Abstract
Multiple sclerosis (MS) is a chronic and debilitating autoimmune disease, characterized by chronic inflammatory demyelination in the nervous tissue and subsequent neurological dysfunction. Spermidine, a natural polyamine, has been shown to affect inflammation in some experimental models. We show here that spermidine could alleviate experimental autoimmune encephalomyelitis (EAE), a model for MS, through regulating the infiltration of CD4+ T cells and macrophages in central nervous system. Unexpectedly, we found that spermidine treatment of MOG-specific T cells did not affect their pathogenic potency upon adaptive transfer; however, spermidine diminished the ability of macrophages in activating MOG-specific T cells ex vivo. Depletion of macrophages in diseased mice completely abolished the therapeutic effect of spermidine, indicating a critical role of spermidine-activated macrophages. Mechanistically, spermidine was found to specifically suppress the expression of interleukin-1beta (IL-1β), IL-12 and CD80 while enhance the expression of arginase 1 in macrophages. Interestingly, macrophages from spermidine-treated mice could also reverse EAE progression, while pretreatment of those macrophages with the arginase 1 inhibitor abrogated the therapeutic effect. Therefore, our studies revealed a critical role of macrophages in spermidine-mediated treatment on EAE and provided novel information for better management of MS.
Similar content being viewed by others
Main
Multiple sclerosis (MS) is a T cell-mediated autoimmune disease, pathologically characterized by multifocal inflammatory demyelination and degeneration in the white matter of the central nervous system (CNS).1 MS most commonly occurs in young adults, especially those with a specific genetic background and exposed to particular non-genetic triggers, such as virus, metabolism or environmental factors, that together lead to a self-sustaining autoimmune disorder and subsequent recurrent immune attacks on the CNS.2 Current therapy of MS mainly relies on non-specific suppression of the immune system and often results in drug resistance and severe side effects.3 Therefore, specific mechanism-based, more effective treatment strategies for MS still await to be developed.
Experimental autoimmune encephalomyelitis (EAE) is a widely used animal model of MS.4 In EAE mice, pathologic T cells are primed and expanded upon exposure to myelin antigens that are normally sequestered in CNS. As professional antigen-presenting cells (APCs), macrophages have the capacity to prime naive T cells and initiate autoreactive immune response in spinal cord.5 Activated T cells migrate to nervous tissues and are restimulated by resident myelin antigens presented by microglia/macrophages.6 During this process, macrophages are also major sources of inflammatory mediators, such as interleukin-1 (IL-1),7 tumor necrosis factor-alpha (TNF-α)8 and nitric oxide,9 that are critical for EAE development.10 In addition, phagocytic cells in nervous tissues engulf myelin debris in MS lesions, supporting for the involvement of macrophages in the demyelination process.11 Importantly, elimination of macrophages could reduce the severity of clinical signs of EAE,12 stressing a key role of infiltrated macrophages as effector cells. Actually, macrophages can adopt different immune phenotypes in response to various local inflammatory environments. Classically activated macrophages (CAMs) generally exhibit pro-inflammatory activities, whereas alternatively activated macrophages (AAMs) with high expression of arginase 1 could inhibit immune responses.13, 14 Therefore, macrophages are involved in multiple stages of the pathogenesis of EAE, and could be potential treatment targets.
Natural polyamines, including putrescine, spermidine and spermine, are essential for cell survival, proliferation, differentiation and aging.15 The cellular concentration of polyamine is under tight regulation, a process achieved by the combination of synthesis, catabolism and transport. The synthesis of polyamines is started from arginine, which is converted to ornithine by arginase. Ornithine is then decarboxylated to produce putrescine, which can then be further converted to spermidine and spermine. Disruption of spermidine metabolism has been reported to be associated with the pathogenesis of various diseases.15, 16, 17 Spermidine has been reported to inhibit the production of pro-inflammatory cytokines by LPS-challenged microglia.18 Through attenuating systematic inflammatory factors, spermine has been shown to enhance the survival rate of mice suffering from septic shock.19 However, it remains elusive whether spermidine has effects on autoimmune diseases.
