potential roles in improving pathophysiology and clinical outcomes of IBD. MicroRNAs (miRNAs) act as post-transcriptional gene regulators and regulate many biological processes, including embryonal development, cell differentiation, apoptosis and proliferation. In this study, we found that miR-200b decreased significantly in inflamed mucosa of IBD, especially for UC, when compared with their adjacent normal tissue. Simultaneously, we also found that the genes of E-cadherin and cyclin D1 were reduced significantly and correlated positively to the miR-200b. In addition, the upregulation of transforming growth factor-beta 1 (TGF-β1) was inversely correlated to the miR-200b in IBD. To investigate the possible roles of miR-200b in IECs maintaining, we used TGF-β1 to induce epithelial-mesenchymal transition (EMT) in IEC-6 initially. After sustained over-expressing miR-200b in IEC-6, the EMT was inhibited significantly that was characterized by downregulation of vimentin and upregulation of E-cadherin. Furthermore, we found that miR-200b enhanced E-cadherin expression through targeting of ZEB1, which encode transcriptional repressors of E-cadherin. SMAD2 was found to act as a target of miR-200b with direct evidence that miR-200b binding to the 3′ UTR of SAMD2 and the ability of miR-200b to repress SMAD2 protein expression. With SMAD2 depletion, the expression of vimentin decreased correspondingly, which suggested miR-200b might reduce vimentin through regulating the SMAD2. With endogenous over-expression of miR-200b, the proliferation of IEC-6 cells increased significantly by increasing S-phase entry and promoting expression of the protein cyclin D1. Summarily, our study suggested a potential role for mir-200b in maintaining intact of intestinal epithelium through inhibiting EMT and promoting proliferation of IECs.
Similar content being viewed by others
Main
Inflammatory bowel disease (IBD), mainly referring to the Crohn’s disease (CD) and ulcerative colitis (UC), is usually caused by a combination of genetic, immunological, bacterial and environmental factors.1, 2, 3, 4 There is increasing evidence that loss of intestinal epithelial cells (IECs) acts as one of the major contributors to the pathogenesis of IBD. An intact monolayer of IECs, the largest areas that are exposed to and react with the external environment protects the body from pathogens and other toxic luminal substances.5, 6, 7, 8 IBD patients often demonstrate increased intestinal paracellular permeability and decreased intestinal epithelial barrier function, which is mainly resulted from a loss of tight junction and epithelial cell loss.6, 9, 10, 11, 12 Therefore, maintaining intact of epithelium is a potential strategy for IBD therapy.
The process of epithelial-mesenchymal transition (EMT) is characterized by losing epithelial cell marker such as E-cadherin, and gaining of a mesenchymal phenotype with expression of mesenchymal proteins including vimentin.13, 14 Briefly, EMT allows a polarized epithelial cell, which normally interacts with basement membrane via its basal surface, to undergo multiple biochemical changes that enable it to a mesenchymal cell phenotype, which enhances migratory capacity, invasiveness and greatly increased production of cell-extracellular matrix components.15 Recent studies demonstrated that EMT contributes to the pathogenesis of IBD, especially to the loss of IECs, based on the clinical analysis and animal experiments.16, 17 Therefore, inhibiting EMT has potential roles in improving clinical outcomes of IBD.
MicroRNAs (miRNAs) are non-coding RNA molecules (21–23 nucleotides long) regulate gene expression at the post-transcriptional level by base pairing with specific sequences (miRNA response element) in the 3′ UTR of target mRNAs causing degradation of mRNA or inhibition of translation.18 The members of miR-200 family have been highlighted for its importance in the maintenance of the epithelial phenotype through repressing EMT by directly targeting and downregulating ZEB1 and ZEB2, resulting in enhanced E-cadherin expression.19, 20 In the present study, we identify that downregulation of miR-200b expression is associated with loss of IECs in IBD. And then, we use a model of EMT to tackle the questions of whether and how miR-200b ameliorates intestinal epithelial barrier function in vitro.
Results
The miR-200b decreases in IBD
To investigate whether miR-200b participates in the pathogenesis of IBD, we performed real-time PCR to quantify the expression of miR-200b in biopsy specimens of IBD initially. A total of 22 IBD patients (11 with CD and 11 with UC) have been enrolled in this study. Five patients with colonic polyps, which pathologically confirmed benign adenoma, served as non-IBD controls. The clinical features of subjects were showed in the Supplementary Table 1. In patients with the active phase of IBD, the expression of miR-200b (175±90) was significantly lower (P=0.018) when compared with controls (261±134). We further divided IBD into CD and UC and analyzed the expression of miR-200b in them. We found that the miR-200b decreased significantly in affected tissues compared with adjacent controls in UC patients (144±72 versus 271±127, P=0.010). However, the expression of miR-200b in lesions and adjacent tissues has no significant difference in CD patients (206±99 versus251±146, P=0l.416). In the non-IBD controls, the expression of miR-200b in the lesion did not differ from adjacent controls (228±89 versus 243±120, P=0.613) (Figure 1).
