Abstract
β-1, 4-Galactosyltransferase gene (B4GALT) family consists of seven members, which encode corresponding enzymes known as type II membrane-bound glycoproteins. These enzymes catalyze the biosynthesis of different glycoconjugates and saccharide structures, and have been recognized to be involved in various diseases. In this study, we sought to determine the expressional profiles of B4GALT family in four pairs of parental and chemoresistant human leukemia cell lines and in bone marrow mononuclear cells (BMMC) of leukemia patients with multidrug resistance (MDR). The results revealed that B4GALT1 and B4GALT5 were highly expressed in four MDR cells and patients, altered levels of B4GALT1 and B4GALT5 were responsible for changed drug-resistant phenotype of HL60 and HL60/adriamycin-resistant cells. Further data showed that manipulation of these two gene expression led to increased or decreased activity of hedgehog (Hh) signaling and proportionally mutative expression of p-glycoprotein (P-gp) and MDR-associated protein 1 (MRP1) that are both known to be related to MDR. Thus, we propose that B4GALT1 and B4GALT5, two members of B4GALT gene family, are involved in the development of MDR of human leukemia cells, probably by regulating the activity of Hh signaling and the expression of P-gp and MRP1.
Similar content being viewed by others
Main
Glycosyltransferases (GTs) catalyze the transfer of sugar moieties from activated donor molecules to specific acceptor molecules that determines the biosynthesis of glycans. In recent years, glycosylation changes in disease symptoms and development have been explored intensively.1 It has shown that oligosaccharide expression may be associated with carcinogenesis, metastasis and development of chemoresistance of malignant cells.2, 3, 4 Although the alterations of glycan structures are observed in drug resistance leukemia cells,5, 6 there is limited report about the effects of GTs and corresponding glycogenes in the development of leukemia drug resistance.
B4GalT gene family encodes a set of type II transmembrane glycoproteins that transfer galactose in a β-1, 4 linkage to similar acceptor sugars. There are seven members of the β-1, 4-galactosyltransferase (β1, 4-Gal-T1) family, all of which are expressed in a tissue-specific manner.7 As a house keeping enzyme, β1, 4-Gal-T1 is thought to be the key enzyme to have important roles in many biological events, including morphogenesis, mammalian fertilization, brain development, cellular adhesion, and so on.8, 9, 10, 11 Abnormal expression of β1, 4-Gal-T has been shown to be implicated in a number of diseases12, 13, 14, 15, and levels of cell surface β1, 4-Gal-T could be influenced by many factors. Literatures show that estrogen and arachidonic acid promote proliferation and cell adhesion of human breast cancer cells by inducing β1, 4-Gal-T1 expression.13, 16 In embryonic stem cells, β1, 4-Gal-T1 expression is regulated by a novel ubiquitin-conjugating enzyme accounting for intercellular adhesion and embryonic development.17 B4GALT is also identified as an apoptosis-related gene in some cancer cells and contributes to the activation of signal transduction pathways.18
The hedgehog (Hh) signaling pathway consists of a series of proteins that are necessary for embryogenesis, cell development and proliferation. To date, tremendous evidence indicates that Hh signaling activation might be associated with a wide variety of human tumors. The key signal molecules of Hh network are recognized as oncogenes, such as smoothened (Smo), sonic hedgehog (Shh) and glioma-associated oncogene (Gli-1).19 Furthermore, several reports indicate that aberrant activation of Hh pathway leads to the survival and drug resistance of different types of human cancer cells.20 Specific inhibition of the Hh pathway may therefore be an effective therapeutic strategy for overcoming treatment resistance of malignant tumors, for example, upregulation of Gli-1 is correlated with glioma recurrence after chemotherapy, and blocking the Hh pathway activity elevates chemosensitivity of glioma cells.21 In leukemic cells, chemoresistance is shown to be maintained by Hh signaling activation, and could be reversed by cyclopamine, a known Hh antagonist.22
A number of studies have focused on the mechanisms of acquired multidrug resistance (MDR) of leukemia cells. Among these, permeability glycoprotein, also known as ATP-binding cassette (ABC) subfamily B member 1, is a contributing factor for MDR. Xenobiotic compounds are transported outside the cell by this protein depending on ATP. Under physiological conditions, p-glycoprotein (P-gp) protects the body against harmful substances through inhibiting drugs reabsorption and keeping the integrity of the blood–brain barrier. In cancer stem cells with MDR, P-gp is responsible for the medicines clearance and promotes the development of chemoresistance.23
MDR-associated protein 1 (MRP1) is another member of ABC transporters, which transports anticancer drugs across cellular membranes and reduces drug accumulation in the cells. MRP1 is closely involved in MDR in several types of cancer.24 Elevated level of MRP1 is often found in various malignant cells before drug treatment.
We previously identified that B4GALT1 gene enhanced the activity of Hh signaling and promoted MDR in K562/adriamycin-resistant (ADR) cell line.25 In current study, we established the expressional profiles of B4GALT gene family in four pairs of parental and chemoresistant human leukemia cell lines and in BMMC of leukemia patients with MDR. Overexpression of B4GALT1 and B4GALT5 had been observed in all these MDR cells and cases. On the basis of these findings, we further elucidated the possible mechanisms of action of these two genes in MDR.
Results
B4GALT1 and B4GALT5 are upregulated in four ADR leukemia cell lines
Here, we performed real-time PCR and western blotting in order to search for abnormally expressed genes and proteins of B4GALT family in four ADR cell lines. Remarkable increases of B4GALT1 and B4GALT5 were observed in four drug-resistant leukemia cells at both gene and protein levels compared with those of four drug-sensitive parental cell lines. No significant changes of the rest members of B4GALT family were shown between parent cell lines and their ADR cells. B4GALT6 gene was absent in HL/60, NB4, U937 cells and their ADR sublines, while B4GALT4 and B4GALT7 were undetectable only in U937 and U937/ADR cell lines (Figures 1a–h).