In this study, we investigated the effect of spermidine on EAE, and found that spermidine administration suppresses EAE progression by inhibiting the pro-inflammatory activity of macrophages, rather than directly regulating pathogenic T cells. When we transferred the spermidine pretreated myelin oligodendrocyte glycoprotein (MOG)-reactive T cells into normal mice, the classical EAE was still established. However, when macrophages were depleted, the therapeutic effect of spermidine was abolished. Moreover, we found that spermidine upregulates arginase 1 expression level in macrophages, which confers these cells with significant therapeutic effect on EAE. Our data revealed a central role of macrophages in spermidine-mediated immunoregulation in EAE.
Results
Spermidine alleviates EAE symptoms in mice
Polyamines, such as spermidine, have been found to be involved in autoimmune diseases and other inflammatory responses.20, 21 To determine whether exogenously administered spermidine could also affect the course of autoimmune diseases, we examined its in vivo effects on mouse EAE. We established the mouse EAE model and treated with spermidine right after the appearance of clinical symptoms and found that spermidine had a significant therapeutic effect (Figure 1a). We also examined the preventive effect of spermidine on EAE by administering this compound immediately following MOG immunization and found that the onset of EAE was also dramatically delayed and the disease severity, as indicated by the clinical scores, was reduced (Figure 1b). Histological analysis of the affected spinal cord showed that spermidine administration markedly attenuated typical demyelination and inflammation in EAE mice (Figure 1c).
Spermidine ameliorates EAE. (a and b) Clinical scores of EAE mice administrated daily with spermidine (50 mg/kg body weight) or PBS from day 8 (n=10) (a) or from day 1 (n=7 or n=5) (b) post immunization. Means±S.E.M. are shown (*P<0.05, two-way ANOVA). (c) Histological analysis of spinal cord from spermidine- or vehicle-treated EAE mice on day 18 post immunization. The paraffin-embedded sections were analyzed for demyelination by luxol fast-blue staining, and analyzed for leukocyte infiltration by hematoxylin and eosin (H&E) staining. Scale bars, 200 μM. Outlines indicate demyelination in Fast-blue staining and indicate leukocyte infiltration area in H&E staining. (d) Infiltration of CD4+ T cells and macrophages was analyzed by immunofluorescence staining of CD4 and CD11b respectively on the spinal cord from spermidine- or vehicle-treated EAE mice. Scale bars, 100 μM. Outlines indicate the infiltration area of CD4+ T cells and macrophages
Spermidine reduces leukocyte infiltration and immune response in CNS
To examine the effect of spermidine treatment on immune cell infiltration into CNS, we detected various cell types using immunofluorescence and found that spermidine treatment greatly reduced the infiltration of CD4+ T cells and CD11b+ macrophages (Figure 1d). To verify this observation, we isolated and enumerated mononuclear cells (MNCs) from the whole spinal cord and found a marked reduction in the number of CNS-infiltrating MNCs in spermidine-treated mice (Figure 2a). To determine the effect of spermidine on different subsets of MNCs, we performed flow-cytometric analysis and found that the all subsets examined (CD4+, CD8+ and CD11b+) were reduced (Figure 2b).