miR-200b was down-regulated in IBD. The expression of mir-200b decreased by about twofold in 22 IBD tissues when compared with the matched controls. In Ulcerative Colitis (UC, N=11) miR-200b was reduced significantly in inflamed mucosa. However, there was no significant changes in Crohn's Disease (CD, N=11). In patients with colonic adenoma, acting as the non-IBD controls, it neither found any significant changes of miR-200b in lesion of colon when compared with adjacent normal controls. *P<0.05; **P<0.01
The downregulation of miR-200b correlates with the injury of IECs in IBD
IBD patients often have damages in IECs, which are linked to a disturbed intestinal homeostasis and barrier function. As we known, E-cadherin is required for the maintenance of architecture and function of the intestinal epithelium. In this study, the CDH1, gene of E-Cadherin, decreased significantly in the inflamed mucosa compared with adjacent normal control (28±67 versus 119±121, P=0.002). (Figure 2) In addition, immunohistochemistry analysis revealed that E-cadherin protein was also reduced significantly. (Supplementary Figure 1 and Supplementary Table 1) Pearson correlation and linear regression analysis showed that miR-200b was closely related to CDH1. (R=0.47, P=0.02) (Figure 2) Once epithelial cells lose polarity by lacking of E-cadherin, they often decide to become mesenchymal-like cells. Vimentin, a marker for mesenchymal cell, increased significantly in inflamed mucosa of IBD (14.5±3.4 versus 5.2±6.2, P=0.001). (Figure 2) This result was also enhanced by immunohistochemistry analysis. As shown in the Supplementary Figure1, the levels of vimentin protein increased significantly simultaneously. However, no obvious correlation was found between miR-200b and vimentin (R=−0.15, P=0.36) (Figure 2). The balance of proliferation and death of IECs is another important factor to maintain the intestinal epithelium homeostasis. Here, we detected the expression of PCNA (proliferating cell nuclear antigen) and CCND1 in these IBD specimens with real-time PCR. PCNA is a marker of human colonic cell proliferation, and CCND1, encodes cyclin D1 that is required for cell cycle G1/S transition.21 As shown in the Figure 3, the mRNA of CCND1 reduced significantly in UC (0.18±0.2 versus 0.89±1.4, P=0.004), but not in CD (0.54±0.63 versus 0.70±0.86, P=0.291). In addition, CCND1 was correlated significantly with miR-200b. For expression of PCNA mRNA in IBD, there was no significant change could be found. (Figure 3)
The miR-200b was significantly correlated with E-cadherin in IBD. The expression of CDH1 (gene of E-cadherin) was reduced significantly in inflamed mucosa of IBD, especially in UC. Pearson correlation and linear regression analysis indicated that miR-200b was correlated significantly to CDH1 (R=0.47, i=0.02). Conversely, the gene of Vimentin increased in lesion tissues of IBD, but had no significant relationship with miR-200b (R=−0.15, P=0.36). *P<0.05, **P<0.01
miR-200b was correlated positively with CCND1 and negatively with TGF-β1 in IBD. As markers of cell proliferation, the genes of CCND1 and PCNA were detected and quantified. It found that CCND1 was downregulated significantly in IBD. Pearson correlation and linear regression analysis showed that CCND1 was correlated significantly to miR-200b. TGF-β1 was upregulated significantly and correlated negatively with miR-200b. *P<0.05, **P<0.01
Enforced expression of the miR-200b prevents TGF-β1-induced EMT
EMT is a process characterized by loss of epithelial markers, gain of mesenchymal markers and changes in cellular morphology and phenotype with increased ability to migrate. The above findings suggested that EMT contributed to the injury of intestinal epithelial barrier in IBD. As an important inducer of EMT, TGF-β1 was detected and analyzed in these samples, and the correlation between TGF-β1 and miR-200b was also analyzed. As shown in Figure 3, TGF-β1 increased significantly in both UC and CD lesions (UC, 12.5±13.6 versus 5.6±10.1, P=0.025; CD, 3.6±4.3 versus 1.2±1.8, P=0.004) and significantly correlated with miR-200b (R= −0.36, P=0.03).