B4GALT1 and B4GALT5 are upregulated at both mRNA and protein levels in four chemoresistant human leukemia cell lines. (a–d) The mRNA levels of B4GALT gene family were detected by real-time PCR. Four ADR cells expressed higher levels of B4GALT1 and T5 mRNA than their parental cell types (*P<0.05). B4GALT6 gene was not detectable in HL/60, NB4, U937 cells and their ADR sublines, while B4GALT4 and B4GALT7 were absent in U937 and U937/ADR cell lines. (e–h) By western blot, β1, 4-Gal-T1 and T5 proteins were found to be highly expressed in four ADR cells compared with those of parental cells (*P<0.05), expressions of the rest enzymes of β1, 4-Gal-T family were also consistent with mRNA levels
Suppression of B4GALT1 or B4GALT5 gene enhances chemosensitivity of HL60/ADR cells in vitro and in vivo
To investigate the impacts of B4GALT1 and B4GALT5 on drug resistance of leukemia cells, HL60/ADR cells were treated with B4GALT1 or B4GALT5 shRNA, respectively. As shown in Figures 2a–d, the expression levels of B4GALT1 and B4GALT5 were significantly reduced in HL60/ADR-shRNA transfectants compared with control transfectants.
Either B4GALT1 or B4GALT5 silencing facilitates HL60/ADR cells sensitive to therapeutic drugs. (a and b) B4GALT1 and B4GALT5 transcripts were decreased apparently in HL60/ADR cells by shRNA treatment. (c and d) After shRNA transfection, distinct reduction of B4GALT1 or B4GALT5 was observed at protein levels by western blot analysis. (e and f) In vitro MTS assay revealed that IC50 values of three drugs were decreased with the inhibition of B4GALT1 or B4GALT5 in HL60/ADR cells. (g and h) When exposed to adriamycin, the tumor volume of nude mice bearing HL60/ADR-B4GALT1 shRNA or HL60/ADR-B4GALT5 shRNA xenograft was significantly diminished. (i and j) Downregulation of B4GALT1 or T5 was also shown by IHC staining in xenograft tumors derived from HL60/ADR-B4GALT1 shRNA or HL60/ADR-B4GALT5 shRNA cells ( × 400). For a–f, i and j, asterisk denotes significant reduction from the groups without an asterisk (P<0.05), for g and h, *P<0.05
After B4GALT1 or B4GALT5 shRNA transfection, the ability of adriamycin, paclitaxel and vincristine to inhibit the growth of HL60/ADR was evaluated by MTS assay. The results showed that IC50 values were significantly decreased in HL60/ADR-B4GALT1 shRNA cells group compared with the control, suggesting that cell proliferation was inhibited by therapeutic drug when HL/60 cells were treated with B4GALT1 shRNA. Similar results were obtained with HL60/ADR-B4GALT5 shRNA cells group, chemosensitivity was remarkably restored when B4GALT5 gene was suppressed (Figures 2e and f).
To investigate the effect of knockdown of B4GALT1 or B4GALT5 gene on chemosensitivity of leukemian cells, we used nude mice bearing HL60/ADR, HL60/ADR-B4GALT1 shRNA and HL60/ADR-B4GALT5 shRNA xenografts to analyze the differences of tumor volumes when therapeutic drugs were administrated. In HL60/ADR-control shRNA group, there was no significant difference in tumor volumes between the mice groups with and without drug treatment, but in HL60//ADR-B4GALT1 shRNA group, tumor volumes were found to decrease significantly with drug treatment in comparison with that of the mice group without drug administration (Figure 2g). The same tendency was also seen in HL60//ADR-B4GALT5 shRNA group (Figure 2h). After the measurements of the tumor volumes, the tumors were sectioned for immunohistochemical (IHC) staining analysis of B4GALT1 and B4GALT5 expression patterns, the expression of these two genes were reduced in the mice group with shRNA treatment compared with untreated group or control group (Figures 2i and j). These results demonstrated that B4GALT1 and B4GALT5 genes were associated with the drug-resistant phenotype of HL60/ADR.
Upregulation of B4GALT1 or B4GALT5 gene results in acquirement of drug resistance of HL60 cells in vitro and in vivo
After verifying the effect of B4GALT1 and B4GALT5 gene suppression on tumor cell chemosensitivity, we transfected HL60 cells with B4GALT1 or B4GALT5 expression vector to determine the effect of overexpression of these two genes on chemoresistance of HL60 cells. Notably, increased levels of mRNA and protein of B4GALT1 and B4GALT5 were detected in B4GALT1 and B4GALT5 transfectants (Figures 3a–d). MTS assay revealed that IC50 values of three drugs were significantly higher in HL60/B4GALT1 and HL60/B4GALT5 cells than those in HL60 cells, suggesting a positive correlation between the two gene expression and chemoresistance of leukemia cells (Figures 3e and f).
Overexpression of B4GALT1 or B4GALT5 mediates the acquirement of MDR in HL60 cells. After full-length sequences transfection, both B4GALT1, T5 mRNAs (a and b) and proteins (c and d) were increased notably in HL60 cells by real-time PCR and western blot. (e and f) MTS assay showed that elevated levels of B4GALT1, T5 made HL60 cells resistant to adriamycin, paclitaxel and vincristine in vitro. (g and h) The tumor volume was not distinctly reduced with adriamycin injection in nude mice bearing HL60/B4GALT1 or HL60/B4GALT5 tumor. (i and j) IHC staining showed an enhanced expression of B4GALT1 or T5 in tumor samples generated from HL60 cells with shRNA treatment. For a–f, i and j, asterisk indicates significant increase from the groups without an asterisk (P<0.05), for g and h, *P<0.05
Nude mice were inoculated with tumor cells HL60, HL60/mock, HL60/B4GALT1 and HL60/B4GALT5. Tumor volumes were measured and compared between the groups with or without adriamycin treatment. In the group of mice bearing HL60 tumors, tumor volumes with adriamycin treatment were lower than those without. In the group of mice bearing HL60/B4GALT1 or B4GALT5 tumors, tumor volumes increased obviously even after adriamycin treatment (Figures 3g and h). High expression of B4GALT1 and B4GALT5 in tumors cells of HL60/B4GALT1 and HL60/B4GALT5 were illustrated by IHC staining, as shown in Figures 3i and j. Therefore, upregulation of B4GALT1 or B4GALT5 gene in HL60 cells led to raised resistance to chemotherapy.