Spermidine suppresses the autoimmune response in EAE mice. (a) The total numbers of MNCs in whole spinal cord were isolated from EAE mice treated with spermidine or vehicle on day 18 post immunization (n=4). (b) The absolute numbers of various types of immune cells per spinal cord (n=4). (c) The distribution of CD4+ T cells, CD8+ T cells, B cells (stained for B220) and macrophages (stained for CD11b) in spleen of spermidine- or vehicle-treated EAE mice. (d) The absolute numbers of cells as gated in (c) per spleen (n=7–9). (e) [3H]-thymidine incorporation assay showing the proliferation of splenocytes from spermidine- or vehicle-treated EAE mice under the stimulation of MOG peptide (20 μg/ml) or ConA (2 μg/ml) for 72 h (n=6). (f) Cytokine production by the splenocytes from spermidine- or vehicle-treated EAE mice. The splenocytes were reactivated with MOG peptide (20 μg/ml) for 48 h before multiplex immunoassay (n=7–9 per group). Data are present as means±S.E.M., representing of two independent experiments. *P<0.05; **P<0.01
To investigate the general effect of spermidine on immune responses, we also determined the percentage and number of CD4+, CD8+, CD11b+ and B220+ cells in the spleen and found that although it is not as dramatic as in CNS, spermidine-treated EAE mice show statistically significant reduction in CD4+ and CD11b+ cells, whereas the percentage for CD8+ T cells and B220+ B cells was not altered (Figures 2c and d). We reasoned that the differential effects of spermidine on immune cells in the spleen and spinal cord could be due to the fact that the MOG35–55 peptide only activated a small portion of CD4+ T cells in the spleen, while in the spinal cord the infiltrated CD4+ T cells are mostly MOG reactive.22 To verify this notion, we isolated splenocytes from MOG-immunized mice with and without spermidine treatment and activated with MOG or ConA. We found that MOG-induced reaction of T cells in vitro is significantly reduced by spermidine, while direct activation of T cells by ConA was not affected (Figure 2e). In parallel, the production of pro-inflammatory cytokines (interferon-gamma (IFN-γ), IL-12, IL-17, IL-2 and IL-6, typical cytokines accompanying EAE) was dramatically reduced in spermidine-treated group (Figure 2f). These results demonstrate that spermidine does not have a general effect on T cells, rather affects T-cell activation induced by antigens presented by APCs.
The therapeutic effect of spermidine on EAE relies on macrophages
Since T cells and macrophages have been reported to be involved in EAE and we showed that spermidine has the effects on both cell populations, it is still possible that spermidine exerts its effect either directly through affecting the function of myelin-specific T cells or indirectly through regulating the function of macrophages. To test this premise, we first pretreated MOG-reactive T cells with or without spermidine and then adoptively transferred into normal recipient mice. Unexpectedly, spermidine pretreatment did not alleviate EAE, suggesting that the therapeutic effect of spermidine was not exerted directly through regulating T cells (Figure 3a). To further determine the effect of spermidine on T cells, we treated MOG-immunized mice with and without spermidine, then isolated T cells and transferred into recipient mice. Again, spermidine did not affect the pathogenic role of the T cells (Figure 3b). Thus based on these results, we conclude that spermidine has no direct effect on T cells, implicating a critical role of macrophages in mediating the anti-inflammatory effect of spermidine on EAE. Therefore, we intravenously injected liposomes containing clodronate to deplete macrophages in spleen and spinal cord (Supplementary Figure S1a). We found that macrophage depletion alleviated the development of EAE, consistent with a previous report.23 Furthermore, spermidine showed no further therapeutic effect when both spermidine and clodronate liposomes were administrated, indicating that the effect of spermidine requires macrophages (Figure 3c). In addition, when splenocytes were challenged with MOG ex vivo, the proliferation of T cells displayed a similar trend (Figure 3d).