To explore whether miR-200b has therapeutic potential in improving intestinal homeostasis, we employed lentiviral-based microRNA system to establish a stable cell line with miR-200b over-expression. (Supplementary Figure 2) Fluorescence microscopic analysis showed that lentiviral particles tagged with red fluorescent protein (RFP) infected IEC-6 effectively, with adequate RFP expressing in cells. Figure 4a showed that expression of miR-200b increased by around 2400-folds in lentiviral-RFP-200b compared with the lentivrial-RFP infected cells. Moreover, the expression of miR-200b was suppressed continuously in respond to TGF-β1. (Figure 4a)
The expression of miR-200b was inhibited by TGF-β1. In respond to stress of TGF-β1, the expression of miR-200b was reduced significantly in both lentiviral-vector and lentiviral-miR-200b infected cells. (a) The cell-cell junction disappeared and was became scatter in respond to the TGF-β1 including, while, miR-200b protected these cells from losing polarity. (b) *P<0.05, **P<0.01. Magnified × 100
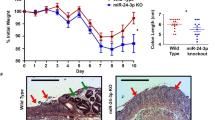
In this study, we induced EMT in IEC-6 cells by exposure to 10 ng/ml human TGF-β1 as reported previously.17 We showed that TGF-β1 treatment could lead IEC-6 cells to undergo EMT-like transformation evidenced by loss of cell-cell adhesion and alterations of morphology from a round compact shape to a spindle shape. (Figure 4b) Immunofluorescent labeling and western-blots demonstrated a phenotypic transition from an epithelial morphology toward mesenchymal-like properties evidenced by loss of the epithelial marker, E-cadherin and in turn increased expression of the mesenchymal marker, vimentin. With miR-200b over-expressed in IEC-6 cells, we observed that miR-200b could inhibit the process of EMT by increasing E-cadherin and decreasing vimentin. (Figure 5)
miR-200b inhibited TGF-β1-induced EMT. Western-blot and immunochemistry analysis showed that TGF-β1 could induce EMT in IEC-6 cells by repression of E-cadherin expression, and increased expression of vimentin at the indicated time. With miR-200b over-expressing in IEC-6 cells, this process of EMT was inhibited significantly (a). Immunochemistry analysis indicated that showed endogenous over-expression of miR-200b decreased the vimentin and increased the E-cadherin at the seventh day of TGF-β1 inducing. (b) Arrows indicated the staining of E-cadherin or vimentin, Magnified × 200
TGF-β1 is a pleiotropic cytokine with important effects on a wide range of cells and processes, including wound healing/tissue remodeling, being profibrotic, proangiogenic and antiproliferative.22, 23 Typically, TGF-β1 affected genes expression through the SMAD transcription factors. Briefly, once TGF-β1 bind to its heterodimeric receptor I or II, the receptor phosphorylates SMAD2 and SMAD3, which then combine with SMAD4 and translocate to the nucleus to induce or repress the expression of several genes.24 With using bioinformatics tool TargetScanHuman 6.2 (http://www.targetscan.org), miR-200b was predicted to target SMAD2 at position of 334–340 sites of its 3′ UTR. The dual luciferase reporter assay showed miR-200b repressed the activity of luciferase significantly, which provided evidence of a direct link between miR-200b and human SMAD2 (Figure 6a). We simultaneously demonstrated that the levels of phospho-SMAD2 were reduced because of miR-200b downregulation of total SMAD2 protein levels (Figure 6b). After depletion of SMAD2 with RNA interference, we found that protein of vimentin was reduced correspondingly. ZEB1 was not only regarded as a transcriptional repressor of E-cadherin, but also of a direct target of miR-200b.25, 26, 27 Here, we demonstrated that the expression of ZEB1 decreased significantly and resulted in upregulating of E-cadherin expression in miR-200b over-expressed cells. (Figure 6b)
MiRNA-200b targeted SMAD2 and modulated response to TGF-β1.The putative binding site of miR-200b at position of 334-340 in SMAD2 3′-UTR region was predicted by TargetScan 6.2 (http://www.targetscan.org). Expression of the firefly luciferase reporter activity was significantly reduced by sustained expression of miR-200b. Western-blot analysis also showed that the expression of SMAD2 protein decreased significantly by endogenous over-expression of miR-200b. (a) After SMAD2 knocked down, the expression of vimentin was decreased evidently. The over-expression of miR-200b inhibited expression of ZEB1 significantly. (b)
MiR-200b promotes proliferation of IECs