Downregulation of B4GALT1 or B4GALT5 inhibits the activity of Hh signaling pathway and expression levels of P-gp and MRP1
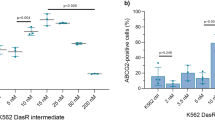
Here, we assessed the activity of the Hh signaling by treatment of HL60/ADR cells with B4GALT1 or B4GALT5 shRNA. The key molecules of Hh signaling, transcripts and proteins, were significantly reduced with shRNA transfection, revealed by real-time PCR (Figures 4a and b), western blotting (Figures 4c and d) and IHC staining (Figures 4e and f and Supplementary Figure 1). P-gp and MRP1 are the recognized molecules involved in the development of MDR, we therefore examined whether gene manipulation of B4GALT1 or B4GALT5 could influence the expression of P-gp and MRP1. Lower expression levels of P-gp and MRP1 were detected in HL60/ADR-B4GALT1 shRNA cells and HL60/ADR-B4GALT5 shRNA cells compared with those in control cells by flow cytometric analysis (Figures 4g and h).
Knockdown of B4GALT1 or B4GALT5 leads to Hh signaling suppression and P-gp, MRP1 downregulation. Expressions of Shh, Smo and GLI-1, the main molecules of Hh pathway, were repressed at mRNA levels with B4GALT1, T5 shRNA transfection in HL60/ADR cells (a and b). The reduced protein levels of sonic Hh signaling molecules were determined by western blot (c and d) and IHC staining (e and f). Decreased expressions of P-gp and MRP1 were examined by flow cytometry analysis in B4GALT1, T5-shRNA-treated HL60/ADR cells (g and h). Asterisk indicates significant difference from the groups without an asterisk (P<0.05)
Elevation of B4GALT1 or B4GALT5 gene expression activates Hh pathway and promotes expression levels of P-gp and MRP1
By contrast, overexpression of B4GALT1 or B4GALT5 in HL60 cells enhanced mRNAs and proteins expression of Smo, Shh and GLI-1, as illustrated in Figures 5a–f and Supplementary Figure 2. Moreover, HL60 cells expressed higher levels of P-gp and MRP1 with B4GALT1 or B4GALT5 overexpression (Figures 5g and h). Thus, the results may reveal an additional drug resistance mechanism of B4GALT1 or B4GALT5 in MDR of leukemia cells.
Upregulation of B4GALT1 or B4GALT5 activates Hh pathway and elevates the expressions of P-gp, MRP1. Shh, Smo and GLI-1 transcripts and proteins were proved to be enhanced in full-length B4GALT1 or B4GALT5-treated HL60 cells by real-time PCR (a and b), western blot (c and d) and IHC staining analysis (e and f), respectively. Flow cytometry analysis revealed a higher coexpression of P-gp and MRP1 in HL60 cells with B4GALT1 or B4GALT5 transfection (g and h). Asterisk suggests significant difference from the groups without an asterisk (P<0.05)
Chemosensitivity of HL60/ADR cells is restored in response to inhibiting Hh signaling activity
The effect of Hh signaling activity on chemoresistance of HL60/ADR cells was investigated by pharmacological inhibition of the Hh pathway. In Figures 6a, HL60/ADR cells with cyclopamine treatment showed significantly decreased mRNA and protein levels of the main signal molecules of Hh pathway. By methyl thiazolyl tetrazolium assay in vitro, we observed the inhibition of Hh pathway caused HL60/ADR cells sensitive to chemotherapy (Figure 6c), similar results were also obtained by in vivo chemosensitivity analysis, reduced tumor volumes were observed in mice group bearing HL60/ADR tumors with impaired Hh signaling (Figure 6d).
Inhibition of Hh pathway by cyclopamine restrains coexpression of P-gp and MRP1, and promotes HL60/ADR cells sensitive to chemotherapy. Using real-time PCR (a), western blot (b), and IHC staining analysis (e) downregulated Shh, Smo and GLI-1 transcripts and proteins were detected in cyclopamine-treated HL60/ADR cells. Cyclopamine treatment also alleviated chemoresistance of HL60/ADR cells, revealed by in vitro (c) and in vivo (d) susceptibility test. Simultaneously, flow cytometry analysis showed that suppression of Hh signaling resulted in reduced levels of P-gp and MRP1 (f). For a–c, e and f, asterisk indicates significant increase from the groups without an asterisk (P<0.05), for d, *P<0.05 versus HL60/ADR-tomatidine cells and HL60/ADR-cyclopamine cells without adriamycin treatment
Furthermore, flow cytometric analysis was performed to explore whether suppression of Hh signaling activity could influence the proteins expression of P-gp and MRP1. Low levels of P-gp and MRP1 were present in HL60/ADR cells with cyclopamine treatment (Figure 6f). These data implicated a role of Hh signaling in regulating P-gp and MRP1 expression and modulating the chemoresistance of HL60/ADR cells.
Increased expression levels of B4GALT1 and B4GALT5 are detected in most AML and CML cases with chemoresistance
To determine the expressions of MDR-related marker and B4GALT1–B4GALT7 of the BMMC samples from acute myeloid leukemia (AML) and chronic myeloid leukemia (CML) patients, flow cytometry assay and real-time PCR were carried out by using FITC-monoclonal antibodies against P-gp, MRP1 and B4GALT1–B4GALT7. Elevated mean fluorescence intensity of P-gp and MRP1 was observed in 37 of 71 CML patients and 29 of 75 AML patients. Then patients were divided into four groups: CML without MDR, CML/MDR, AML without MDR and AML/MDR. Each gene expression of B4GALT family of patient with MDR was compared with that of patient without MDR to obtain expression ratio. The value of each gene expression ≥2 was recognized to be significant. Data from 66 MDR patients were summarized in Table 1. Higher levels of B4GALT1 and B4GALT5 were found in chemoresistant leukemia samples, but expression levels of the other members of B4GALT family showed no difference between drug-resistant group and chemosensitive group. According to these results, the involvement of B4GALT1 and B4GALT5 overexpressions in drug resistance of leukemia cells was further confirmed.