The therapeutic effect of spermidine on EAE is dependent on macrophages. (a) Clinical scores of mice with passive EAE induced by adoptive transfer of CD4+ T cells (3 × 106 per mouse) that were pretreated with spermidine (10 μM) or vehicle in vitro. (b) Clinical scores of mice with passive EAE induced by adoptive transfer of CD4+ T cells (3 × 106 per mouse) isolated from spermidine- or vehicle-treated EAE mice. (c) Clinical sores of EAE mice that were treated with spermidine or vehicle combined with empty or clodronate liposome. One microgram of empty or clodronate liposome was given to EAE mice intravenously on day 7, day 9, day 11 and day 13; spermidine or vehicle was administrated daily from day 11 post immunization. (d) Splenocytes were derived from spermidine-treated or control EAE mice, which were injected with clodronate liposome or empty liposome. Then, the proliferation of MOG-T cell was assessed by [3H]-thymidine incorporation. (e) [3H]-thymidine incorporation assay showing the proliferation of CD4+ T cells from EAE mice co-cultured with macrophages from spermidine- or vehicle-treated EAE mice in the presence of MOG peptide (20 μg/ml) (left panel), and CD4+ T cells from spermidine- or vehicle-treated EAE mice co-cultured with macrophages derived from EAE mice in the presence of MOG peptide (20 μg/ml) (right panel) (n=6 wells in each group). (f) Cytokine production in the supernatant of the aforementioned cultures was analyzed by multiplex immunoassay (n=3 wells in each group). (g) The levels of anti-inflammatory cytokines including IL-10 and TGF-β in the supernatant of CD4+ T cells co-culture with macrophages. Data are representative of three independent experiments. *P<0.05; **P<0.01. N.S., not significant
We next investigated how macrophages exert their effect on EAE in spermidine-treated mice. We co-cultured CD4+ T cells with macrophages derived from EAE mice treated with or without spermidine. We found that MOG35–55 peptide-induced T-cell proliferation was significantly reduced when presented by macrophages from spermidine-treated mice (Figure 3e). In addition, proinflammatory cytokines including IL-1β, TNF-α and IL-12 were also decreased (Figure 3f), whereas the levels of anti-inflammatory cytokines such as IL-10 and TGF-β were not affected (Figure 3g). Consistently, we found that the levels of pro-inflammatory cytokines including IL-1β, TNF-α and IL-12, as well as chemokines such as CCL2, CCL3 and CXCL1 were also decreased in serum upon spermidine treatment (Supplementary Figure S2a and b). These results indicate that spermidine may exert its effect by indirectly altering the encephalitogenic activity of CD4+ T cells through regulating the function of macrophages.
Spermidine alters macrophage phenotypes
It has been revealed that macrophages can be activated by different signals and resulted in different functional phenotypes. CAMs are often associated with pro-inflammatory response and AAMs frequently accompany anti-inflammatory reactions.13 The expression patterns of co-stimulatory molecules and various cytokines are important determinators of macrophage phenotypes.24 We therefore assessed whether the expression of co-stimulatory molecules and cytokines in macrophages was affected by spermidine treatment. As shown in Figure 4a, the expression of CD80 and CD86 was markedly reduced on the macrophages from both spleen and spinal cord of spermidine-treated EAE mice. We next examined whether the inflammatory cytokine production is affected by spermidine treatment. Macrophages purified from the spleen of spermidine-treated mice were stimulated with LPS for 24 h. Interestingly, we found that the levels of IL-1β, IL-12, IL-6 and TNF-α secreted by these macrophages were significantly downregulated, whereas IL-10 and TGF-β were unchanged (Figure 4b). Collectively, our data demonstrate that spermidine inhibits the expression of co-stimulatory molecules as well as production of pro-inflammatory cytokines by macrophages, leading to reduced T-cell activation and proliferation.