The intestinal epithelium is a dynamic tissue characterized by a high rate of cell death and reproduction, leading to renewal of the entire intestinal epithelium every 3–5 days.28 Patients with IBD have been demonstrated increased apoptosis of the acute inflammatory sites throughout the entire crypt-villus axis.29, 30 Sartor et al.24 reported that aberrant of immune activation and overproduction of inflammatory cytokines induced death of intestinal epithelial cells in IBD. Therefore, promoting IEC proliferation was necessary to replenish the decreased cell pool and further to ameliorate epithelial barrier function. Here, we demonstrated that proliferation of IEC-6 was increased significantly with endogenous miR-200b over-expression. In addition, TGF-β1-induced IEC-6 cells growth inhibition was partially reversed by sustained expression of miR-200b. (Figure 7a) With flow cytometry analysis, we observed that the over-expression of miR-200b altered the cell cycle by increasing S-phase and decreasing G1 phase significantly. Moreover, we found that the cyclin D1 protein expression was promoted by miR-200b over-expression. (Figures 7b and c)
miR-200b promoted the proliferation of IECs. The growth of IEC-6 was suppressed by TGF-β1. While, with miR-200b over-expressing in IEC-6 cells, the proliferation was promoted significantly. (a) Cell-cycle analysis showed that cells infected with lentiviral-miR-200b had increased numbers of cells in S phase and corresponding decreased numbers of cells in G1 phase. (b) miR-200b upregulated the expression of Cyclin D1. (c) *P<0.05; **P<0.01
Discussion
Currently, it remained unclear about the etiology and pathogenesis of IBD. Evidences from the animals and human have been demonstrated that loss of IECs contributed to the tissue damage and the severity of colonic inflammatory response. Therefore, maintaining intact of epithelium may provide novel and effective strategies to treat IBD.31 At the center of intestinal barrier, IECs, has an active role in producing mucus and providing a physical barrier capable of controlling antigen traffic through the intestinal mucosa. Injuries/defects of IECs have been shown to increase epithelial permeability in IBD, which has been shown to possibly caused relapse.32, 33, 34
The EMT, characterized by losing of epithelial markers and the acquisition of mesenchymal morphological markers, has aroused extensive interest in IBD research recently.17, 35, 36 The EMT contributes to the disassembly of tight junctions and loss of apical-basal polarity in IECs due to a repression of the transmembrane adhesion receptor E-cadherin and a gain in expression of the mesenchymal features. The gene of E-cadherin (CDH1) has been reported to be associated with pathogenesis of IBD, with patients possessing the disease-associated single nucleotide polymorphisms having increased E-cadherin cytoplasmic accumulation.37
In this study, we found that the expression of E-cadherin decreased in the inflamed mucosa of IBD compared with the adjacent controls at both mRNA and protein levels. On the contrary, the expression of vimentin mRNA increased significantly. (Figure 2 and Supplementary Figure 1) Therefore, it was reasonable that EMT inhibition was a potential approach to protect IECs from injuring. We first found that miR-200b reduced significantly in IBD, and correlated significantly with E-cadherin. (Figures 1 and 2) It reminded us that enhanced miR-200b expression in epithelium of IBD might resist to the loss of tight junctions and polarity in IECs. Indeed, we demonstrated that sustained over-expression of miR-200b in IEC-6 cells decreased TGFβ1-mediated EMT significantly by repressing expression of vimentin and robust expression of E-cadherin. ZEB1, a known transcriptional repressor of E-cadherin and a direct target gene of miR-200b, was decreased by miR-200b. These data suggested over-expression of miR-200b promoted E-cadherin through disrupting the ZEB1. (Figure 5) SMAD2 has been reported to act as a target gene of miR-200b in regulating mammalian palate development.38 Here, dual-luciferase and western-blot analysis provided direct evidence that miR-200b binded to 3′ UTR of SMAD2 hence repressed SMAD2 protein expression in IEC-6 cells. As one important mediator in TGF-β1 signaling, SMAD2 was involved in TGF-β1-mediated EMT.39, 40, 41 In this study, we found that expression of vimentin was decreased correspondingly after SMAD2 knocked down (Figure 6). It suggested that miR-200b might inhibit expression of vimentin through TGF-β1-SMAD2 signal pathway.