Discussion
As a global issue of increasing concern, MDR leads to inadequate treatment and poor prognosis of leukemia patients. For decades, some progress has been gained on the mechanisms of MDR. Interestingly, our previous work has implied B4GALT1, a kind of glycogene, acts as a MDR mediator of human leukemia K562 cell line. Here, we carried on the studies in order to investigate the association between the B4GALT family and MDR of human leukemia cells.
Among seven members of B4GALT family, B4GALT1 is the first gene to be cloned and characterized, and is identified as a potential biomarker in malignancies.26, 27 B4GALT2 and B4GALT3 gene products catalyze the synthesis of N-linked oligosaccharides in many glycoproteins and specific glycolipids. Overexpression of B4GALT2 is proved to induce apoptosis in Hela cells.28 Unlike β1, 4-Gal-T1, T2 and T3, β1, 4-Gal-T4 has exclusive specificity for the acceptor sugars, and does not catalyze the transfer of galactose to asialo-agactotransferrin, asialo-agalacto-fetuin or ovalbumin. It has been reported that highly expression of B4GALT4 is linked to colorectal cancer metastasis and poor prognosis.29 β1, 4-Gal-T5 participates in the formation of both N-linked oligosaccharides and the various glycolipids. This enzyme could lead to high galactosylation on cell surfaces, and has been proved to be involved in the malignant phenotype of astrocytoma and glioma, indicating a possible role in tumorigenesis.30, 31 β1, 4-Gal-T6 catalyzes the biosynthesis of glycosphingolipids in UDP-dependent manner using magnesium or zinc. So far, there are few reports of the correlation of B4GALT6 to the different diseases. β1, 4-Gal-T7 regulates the synthesis of glycosaminoglycans and has roles in several pathophysiological events,32 for example, a missense mutation in the B4GALT7 gene is related to the Ehlers–Danlos syndrome progeroid type.33
In current study, B4GALT1, T2, T3 and T5 transcripts and proteins expressed constitutively in the four pairs of human leukemia cell lines and in the tumor cells of leukemia patients. B4GALT6 was not detectable in three pairs of cell lines except K562 and K562/ADR cells, while nonexistence of B4GALT4 and B4GALT7 was only found in U937 and U937/ADR cell line. All MDR cells and sample cells from patients with MDR were characterized by elevated levels of B4GALT1 and B4GALT5 compared with those of cells without MDR. These two genes are well known for their key roles in the process of proliferation, invasion and apoptosis of cancer cells. Our data also showed evidence that abnormal expression of B4GALT1 and B4GALT5 has an impact on the development of multidrug resistance, another malignant behavior of tumor cells. Although B4GALT4 has been recognized involving in cancer metastatic processes, we do not find a significant difference of B4GALT4 expression between the cell groups with or without MDR. After all, occurrence and development of tumors is a complex multistep process different from MDR.
Glycosylation, occurring to most of the human proteins after transcription, has important roles in the structural and functional changing of protein. Glycan chains are essential in maintaining the normal physiological function of cells and glycosylation alterations that have been studied intensively in the tumor biology field so as to better understand how diseases develop. It is well demonstrated that malignant cells and normal cells differ significantly in the characteristic changes of glycans and glycoconjugates.34, 35, 36, 37 Biosynthesis of glycans depends on GTs, the largest and most diverse enzyme groups. As upstream regulators of glycoproteins, GTs often exhibited abnormal activity in tumors, also in the development of drug-resistance process.38 In this study, the effects of B4GALT1 and B4GALT5 on MDR in HL60/ADR cell line were confirmed by in vitro and in vivo drug susceptibility analysis. We established two transfectants with stable inhibition of B4GALT1 or B4GALT5 gene using RNAi approach. Increased sensitivity of HL60/ADR cells to anti-leukemia drugs was found with both B4GALT1 and B4GALT5 shRNA treatment. Conversely, in HL60 cells with the overexpression of the two genes, acquirement of MDR was observed. On the basis of this result, we propose that B4GALT1 and B4GALT5 might function as critical genes involving in MDR.
The Hh signaling is one of the most examined signal pathways and participates in embryonic development, cell proliferation, carcinogenesis, apoptosis and acquirement of drug resistance.39, 40, 41, 42 Previously, we have revealed that B4GALT1 functioned as a modulator of Hh pathway in K562/ADR cell line. Here, B4GALT5 also exhibited the similar effect on the activity of Hh pathway in HL60/ADR cells, and blockage of Hh pathway by cyclopamine alleviated chemoresistance of HL60/ADR cells. These findings suggest both B4GALT1 and B4GALT5 could promote the development of MDR probably through regulating the Hh signaling pathway, where the main molecules are all glycoproteins. Further analysis would be necessary to estimate the glycosylation changes in drug-resistant leukemia cells compared with drug-sensitive cells.
It has been reported that the Hh signaling enhances drug efflux by ABC transporters in order to maintain MDR of tumor cells.43 ABC transporters are a superfamily of transmembrane proteins that transport a wide variety of substrates across cell membranes. They are found on the surface of normal cells and various cancer cells where they have crucial roles in the development of MDR. P-gp and MRP1, two main members of ABC transporters, are frequently used as markers to screen MDR patients clinically. We found that the levels of P-gp and MRP1, had a positive relationship with the expression of B4GALT1, B4GALT5 and the activity of Hh signaling in HL60 and HL60/ADR cell lines. As B4GALT1 and B4GALT5 were observed as regulatory genes on the activity of Hh signaling, we assumed that B4GALT1 and B4GALT5 might elevate the expression of P-gp and MRP1 through Hh pathway, thereby promoting MDR of leukemia cells.