Spermidine suppresses the inflammatory responses of macrophages. (a) MNCs isolated from spleen of spermidine-treated (black lines) or vehicle-treated (gray lines) EAE mice at day 18 post immunization were stimulated with MOG35–55 peptide for 48 h and analyzed for CD80 and CD86 expression in the population of CD11b+ macrophages by flow cytometry. Numbers indicate the median fluorescence intensity of sample of spermidine treated (black) and vehicle treated (gray), respectively. Representative histogram of three independent experiments is shown. (b) Production of cytokines by splenic macrophages from spermidine- or vehicle-treated EAE mice. Splenic macrophages were treated with LPS (50 ng/ml) for 24 h and the supernatant was analyzed with multiplex immunoassay (n=4). (c) Immunoblot analysis of phosphorylated IKKα/β, IκBα and p65, as well as total IKKα/β, IκBα, p65 and GAPDH in lysates of CD4+ T cells and macrophages from spleen of spermidine- or vehicle-treated EAE mice. (d) Immunoblot analysis of phosphorylated IKKα/β, IκBα and p65, as well as total IKKα/β, IκBα, p65 and GAPDH in lysates of splenic macrophages from EAE mice. Splenocytes from EAE mice were stimulated with the MOG peptide in the presence of spermidine (20 μM) or vehicle for 2 h. The macrophages were then purified and analyzed by immunoblotting. (e) Immunoblot analysis of phosphorylated IκBα and p65, as well as total IκBα, p65 and GAPDH in lysates of bone marrow-derived macrophages pretreated with or without spermidine for 1 h before LPS stimulation for the indicated times. Immunoblotting results in (c–e) represent three independent experiments. (f) The BMDMs were stimulated with LPS (50 ng/ml) in the presence of different concentrations of spermidine or vehicle for 16 h and then harvested for total RNA extraction. The mRNA levels of Il1b, Il12a and Tnfa were detected by quantitative RT-PCR. Error bars represent means±S.E.M. of three independent experiments. Protein levels were quantified using Image J software. *P<0.05; **P<0.01
Spermidine inhibits NF-κB signaling in macrophages
To delineate the molecular mechanism underlying the observed inhibitory effects of spermidine on macrophages, we assessed the changes in NF-κB signaling, which is believed to have critical roles in the regulation of the expression of pro-inflammatory factors and co-stimulatory molecules in macrophages.25, 26, 27 As expected, macrophages derived from spermidine-treated EAE mice exhibited markedly reduced activation of NF-κB accompanied by decreased phosphorylation of IKKα/β and IκB. The phosphorylation of p65 at Ser536, which is required for optimal transactivation potential of NF-κB, was also reduced in macrophages from spermidine-treated EAE mice, whereas the activity of NF-κB signaling in CD4+ T cells was not affected (Figure 4c). Similar results were obtained with macrophages derived from EAE mice treated with spermidine in the presence of MOG peptide in vitro (Figure 4d).
To verify the direct effect of spermidine on macrophages, we isolated bone marrow-derived macrophages (BMDMs) from naive mice and then treated with spermidine in vitro. We found that spermidine also inhibited LPS-induced phosphorylation and degradation of IκBα as well as phosphorylation of p65 in BMDMs at both the initial (10 min) and the later (20–60 min) stages (Figure 4e). Additionally, the expression level of pro-inflammatory cytokines including Il1b, Il12 and Tnfa was significantly inhibited by spermidine in these BMDMs (Figure 4f). We also found that the expression level of Nos2 and the production of nitric oxide were decreased in BMDMs with spermidine treatment (Supplementary Figure S3a and b). Therefore, our findings suggest that spermidine exerts its effect directly on macrophages by blocking NF-κB signaling via regulating IκBα stability and p65 activity, subsequently reducing NF-κB targeted gene expression in macrophages. Thus, this critical signaling pathway involved in pro-inflammatory response was affected by spermidine treatment.
Macrophages of spermidine-treated mice could adoptively transfer the protective effect on EAE
The above results showed that spermidine inhibited pro-inflammatory activity of macrophages. Given the plasticity of macrophage-mediated immunoregulation, we questioned whether the immunophenotype of macrophages could be affected by spermidine. To investigate whether spermidine-treated macrophages possess the anti-inflammatory function, we isolated splenic macrophages from spermidine-treated EAE mice and vehicle control mice on day 15 post immunization, and then transferred into recipient EAE mice on the day of disease onset. Surprisingly, we found that macrophages from spermidine-treated mice dramatically ameliorated the disease severity while those received macrophages from vehicle control mice showed no changes (Figure 5a). To verify whether the donor macrophages regulate the T-cell function, we challenged splenocytes derived from treated EAE mice with MOG peptide, and found that MOG-elicited proliferative response (Figure 5b) and the production of pro-inflammatory cytokines such as IL-1β, IL-12 and IL-17 (Figure 5c) were significantly reduced in recipient mice that received spermidine-treated macrophages. Moreover, we found that the infiltration of inflammatory cells including T cells and B cells was significantly decreased in EAE mice transferred with spermidine-treated macrophages (Figures 5d and e). Collectively, these data demonstrate that spermidine conferred macrophages immunosuppression activity in EAE mice.