The intestinal epithelium is a dynamic tissue characterized by renewal of the entire intestinal epithelium every 3–5 days in mice.28 A balance between cellular proliferation and death is necessary to maintain the normal function of IECs. We found that the CCND1, gene of Cyclin D1, was decreased significantly in IBD, and positively related to the miR-200b in these specimens. (Figure 3) With endogenous over-expression of miR-200b, we found that proliferation of IEC-6 cells was increased significantly by increasing S-phase and decreasing G1 phase. In proliferative cells, the cell cycle consists of four phases. Passage through the four phases of the cell cycle is regulated by a family of cyclins that act as regulatory subunits for cyclin-dependent kinases (cdks). The cyclin-cdk-complex of G1/S is either cdk4 or cdk6 bound to a cyclin D isoform. Here, we demonstrated miR-200b could promote the expression of cyclin D1 protein. This finding was consistent with a report previously, which demonstrated that miR-200b increased cyclin D1 expression by targeting RND3 in HeLa cells.42
Materials and Methods
Reagents
Reagents were used in this study as followed: IEC-6 cell line (American Type Culture Collection, ATCC), Phospho-Smad Antibody Sampler Kit (Cell Signaling, Danvers, MA, USA), Human Transforming Growth Factor β1 (Cell Signaling), Epithelial-Mesenchymal Transition (EMT) Antibody Sample kit (Cell Signaling); Anti-E-cadherin antibody (BD Biosciences, San Diego, CA, USA); Has-mir-200b inhibitor, SMAD2 siRNA (GenePharma Inc, Shanghai, China), Cyclin D1 (Bioworld, Dublin, OH, USA), Cell Counting Kit-8, DAPI (Dojindo, Kumamoto, Japan), has-mir-200b TaqMan MicroRNA Assays (Applied Biosystems, Foster City, CA, USA)
Specimens
The use of human tissue in this study was approved by the Ethics Committee at the Xinhua Hospital, Shanghai, China. A total of 27 biopsy mucosal samples and their adjacent controls were obtained from endoscopic specimens of patients with diagnosis of IBD (CD, N=11; UC, N=11) and tubulovillous adenoma of the colon (N=5). Briefly, 5 × 5 mm mucosal tissues were obtained during colonoscopy. Adjacent controls were obtained from the sites that distanced 5–10 cm from inflamed area in the same patients. All of the patients or their guardians provided written informed consent. Specimens were paraffin-embedded or stored at −80 °C. The diagnosis was based on established clinical, endoscopic, histological parameters. Tissue specimens were assessed microscopically by two pathologists (M, Z and W, Z). All samples considered active showed the typical characteristics of inflamed IBD and demonstrated histological parameters such as increased mononuclear infiltrates accompanied by active lesion such as erosions/ulcerations or crypt abscesses/cryptitis. Diagnostic findings of the patients are provided in Supplementary Table 1 and Supplementary Figure 1.
Immunohistochemistry and immunofluorescence assay
Immunohistochemistry was performed using method of diaminobenzidine (DAB) chromogen as described previously.35 Briefly, tissue samples were incubated with xylol and descending concentrations of ethanol. Antigen retrieval was performed using citrate buffer, pH 6.0 (microwave treatment, 40 min at 240 W). Endogenous peroxidases were removed by incubation with 0.3% H2O2 for 15 min at room temperature (RT) and blocking was performed using 5% bovine serum albumin (BSA) for 1 h at RT. Primary antibodies were then applied in an optimal concentration overnight in a wet chamber. (N-cadherin, dilution 1:200; E-cadherin, dilution 1:200; vimentin dilution 1:100). After incubation for 30 min at 37 °C following overnight at 4 °C, the slides were rinsed in phosphate-buffered saline (PBS) and incubated with the secondary antibody for 1 h at RT. Antibody binding was visualized by a liquid DAB Substrate Chromogen System (Dako, Glostrup, Denmark). The slides were rinsed in PBS and counterstained with hematoxylin. The evaluation of immunohistochemical pattern was performed in blinded fashion by a pathologist (M, Z) experienced in IBD. For immunofluorescence analysis, the cells were fixed with 4% paraformaldehyde initially. After blocking cell with 3% BSA for half an hour at RT, the cells were incubated with the anti-E-cadherin antibody or anti-Vimentin antibody at RT for 2 h. After washing three times with PBS, the second antibody conjugated with FITC was performed on these cells for 1 h at RT. The nuclei were counterstained with DAPI.
Cell culture and lentivirus production
The small intestinal cell line IEC-6 was grown in Dulbecco's modified Eagle's medium (DMEM) supplemented with 10% heat-inactivated fetal bovine serum (FBS).
Lentivirus infection was commenced when the IEC-6 cells were either at 40–60% confluence. The EMT was induced by conditioned medium DMEM supplemented with 0.5% FBS containing TGF-β1 (10 ng/ml) as described previously.43 For constructing the miR-200b-lentivirus, the sequence of miR-200b precursor was inserted into pGCSIL vector with enzymes Age I/ EcoR I. The combined plasmid was transfected into 293T cells. After 48 h, the supernatant was collected by centrifugation at 4000 r.p.m. for 10 min. The debris were removed by filtering with 0.45 μm filter. The titer of lentiviral vectors was determined by fluorescence-activated cell sorting.
Real-time PCR
The total RNA was extracted from the cells or tissues with Trizol (Invitrogen, Carlsbad, CA, USA) according to the protocol of manufacture. For determining the expression of miR-200b, miR-200b was reverse transcribed and quantified with a TaqMan microRNA assays (Applied Biosystems). All data were normalized to U6. For genes assay, SYBR-Green Universal Master Mix kit and High Capacity cDNA Reverse Transcription kit (Applied Biosystems) were employed to detect the levels of these genes. All reactions were repeated three times and GAPDH was used to normalize the target genes. The PCR primers: GAPDH, forward, 5′-GAAGGTGAAGGTCGGAGTC-3′, reverse, 5′-GAAGATGGTGATGGGATTTC-3′; CDH1, forward, 5′-GGAGGAGAGCGGTGGTCAAA-3′, reverse, 5′-TGTGCAGCTGGCTCAAGTCAA-3′; vimentin, forward, 5′-CCTCCTACCGCAGGATGTT-3′, reverse, 5′-CTGCCCAGG CTGTAGGTG-3′; CCND1, Forward 5'-CACACGGACTACAGGGGAGT-3′, reverse, 5′-CACAGGAGCTGGTGTTCCAT-3′; PCNA, Forward 5′-AGGCACTCAAGGACCTCATCA-3′, reverse, 5′-GAGTCCATGCTCTGCAGGTTT-3′ and TGF-β1, Forward 5′-GCACGTGGAGCTGTACCA-3′ reverse, 5′-CAGCCGGTTGCTGAGGTA-3′.