In conclusion, our data demonstrated that overexpression of both B4GALT1 and B4GALT5 could activate the Hh signaling and increase the levels of P-gp and MRP1, thus reduce the efficacy of chemotherapy for leukemia cells. Seeking for agents that simultaneously inhibit β1, 4-Gal-T1 and β1, 4-Gal-T5 might be a promising strategy for overcoming MDR of leukemia patients.
Materials and Methods
Cell lines and culture conditions
Four human cell lines, including a chronic myelogenous leukemia cell line (K562), an acute myelogenous leukemia cell line (HL60), an acute promyelocytic leukemia cell line (NB4) and a leukemic monocytic lymphoma cell line (U937) were purchased from the China Center for Type Culture Collection (CCTCC, Wuhan, China). All cell lines were cultured in RPMI 1640 medium (Gibco, Grand Island, NY, USA) supplemented with 10% heat-inactivated fetal bovine serum (Gibco) and 1% penicillin–streptomycin (Gibco) at 37 °C in 5% CO2. We established four ADR sublines namely K562/ADR, HL60/ADR, NB4/ADR and U937/ADR from corresponding parental cell lines by stepwise exposures of cells to increasing concentrations of adriamycin from 1 μg/ml up to 5 μg/ml for 2 months. All ADR sublines could grow in the presence of chemotherapeutic agents, including adriamycin, paclitaxel and vincristine. One week before subsequent treatments, ADR cells were maintained in complete medium without adriamycin and cells with >90% viability were used for further studies.
Samples of patients
Seventy-one cases of CML patients and 75 cases of AML patients were included in this study after obtaining informed consent. The diagnosis of CML and AML was based on morphology, immunology, molecular and cytogenetic classification. All patients were treated in the First Affiliated Hospital of Dalian Medical University between March 2009 and May 2011. Bone marrow samples were collected at diagnosis and before treatment. Bone marrow mononuclear cells (BMMCs) were isolated by Ficoll-Hypaque density gradient centrifugation (Sigma-Aldrich, INC. St. Louis, MO, USA) and were cultured in plastic dishes to remove adherent cells at 37 °C for 24 h. Freshly separated non-adherent cells were maintained in modified Dulbecco’s medium containing 10% fetal bovine serum, 10 mM β-mercaptoethanol, 2 mM L-glutamine, 50 ng/ml human stem cell factor, 10 ng/ml human interleukin-3 and 10 ng/ml human interleukin-6. The expressions of P-gp and MRP1 were measured by flow cytometric assays to determine the resistant phenotype of patients. B4GALT1-7 levels of all patients were determined by real-time PCR.
Real-time PCR analysis
Real-time PCR was used to analyze gene expression. Total RNA was isolated using the RNeasy Mini Kit (Qiagen, Valencia, CA, USA), and cDNA was synthesized using QuantiTect Reverse Transcription Kit (Qiagen), according to the manufacturer’s protocol. Real-time PCR was carried out on an ABI Prism 7500 fast real-time PCR system (Applied Biosystems, Foster City, CA, USA) using QuantiTect SYBR Green PCR Kit (Qiagen). The primer pairs for PCR are listed in Table 2. Ratios of each gene and GAPDH gene expression levels were determined by subtracting the threshold cycle number (Ct) of the target gene from the Ct of GAPDH. The relative expression level of each gene was normalized to that of respective GAPDH.
Western blot analysis
Cells (1 × 106) were collected and lysed by adding 1 ml of 2 × concentrated electrophoresis sample buffer (125 mM Tris-HCl, pH 6.8, 5% glycerol, 2% SDS, 1% β-mercaptoethanol) to each Eppendorf tube. Protein concentrations were determined by a Micro BCA Protein Assay kit (Pierce, Rockford, IL, USA) according to the manufacturer’s protocol. Fifty micrograms of total protein were resolved by SDS-PAGE (10%) gel and then blotted onto a polyvinylidene difluoride membrane. After being blocked for 2 h with phosphate-buffered saline containing 0.1% Tween-20 and 5% powdered skim milk, the blots were incubated, respectively, overnight at 4 °C with rabbit anti human B4GALT1(Abcam, Cambridge, UK; 1 : 250 dilution), B4GALT2 (Abcam; 1 : 100 dilution), B4GALT3, 4, 5, 7 (Abcam; 1 : 500 dilution), B4GALT6 (Abcam; 1 : 200 dilution), Shh (Abcam; 1 : 2000 dilution), Smo (Abcam; 1 : 100 dilution) and GLI-1 antibodies (Abcam; 1 : 40 dilution), and then incubated with secondary antibody anti-rabbit-HRP (GE Healthcare UK Ltd, Little Chalf-ont, UK; 1 : 10 000 diluted). GAPDH antibody (Santa Cruz Biotech, Santa Cruz, CA, USA; 1 : 1000 dilution) was used as internal marker for control. All bands intensities were evaluated using ECL Western blotting kit (Amersham Biosciences, Buckinghamshire, UK) and were normalized to those of GAPDH.
Deregulation of B4GALT1 or B4GALT5 in HL60/ADR cells by RNAi
Transfection was performed in a 12-well plate at ∼ 50% confluent cultures. HL60/ADR cells were maintained in 1 ml of complete medium with 5 μg/ml Polybrene (sc-134220, Santa Cruz Biotech) per well and were treated with 0.4 μM B4GALT1 or T5-specific shRNA lentiviral particles (sc-40616-V and sc-72405-V, Santa Cruz Biotech) overnight, three control wells were transduced with control shRNA lentiviral particles (sc-108080, Santa Cruz Biotech). Then medium in each well was replaced with 1 ml of complete medium (without Polybrene) and cells were diluted to 1 : 3 for selecting stable clones expressing the shRNA by 5 μg/ml puromycin dihydrochloride (sc-108071, Santa Cruz Biotech). The transfection efficiency was about 80% and cell viability was 90% by trypan blue dye exclusion assay. Four weeks later, several resistant colonies were picked and expanded for further study.