Spermidine endows macrophages with the immunosuppression capacity. (a) Clinical scores of EAE mice received splenic macrophages at indicated time from spermidine- or vehicle-treated EAE mice (n=7 in each group) (**P<0.01, two-way ANOVA). (b) [3H]-thymidine incorporation assay showing the proliferation of MOG peptide-stimulated splenocytes of indicated treated EAE mice (n=4). (c) Production of inflammatory cytokines by MOG peptide-stimulated splenocytes of EAE mice in the treatment of splenic macrophages from spermidine- or vehicle-treated EAE mice (n=4). The absolute numbers of MNCs in whole spinal cords (d) and various types of immune cells per spinal cord (e) in recipient EAE mice transferred with macrophages (n=5). Data are present as means±S.E.M. and representing of at least two independent experiments. *P<0.05; **P<0.01
Spermidine induces inhibitory macrophages and arginase 1-mediated immunosuppression in macrophages
To elucidate the mechanism underlying the observed therapeutic effect of macrophages on EAE, we purified macrophages from the spleen of spermidine-treated or control EAE mice, and performed RNA sequencing analysis to pinpoint the immunosuppression effectors. We identified 45 differentially expressed genes between macrophages from spermidine-treated EAE mice and those from vehicle-treated EAE mice (Figures 6a and b). Among the downregulated genes, NF-κB target genes including Ptgis, Vcam1, Fcgrt, Ppplr14a and Cd7 were identified (Figure 6a), corroborating the observation that spermidine inhibits NF-κB signaling. Additionally, by qPCR analysis, we found that macrophages from spermidine-treated EAE mice expressed significantly lower levels of NF-κB target pro-inflammatory cytokines including Il6, Il1b, Il12 as well as Nos2 (Supplementary Figure S4a), as compared with those from control mice, whereas the levels of Il10 and Tgfb had no changes (Supplementary Figure S4b). Interestingly, we found that the most upregulated gene is Arg1, a M2 polarization marker, and we further validated the upregulated Arg1 by qPCR and flow-cytometrical analysis (Figures 6c and d). Immunoblotting analysis showed that the protein level of arginase 1 was also significantly increased in macrophages from mice treated with spermidine (Figure 6e). Consistently, a substantial increase in arginase-1 activity was observed in spermidine-treated BMDMs (Figure 6f). Besides, we found that other M2 makers such as Retnla and Ym1 are also upregulated in the macrophages from spermidine-treated EAE mice (Supplementary Figure S4c). Arginase 1 in macrophages has been reported to modulate the innate as well as adaptive immune responses.28, 29 We thus hypothesized that arginase 1 may mediate the inhibition of EAE by macrophages from spermidine-treated mice. To examine this hypothesis, Nw-hydroxy-nor-l-arginine (nor-NOHA) was employed to block arginase-1 activity. Macrophages derived from bone marrow were pretreated with spermidine for 24 h in the presence or absence of nor-NOHA at 100 μM, a concentration exhibited no cytotoxicity to macrophages (Supplementary Figure S5a), and then co-cultured with anti-CD3/28 activated CD4+ T cells. [3H]-thymidine incorporation analysis showed that the inhibitory effect of spermidine-treated macrophages on CD4+ T-cell proliferation was completely abolished by addition of nor-NOHA (Figure 6g). Moreover, the upregulation of Arg1 mRNA induced by spermidine was markedly reversed (Supplementary Figure S5b). Consistently, pretreatment with nor-NOHA abrogated the therapeutic effect of macrophages from spermidine-treated mice on EAE (Figure 6h). Taken together, these data demonstrated that spermidine induces the expression of arginase 1, which has a critical role in macrophage-mediated inhibition of T-cell proliferation and the therapeutic effect on EAE.