Western blots
Western blots were performed using standard procedures. Briefly, protein of 30 μg/well was separated on 4–12% SDS-polyacrylamide gels and transferred onto nitrocellulose using a dry blotting system (iBLOT system, Invitrogen). After blocking in PBS, 5% nonfat milk at RT for 30 min, membranes were incubated with the primary antibodies overnight at 4 °C. The primary antibodies of E-cadherin, Vimentin, SMAD2, ZEB1 and cyclin D1 were performed in this study. The membranes were washed three times with PBS and 0.1% Tween-20, and then incubated with secondary antibodies. After final washes with PBS and 0.1% Tween-20, the signals were detected using ECL chemiluminescence reagents. (Pierce, Rockford, IL, USA).
Flow cytometric and proliferative analysis
Cells were seeded in 96-well plates with 30–50% confluence initially. The proliferation of IEC-6 cells was analyzed using the Cell Counting Kit-8 (Dojindo) after 24 or 48 h. The absorbance value of each well was determined at 450 nm by a microplate reader (Beckman Coulter Instruments, Brea, CA, USA). IEC-6 cells were fixed with ice-cold 70% ethanol, labeled with PI, and cell cycle was detected by flow cytometry as described before.44
Luciferase reporter assay
The 3′-UTR for SMAD2 was amplified from genomic DNA. Amplified 3′ UTRs were cloned to the downstream of luciferase coding region in the pGL3 vector (Promega, Madison, WI, USA). 400 ng pGL-SMAD2 plasmids were transfected into IEC-6 cells with lentiviral-vector/lentiviral-miR-200b infection by using Lipofectamine-2000 (Invitrogen, Inc). Cells were harvested for luciferase activity assays 48 h after transfection. The relative reporter activity was obtained by normalization to the Renilla control luciferase activity.
Statistical analysis
All data are reported as mean ±S.D. When comparisons were made between two different groups, statistical significance was determined by the Student’s t-test using SPSS19 software program. P values from a two-tailed test were <0.05 were considered statistically significant. Pearson correlation and linear regression analysis were used to assess correlation between miR-200b and CDH1, Vimentin, TGF-β1, CCND1 and PCNA.
Abbreviations
- IBD:
-
Inflammatory bowel disease
- CD:
-
Crohn’s disease
- UC:
-
ulcerative colitis
- miRNA:
-
microRNA
- IECs:
-
intestinal epithelial cells
- EMT:
-
epithelial-mesenchymal transition
- UTR:
-
untranslated regions
- TGF-β1:
-
transforming growth factor-beta1
- PCNA:
-
proliferating cell nuclear antigen
References
Khor B, Gardet A, Xavier RJ . Genetics and pathogenesis of inflammatory bowel disease. Nature 2011; 474: 307–317.
Strober W, Fuss IJ . Proinflammatory cytokines in the pathogenesis of inflammatory bowel diseases. Gastroenterology 2011; 140: 1756–1767.
Xavier RJ, Podolsky DK . Unravelling the pathogenesis of inflammatory bowel disease. Nature 2007; 448: 427–434.
Abraham C, Cho JH . IL-23 and autoimmunity: new insights into the pathogenesis of inflammatory bowel disease. Annu Rev Med 2009; 60: 97–110.
Feng BS, Chen X, Li P, Zheng PY, Chong J, Cho DB et al. Expression of integrin alphavbeta6 in the intestinal epithelial cells of patients with inflammatory bowel disease. N Am J Med Sci 2009; 1: 200–204.
McCole DF . Regulation of epithelial barrier function by the inflammatory bowel disease candidate gene, PTPN2. Ann N Y Acad Sci 2012; 1257: 108–114.
Kaser A, Autophagy BlumbergRS . microbial sensing, endoplasmic reticulum stress, and epithelial function in inflammatory bowel disease. Gastroenterology 2011; 140: 1738–1747.
Siccardi D, Turner JR, Mrsny RJ . Regulation of intestinal epithelial function: a link between opportunities for macromolecular drug delivery and inflammatory bowel disease. Adv Drug Deliv Rev 2005; 57: 219–235.