Overexpression of B4GALT1 or B4GALT5 in HL60 cells
The human B4GALT1, B4GALT5 and Shh coding sequences were obtained from TaKaRa company (Dalian, China) and were inserted into the pEGFP-N2 vector (Invitrogen, Carlsbad, CA, USA), respectively, using EcoRI, XhoI sites. Cells were transfected with 5 μg of target gene expression vector or empty vector (EV) in 100-mm dishes using PolyFect Transfection Reagent (Qiagen) according to the manufacturer’s instruction. After 60 days of screening, the cell lines stably expressing B4GALT1 (HL60/B4GALT1), B4GALT5 (HL60/B4GALT5) and empty vector (HL60/mock) were established. Then cells were collected for gene expression assay and for further explorations.
In vitro drug cytotoxic assay
The CellTiter 96 AQueous One Solution Cell Proliferation Assay (MTS) kit (Promega, Madison, WI, USA) was used to determine the chemosensitivity of cell groups with genetic manipulation and pharmacological inhibition of the Hh pathway. Cells (1 × 104) were seeded in 96-well plate and incubated with paclitaxel, vincristine and adriamycin (Sigma, St. Louis, MO, USA) ,respectively, for 48 h. Then cells were stained with 10 μl MTS for 3 h at 37 °C. The absorbance was measured at 490 nm by microplate reader (Model 680; Bio-Rad, Hercules, CA, USA). The drug resistance was estimated by comparing the IC50 values (drug concentration that inhibits cell growth by 50%) from growth inhibition curves.
In vivo chemosensitivity assay
A total of 84 male nude mice (5 weeks old) were acquired from the Animal Facility of Dalian Medical University and equally divided into seven groups-HL60, HL60/ADR, HL60/ADR-control shRNA, HL60/ADR-B4GALT1 shRNA, HL60/ADR-B4GALT5 shRNA, HL60/ADR-tomatidine and HL60/ADR-cyclopamine. Tumor cells (5 × 106) were injected into the right flank of the nude mouse subcutaneously. Seven days later, tumors appeared at the sites of injection, and then half of each group was randomly assigned to receive 7 mg/kg adriamycin i.p. three times a week for 3 weeks, the rest tumor-bearing mice of each group received normal saline injection as control. Twenty-eight days after tumor implantation, IHC staining was conducted and external caliper was used to determine the volume of xenografted tumors, and the tumor volume was calculated by the following formula:
Tumor volume=1/2(length × width2)
IHC staining analysis
Visible tumors were removed from the mice and immunohistochemistry was performed on paraffin-embedded sections. The slides were dried, deparaffinized, rehydrated and then were immersed in 3% hydrogen peroxide for 10 min to quench the endogenous peroxidase. After consecutive washing with PBS, the slides were labeled overnight at 4 °C with anti-Shh, Smo, GLI-1, B4GALT1 and T5 antibodies (Abcam) at a dilution of 1 : 200 or isotype immunoglobulins (Santa Cruz Biotechnology) as negative control. The following staining was performed at room temperature for 60 min with secondary streptavidin-HRP-conjugated antibody (Santa Cruz Biotech). Finally, the sections were counterstained with hematoxylin and cover-slipped. The Image-Pro Plus 4.5 Software (Media Cybernetics, Bethesda, MD, USA) was used to analyze the expression of proteins.
Inhibition of the Hh signaling
Cyclopamine was used to suppress the activity of the Hh signaling in HL60/ADR cells. Briefly, cells (1 × 104 cells per well) were maintained in 100 μl medium containing 0.5% FBS for 48 h in the presence or absence of 6 μM cyclopamine. Tomatidine, inactive but with similar structure to cyclopamine, was served as control. Changes in chemosensitivity and gene expression were measured by MTS assay and real-time PCR analysis, respectively. Each experiment was run in triplicate to determine means and S.D.s.
Flow cytometry analysis
Tumor cells were washed with1 × PBS buffer containing 20% bovine serum, and then were preincubated with 5% powdered skim milk for 30 min to block nonspecific binding. For surface staining of P-gp and MRP1, aliquots of cells were incubated with fluorescein isothiocyanate-anti human P-gp, MRP1 (Abcam) or an isotype control antibody (Santa Cruz Biotech for 40 min at 4 °C at the recommended dilutions. After repeated centrifugation at 1000 r.p.m., labeled cells were resuspended in 0.2 ml PBS and were analyzed with FACSCalibur (BD Biosciences, San Jose, CA, USA). Fluorescence intensity was measured by Cell Quest software (BD Biosciences).
Statistical analysis
Statistical analysis was performed using SPSS17.0 statistical software (IBM Inc., Beijing, China). A one-way analysis of variance and Student’s t-test was used to examine the possible differences in multiple comparisons. P<0.05 was considered to be statistically significant. Each experiment was repeated at least three times.
Abbreviations
- B4GALT:
-
β-1,4-galactosyltransferase gene
- BMMC:
-
bone marrow mononuclear cells
- MDR:
-
multidrug resistance
- Hh:
-
hedgehog
- P-gp:
-
p-glycoprotein
- MRP1:
-
multidrug resistance-associated protein 1
- GTs:
-
glycosyltransferases
- β1, 4-Gal-T:
-
β-1, 4-galactosyltransferase
- ABCB1:
-
ATP-binding cassette subfamily B member 1
- ADR:
-
adriamycin-resistant
- GAGs:
-
glycosaminoglycans
- EDSP:
-
Ehlers–Danlos syndrome progeroid type
- Shh:
-
sonic hedgehog
- Smo:
-
smoothened
- GLI:
-
glioma-associated oncogene
- MTT:
-
methyl thiazolyl tetrazolium
References
Coutinho PM, Deleury E, Davies GJ, Henrissat B . An evolving hierarchical family classification for glycosyltransferases. J Mol Biol 2003; 328: 307–317.