Immunosuppression capacity of macrophage is associated with M2 polarization and mediated by arginase 1. (a) Heatmap representing differentially expressed genes by RNA sequencing analysis on macrophages from spermidine- or vehicle-treated mice, with fold-change cutoff of 0.5 and 2, and q-value cutoff of 0.1 (P-value below 0.0009). Gene symbols in green indicate NF-κB target genes. (b) Volcano plot of gene expression comparing P-value versus fold change of the RNA sequencing data on macrophages from spermidine- or vehicle-treated mice. The cutoffs were set as described in (a). The expression of Arg1 in splenic macrophages from spermidine- or vehicle-treated EAE mice was analyzed by qPCR (c) and flow cytometry (d) (n=5–6 mice in each group). (e) Immunoblot analysis of arginase 1 and GAPDH in lysates of splenic macrophages from EAE mice. Splenocytes of EAE mice were stimulated with MOG peptides in the presence of indicated concentrations of spermidine for 24 h. The macrophages were then purified and analyzed by immunoblotting. (f) The arginase-1 activity in BMDMs treated with various dosages of spermidine was determined. (g) [3H]-thymidine incorporation assay showing the proliferation of anti-CD3/CD28 stimulated CD4+ T cells co-cultured with bone marrow macrophages. The macrophages had been pretreated with spermidine or vehicle in the presence or absence of nor-NOHA for 24 h. (h) Clinical scores of EAE mice treated with transfer of splenic macrophages from spermidine- or vehicle-treated EAE mice. The splenic macrophages were pretreated with or without nor-NOHA (100 μM) before transfer. Means±s.e.m. are shown (n=7 mice in each group). *P<0.05, **P<0.01 (two-way ANOVA (h) and two-tailed unpaired t-test (c, d, f, g))
Discussion
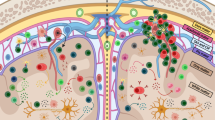
Polyamines, primarily spermidine and spermine, have been found to be involved in the regulation of inflammatory responses. The concentration of polyamines specifically increases at inflammatory sites during infection, trauma, cancer and autoimmune diseases.16, 17 Released by injured or dying cells, polyamines have been considered as important regulators to limit inflammatory damages.21 In this study, we investigated the anti-inflammatory property of spermidine in the context of an autoimmune disease. We found that spermidine administration ameliorated mouse EAE by modulating the function of macrophages. Specifically, spermidine reduces the antigen-presenting capacity and pro-inflammatory cytokine production of macrophages by targeting NF-κB signaling and endows them with an M2-like anti-inflammatory phenotype. One important characteristic of these macrophages is their high expression of arginase-1. We further demonstrated that this enzyme has a critical role in mediating the therapeutic effect of spermidine (summarized in Figure 7).
Schematic depiction of spermidine alleviating EAE through shifting the activity of macrophages. Spermidine is uptaken by macrophages and modulate their function, rather than directly targeting pathogenic myelin-specific T cells. Specifically, spermidine inhibited the expression of pro-inflammatory cytokines and co-stimulatory molecules in macrophages through downregulating the activity of NF-κB pathway. More importantly, spermidine upregulates expression of arginase 1 in macrophages, which consume the microenvironmental l-arginine required for T cells. A synergetic effect of the above elements suppresses the activation and proliferation of myelin-specific T cells and inhibits the progression of EAE
Although the pathogenesis of MS and EAE has been demonstrated to be CD4+ T-cell dependent, innate immune cells, especially macrophages, have also been shown to have important roles in the progression of MS and EAE. Adoptive transfer of T cells from EAE mice treated with spermidine did not affect the course of EAE development, indicating that spermidine has no direct effect on T cells. Critically, we observed that depletion of macrophages with liposome completely abolished the treatment effects of spermidine on EAE, verifying the central role of macrophages in spermidine-mediated immunoregulation in EAE.