Petit CS, Barreau F, Besnier L, Gandille P, Riveau B, Chateau D et al. Requirement of cellular prion protein for intestinal barrier function and mislocalization in patients with inflammatory bowel disease. Gastroenterology 2012; 143: 122–132 e115.
Gadaleta RM, van Erpecum KJ, Oldenburg B, Willemsen EC, Renooij W, Murzilli S et al. Farnesoid X receptor activation inhibits inflammation and preserves the intestinal barrier in inflammatory bowel disease. Gut 2011; 60: 463–472.
Hering NA, Schulzke JD . Therapeutic options to modulate barrier defects in inflammatory bowel disease. Dig Dis 2009; 27: 450–454.
Laukoetter MG, Nava P, Nusrat A . Role of the intestinal barrier in inflammatory bowel disease. World J Gastroenterol 2008; 14: 401–407.
Cano A, Perez-Moreno MA, Rodrigo I, Locascio A, Blanco MJ, del Barrio MG et al. The transcription factor snail controls epithelial-mesenchymal transitions by repressing E-cadherin expression. Nat Cell Biol 2000; 2: 76–83.
Auersperg N, Pan J, Grove BD, Peterson T, Fisher J, Maines-Bandiera S et al. E-cadherin induces mesenchymal-to-epithelial transition in human ovarian surface epithelium. Proc Natl Acad Sci USA 1999; 96: 6249–6254.
Kalluri R, Neilson EG . Epithelial-mesenchymal transition and its implications for fibrosis. J Clin Invest 2003; 112: 1776–1784.
Scharl M, Weber A, Furst A, Farkas S, Jehle E, Pesch T et al. Potential role for SNAIL family transcription factors in the etiology of Crohn’s disease-associated fistulae. Inflamm Bowel Dis 2011; 17: 1907–1916.
Flier SN, Tanjore H, Kokkotou EG, Sugimoto H, Zeisberg M, Kalluri R . Identification of epithelial to mesenchymal transition as a novel source of fibroblasts in intestinal fibrosis. J Biol Chem 2010; 285: 20202–20212.
Winter J, Jung S, Keller S, Gregory RI, Diederichs S . Many roads to maturity: microRNA biogenesis pathways and their regulation. Nat Cell Biol 2009; 11: 228–234.
Vandewalle C, Comijn J, De Craene B, Vermassen P, Bruyneel E, Andersen H et al. SIP1/ZEB2 induces EMT by repressing genes of different epithelial cell-cell junctions. Nucleic Acids Res 2005; 33: 6566–6578.
Gregory PA, Bert AG, Paterson EL, Barry SC, Tsykin A, Farshid G et al. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat Cell Biol 2008; 10: 593–601.
Kubben FJ, Peeters-Haesevoets A, Engels LG, Baeten CG, Schutte B, Arends JW et al. Proliferating cell nuclear antigen (PCNA): a new marker to study human colonic cell proliferation. Gut 1994; 35: 530–535.
Gorelik L, Flavell RA . Immune-mediated eradication of tumors through the blockade of transforming growth factor-beta signaling in T cells. Nat Med 2001; 7: 1118–1122.
Massague J . How cells read TGF-beta signals. Nat Rev Mol Cell Biol 2000; 1: 169–178.
Massague J, Wotton D . Transcriptional control by the TGF-beta/Smad signaling system. EMBO J 2000; 19: 1745–1754.
Dave N, Guaita-Esteruelas S, Gutarra S, Frias A, Beltran M, Peiro S et al. Functional cooperation between Snail1 and twist in the regulation of ZEB1 expression during epithelial to mesenchymal transition. J Biol Chem 2011; 286: 12024–12032.
Gill JG, Langer EM, Lindsley RC, Cai M, Murphy TL, Kyba M et al. Snail and the microRNA-200 family act in opposition to regulate epithelial-to-mesenchymal transition and germ layer fate restriction in differentiating ESCs. Stem Cells 2011; 29: 764–776.
Kim T, Veronese A, Pichiorri F, Lee TJ, Jeon YJ, Volinia S et al. p53 regulates epithelial-mesenchymal transition through microRNAs targeting ZEB1 and ZEB2. J Exp Med 2011; 208: 875–883.
Hall PA, Coates PJ, Ansari B, Hopwood D . Regulation of cell number in the mammalian gastrointestinal tract: the importance of apoptosis. J Cell Sci 1994; 107: 3569–3577.
Hagiwara C, Tanaka M, Kudo H . Increase in colorectal epithelial apoptotic cells in patients with ulcerative colitis ultimately requiring surgery. J Gastroenterol Hepatol 2002; 17: 758–764.
Iwamoto M, Koji T, Makiyama K, Kobayashi N, Nakane PK . Apoptosis of crypt epithelial cells in ulcerative colitis. J Pathol 1996; 180: 152–159.
Ellis RE, Yuan JY, Horvitz HR . Mechanisms and functions of cell death. Annu Rev Cell Biol 1991; 7: 663–698.