Kang X, Wang N, Pei C, Sun L, Sun R, Chen J et al. Glycan-related gene expression signatures in human metastatic hepatocellular carcinoma cells. Exp Ther Med 2012; 3: 415–422.
Li M, Song L, Qin X . Glycan changes: cancer metastasis and anti-cancer vaccines. J Biosci 2010; 35: 665–673.
Kudo T, Nakagawa H, Takahashi M, Hamaguchi J, Kamiyama N, Yokoo H et al. N-glycan alterations are associated with drug resistance in human hepatocellular carcinoma. Mol Cancer 2007; 6: 32–40.
Nakano M, Saldanha R, Göbel A, Kavallaris M, Packer NH . Identification of glycan structure alterations on cell membrane proteins in desoxyepothilone B resistant leukemia cells. Mol Cell Proteomics 2011; 10: M111.009001.
Zhang Z, Zhao Y, Jiang L, Miao X, Zhou H, Jia L . Glycomic alterations are associated with multidrug resistance in human leukemia. Int J Biochem Cell Biol 2012; 44: 1244–1253.
Amado M, Almeida R, Schwientek T, Clausen H . Identification and characterization of large galactosyltransferase gene families: galactosyltransferases for all functions. Biochim Biophys Acta 1999; 1473: 35–53.
Han Y, Zhou X, Ji Y, Shen A, Sun X, Hu Y et al. Expression of beta-1,4-galactosyltransferase-I affects cellular adhesion in human peripheral blood CD4+ T cells. Cell Immunol 2010; 262: 11–17.
Nixon B, Lu Q, Wassler MJ, Foote CI, Ensslin MA, Shur BD . Galactosyltransferase function during mammalian fertilization. Cells Tissues Organs 2001; 168: 46–57.
Nakamura N, Yamakawa N, Sato T, Tojo H, Tachi C, Furukawa K . Differential gene expression of beta-1,4-galactosyltransferases I, II and V during mouse brain development. J Neurochem 2001; 76: 29–38.
Nakamura Y, Haines N, Chen J, Okajima T, Furukawa K, Urano T et al. Identification of a Drosophila gene encoding xylosylprotein beta4-galactosyltransferase that is essential for the synthesis of glycosaminoglycans and for morphogenesis. J Biol Chem 2002; 277: 46280–46288.
Zhu X, Jiang J, Shen H, Wang H, Zong H, Li Z et al. Elevated beta1,4-galactosyltransferase I in highly metastatic human lung cancer cells. Identification of E1AF as important transcription activator. J Biol Chem 2005; 280: 12503–12516.
Choi HJ, Chung TW, Kim CH, Jeong HS, Joo M, Youn B et al. Estrogen induced β-1,4-galactosyltransferase 1 expression regulates proliferation of human breast cancer MCF-7 cells. Biochem Biophys Res Commun 2012; 426: 620–625.
Park JE, Lee KY, Do SI, Lee SS . Expression and characterization of beta-1,4-galactosyltransferase from Neisseria meningitidis and Neisseria gonorrhoeae. J Biochem Mol Biol 2002; 35: 330–336.
Yan M, Cheng C, Ding F, Jiang J, Gao L, Xia C et al. The expression patterns of beta1,4 galactosyltransferase I and V mRNAs, and Galbeta1-4GlcNAc group in rat gastrocnemius muscles post sciatic nerve injury. Glycoconj J 2008; 25: 685–701.
Villegas-Comonfort S, Serna-Marquez N, Galindo-Hernandez O, Navarro-Tito N, Salazar EP . Arachidonic acid induces an increase of β-1,4-galactosyltransferase I expression in MDA-MB-231 breast cancer cells. J Cell Biochem 2012; 113: 3330–3341.
Wassler MJ, Shur BD, Zhou W, Geng YJ . Characterization of a novel ubiquitin-conjugating enzyme that regulates beta1,4-galactosyltransferase-1 in embryonic stem cells. Stem Cells 2008; 26: 2006–2018.
Wei Y, Liu D, Ge Y, Zhou F, Xu J, Chen H et al. Down-regulation of beta1,4GalT V at protein level contributes to arsenic trioxide-induced glioma cell apoptosis. Cancer Lett 2008; 267: 96–105.
Pasca di Magliano M, Hebrok M . Hedgehog signalling in cancer formation and maintenance. Nat Rev Cancer 2003; 3: 903–911.
Zhu W, You Z, Li T, Yu C, Tao G, Hu M et al. Correlation of hedgehog signal activation with chemoradiotherapy sensitivity and survival in esophageal squamous cell carcinomas. Jpn J Clin Oncol 2011; 41: 386–393.
Cui D, Xu Q, Wang K, Che X . Gli1 is a potential target for alleviating multidrug resistance of gliomas. J Neurol Sci 2010; 288: 156–166.
Kobune M, Takimoto R, Murase K, Iyama S, Sato T, Kikuchi S et al. Drug resistance is dramatically restored by hedgehog inhibitors in CD34+ leukemia cells. Cancer Sci 2009; 100: 948–955.
Fenner KS, Troutman MD, Kempshall S, Cook JA, Ware JA, Smith DA et al. Drug-drug Interactions mediated through p-glycoprotein: clinical relevance and in vitro-in vivo correlation using digoxin as a probe drug. Clin Pharmacol Ther 2009; 85: 173–181.
Deeley RG, Westlake C, Cole SP . Transmembrane transport of endo- and xenobiotics by mammalian ATP-binding cassette multidrug resistance proteins. Physiol Rev 2006; 86: 849–899.
Zhou H, Zhang Z, Liu C, Jin C, Zhang J, Miao X et al. B4GALT1 gene knockdown inhibits the hedgehog pathway and reverses multidrug resistance in the human leukemia K562/adriamycin-resistant cell line. IUBMB Life 2012; 64: 889–900.
Poeta ML, Massi E, Parrella P, Pellegrini P, De Robertis M, Copetti M et al. Aberrant promoter methylation of beta-1,4 galactosyltransferase 1 as potential cancer-specific biomarker of colorectal tumors. Genes Chromosomes Cancer 2012; 51: 1133–1143.
Brown JR, Yang F, Sinha A, Ramakrishnan B, Tor Y, Qasba PK et al. Deoxygenated disaccharide analogs as specific inhibitors of beta1-4-galactosyltransferase 1 and selectin-mediated tumor metastasis. J Biol Chem 2009; 284: 4952–4959.
Zhou J, Wei Y, Liu D, Ge X, Zhou F, Jiang XY et al. Identification of beta1,4GalT II as a target gene of p53-mediated HeLa cell apoptosis. J Biochem 2008; 143: 547–554.
Chen WS, Chang HY, Li CP, Liu JM, Huang TS . Tumor beta-1,4-galactosyltransferase IV overexpression is closely associated with colorectal cancer metastasis and poor prognosis. Clin Cancer Res 2005; 11: 8615–8622.
Xu S, Zhang S, Chen C, Yan J, Cai M, Zhu X et al. Over-expression of beta-1,4-galactosyltransferase V increases the growth of astrocytoma cell line. J Exp Clin Cancer Res 2002; 21: 409–414.
Wei Y, Zhou F, Ge Y, Chen H, Cui C, Li Q et al. Beta1,4-galactosyltransferase V regulates self-renewal of glioma-initiating cell. Biochem Biophys Res Commun 2010; 396: 602–607.
Talhaoui I, Bui C, Oriol R, Mulliert G, Gulberti S, Netter P et al. Identification of key functional residues in the active site of human {beta}1,4-galactosyltransferase 7: a major enzyme in the glycosaminoglycan synthesis pathway. J Biol Chem 2010; 285: 37342–37358.
Faiyaz-Ul-Haque M, Zaidi SH, Al-Ali M, Al-Mureikhi MS, Kennedy S, Al-Thani G et al. A novel missense mutation in the galactosyltransferase-I (B4GALT7) gene in a family exhibiting facioskeletal anomalies and Ehlers-Danlos syndrome resembling the progeroid type. Am J Med Genet A 2004; 128A: 39–45.
Alley WR Jr, Vasseur JA, Goetz JA, Svoboda M, Mann BF, Matei DE et al. N-linked glycan structures and their expressions change in the blood sera of ovarian cancer patients. J Proteome Res 2012; 11: 2282–2300.
Park SY, Lee SH, Kawasaki N, Itoh S, Kang K, Hee Ryu S et al. α1-3/4 fucosylation at Asn 241 of β-haptoglobin is a novel marker for colon cancer: a combinatorial approach for development of glycan biomarkers. Int J Cancer 2012; 130: 2366–2376.
de Leoz ML, Young LJ, An HJ, Kronewitter SR, Kim J, Miyamoto S et al. High-mannose glycans are elevated during breast cancer progression. Mol Cell Proteomics 2011; 10: M110.002717.
Satomaa T, Heiskanen A, Leonardsson I, Angström J, Olonen A, Blomqvist M et al. Analysis of the human cancer glycome identifies a novel group of tumor-associated N-acetylglucosamine glycan antigens. Cancer Res 2009; 69: 5811–5819.
Baran Y, Bielawski J, Gunduz U, Ogretmen B . Targeting glucosylceramide synthase sensitizes imatinib-resistant chronic myeloid leukemia cells via endogenous ceramide accumulation. J Cancer Res Clin Oncol 2011; 137: 1535–1544.
Agathocleous M, Locker M, Harris WA, Perron M . A general role of hedgehog in the regulation of proliferation. Cell Cycle 2007; 6: 156–159.
Jeong J, Mao J, Tenzen T, Kottmann AH, McMahon AP . Hedgehog signaling in the neural crest cells regulates the patterning and growth of facial primordia. Genes Dev 2004; 18: 937–951.
Ma X, Chen K, Huang S, Zhang X, Adegboyega PA, Evers BM et al. Frequent activation of the hedgehog pathway in advanced gastric adenocarcinomas. Carcinogenesis 2005; 26: 1698–1705.
Steg AD, Katre AA, Bevis KS, Ziebarth A, Dobbin ZC, Shah MM et al. Smoothened antagonists reverse taxane resistance in ovarian cancer. Mol Cancer Ther 2012; 11: 1587–1597.
Sims-Mourtada J, Izzo JG, Ajani J, Chao KS . Sonic Hedgehog promotes multiple drug resistance by regulation of drug transport. Oncogene 2007; 26: 5674–5679.
Acknowledgements
This work was supported by grants from the National Key Basic Research and Development Program (973 program) of China (no. 2012CB822100), and from the National Natural Science Foundation of China (81071415, 81271910).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by A Stephanou
Supplementary Information accompanies this paper on Cell Death and Disease website
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Zhou, H., Ma, H., Wei, W. et al. B4GALT family mediates the multidrug resistance of human leukemia cells by regulating the hedgehog pathway and the expression of p-glycoprotein and multidrug resistance-associated protein 1. Cell Death Dis 4, e654 (2013). https://doi.org/10.1038/cddis.2013.186
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2013.186
Keywords
This article is cited by
-
B4GALT1 expression predicts prognosis and adjuvant chemotherapy benefits in muscle-invasive bladder cancer patients
BMC Cancer (2018)
-
Association between one-carbon metabolism indices and DNA methylation status in maternal and cord blood
Scientific Reports (2018)
-
Chromosome 9p copy number gains involving PD-L1 are associated with a specific proliferation and immune-modulating gene expression program active across major cancer types
BMC Medical Genomics (2017)
-
MiR-124-3p/B4GALT1 axis plays an important role in SOCS3-regulated growth and chemo-sensitivity of CML
Journal of Hematology & Oncology (2016)
-
Modification of sialylation is associated with multidrug resistance in human acute myeloid leukemia
Oncogene (2015)