Clayburgh DR, Shen L, Turner JR . A porous defense: the leaky epithelial barrier in intestinal disease. Lab Invest 2004; 84: 282–291.
Soderholm JD, Olaison G, Lindberg E, Hannestad U, Vindels A, Tysk C et al. Different intestinal permeability patterns in relatives and spouses of patients with Crohn's disease: an inherited defect in mucosal defence? Gut 1999; 44: 96–100.
Porras M, Martin MT, Yang PC, Jury J, Perdue MH, Vergara P . Correlation between cyclical epithelial barrier dysfunction and bacterial translocation in the relapses of intestinal inflammation. Inflamm Bowel Dis 2006; 12: 843–852.
Bataille F, Rohrmeier C, Bates R, Weber A, Rieder F, Brenmoehl J et al. Evidence for a role of epithelial mesenchymal transition during pathogenesis of fistulae in Crohn’s disease. Inflamm Bowel Dis 2008; 14: 1514–1527.
Chen Y, Ge W, Xu L, Qu C, Zhu M, Zhang W et al. miR-200b is involved in intestinal fibrosis of Crohn’s disease. Int J Mol Med 2012; 29: 601–606.
McGovern DP, Gardet A, Torkvist L, Goyette P, Essers J, Taylor KD et al. Genome-wide association identifies multiple ulcerative colitis susceptibility loci. Nat Genet 2010; 42: 332–337.
Shin JO, Lee JM, Cho KW, Kwak S, Kwon HJ, Lee MJ et al. MiR-200b is involved in Tgf-beta signaling to regulate mammalian palate development. Histochem Cell Biol 2012; 137: 67–78.
Kolosova I, Nethery D, Kern JA . Role of Smad2/3 and p38 MAP kinase in TGF-beta1-induced epithelial-mesenchymal transition of pulmonary epithelial cells. J Cell Physiol 2011; 226: 1248–1254.
Lv ZD, Kong B, Li JG, Qu HL, Wang XG, Cao WH et al. Transforming growth factor-beta 1 enhances the invasiveness of breast cancer cells by inducing a Smad2-dependent epithelial-to-mesenchymal transition. Oncol Rep 2013; 29: 219–225.
Li Y, Kang X, Wang Q . HSP70 decreases receptor-dependent phosphorylation of Smad2 and blocks TGF-beta-induced epithelial-mesenchymal transition. J Genet Genomics 2011; 38: 111–116.
Xia W, Li J, Chen L, Huang B, Li S, Yang G et al. MicroRNA-200b regulates cyclin D1 expression and promotes S-phase entry by targeting RND3 in HeLa cells. Mol Cell Biochem 2010; 344: 261–266.
Zeisberg M, Yang C, Martino M, Duncan MB, Rieder F, Tanjore H et al. Fibroblasts derive from hepatocytes in liver fibrosis via epithelial to mesenchymal transition. J Biol Chem 2007; 282: 23337–23347.
Iredale JP, Benyon RC, Pickering J, McCullen M, Northrop M, Pawley S et al. Mechanisms of spontaneous resolution of rat liver fibrosis. Hepatic stellate cell apoptosis and reduced hepatic expression of metalloproteinase inhibitors. J Clin Invest 1998; 102: 538–549.
Acknowledgements
This study is supported by National Natural Science Foundation of China (81270455), Key Scientific Research Program of Shanghai Health Bureau (2010005), Funding of Xinhua hospital (11QYJ010), Shanghai Key Laboratory of Pediatric Gastroenterology (11DZ2260500) and Shanghai Municipal Education Commission Special Research Fund for Excellent Young College and University Teachers (ZZjdyx12095).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by A Stephanou
Supplementary Information accompanies the paper on Cell Death and Disease website
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Chen, Y., Xiao, Y., Ge, W. et al. miR-200b inhibits TGF-β1-induced epithelial-mesenchymal transition and promotes growth of intestinal epithelial cells. Cell Death Dis 4, e541 (2013). https://doi.org/10.1038/cddis.2013.22
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2013.22
Keywords
This article is cited by
-
Bovine Milk Derived Exosomes Affect Gut Microbiota of DSS-Induced Colitis Mice
Indian Journal of Microbiology (2024)
-
lncRNA H-19 and miR-200a implication and frequency of lncRNA H-19 rs2170425 SNP in ulcerative colitis and Crohn’s disease
Comparative Clinical Pathology (2023)
-
miR-200b-3p alleviates TNF-α-induced apoptosis and inflammation of intestinal epithelial cells and ulcerative colitis progression in rats via negatively regulating KHDRBS1
Cytotechnology (2021)
-
microRNAs as therapeutic targets in intestinal diseases
ExRNA (2019)
-
Epithelial–mesenchymal transition in Crohn's disease
Mucosal Immunology (2018)