The function of activated macrophages during EAE progression is complicated. In CNS, CAMs (M1 cells) release pro-inflammatory cytokines, which contribute to the damage of myelin sheath and axon,30 whereas AAMs (M2 cells) produce anti-inflammatory factors and mediate inflammation resolution and tissue repair.31 The effect of spermidine on macrophages could be due to its inhibitory effect on the NF-κB signaling pathway, which is critical for the production of pro-inflammatory cytokines and progression of EAE. Indeed, it has been shown that the mice with deficiency in p50, one of the NF-κB subunits, became resistant to EAE.32 In our analysis, we found that the phosphorylation and degradation of IκBα and phosphorylation of p65 were downregulated in macrophages, but not in CD4+ T cells. Therefore, blocking NF-κB signaling by spermidine may lead macrophages to M2 polarization during EAE. Indeed, spermidine significantly increased the expression of M2 marker genes such as Arg1, Retnla and Ym1 in macrophages.
Arginase 1 is well known for its physiological role in converting l-arginine to ornithine and urea. Consumption of arginine is believed to impair effective immune responses. In this regard, myeloid cells, such as macrophages, utilize local l-Arg starvation to control the proliferation of T lymphocytes.33 Indeed, Arg1 activity in myeloid cells has been shown to inhibit immune responses and attenuate chronic disease.34, 35 Interestingly, it has also been reported that arginase 1 from macrophages directly suppresses the proliferation of T lymphocytes through impairing the expression of the CD3ξ chain, the major conductor of TCR signaling.28, 36 Given the immunoregulatory function of arginase 1, we next focused on arginase 1 in macrophages induced by spermidine. Surprisingly, we found that pretreatment with arginase 1 inhibitor remarkably abrogated macrophages-mediated inhibition of T-cell proliferation and therapeutic efficacy against EAE, suggesting that the enzyme activity of arginase 1 underlies the anti-inflammatory function of M2-like macrophages induced by spermidine. During the progression of EAE, polyamine metabolism undergoes dynamic changes. We found that the level of polyamines including putrecine, spermine and spermidine in splenocytes was dramatically increased at the remission stage of EAE (day 20 post immunization). Interestingly, upon the treatment with exogenous spermidine, the increase in level of those polyamines shifted to the peak stage of EAE and then declined during the remission stage (Supplementary Figure S6a). Moreover, the level of arginine was significantly decreased in macrophages from spermidine-treated mice (Supplementary Figure S6b). Since high levels of spermidine and spermine can be converted to putrescine,37 these dynamic changes could be attributed to the upregulated arginase 1 induced by exogenous spermidine in macrophages.
The transport system of spermidine is well characterized in bacterium Escherichia coli and in yeast Saccharomyces cerevisiae.38, 39 However, in mammals, no polyamine receptor has been defined. Actually, it has been believed that spermidine uptake is mediated by endocytosis in mammals.39 As the main component of mononuclear-phagocyte system, macrophages are one of the most competent cells with endocytosis capacity.24 Thus, macrophages, rather than T lymphocytes, could be the major target cells for administrated spermidine. Spermidine is an ionic compound, and versatile in regulating cellular processes. In addition to its anti-inflammatory function, spermidine has also been reported to promote optic nerve regeneration in EAE through exerting its anti-oxidant effect.40 Although oxidative stress occurred in the optic nerve, inflammation has critical roles in the initiation and progression of EAE. Therefore, it is possible that spermidine may attenuate the severity of EAE mainly by exerting its anti-inflammatory function partially through the anti-oxidant activity. Spermidine has also been implicated to exert its effect through electrostatic interaction with many anionic macromolecules, such as DNA, RNA and proteins,38, 41 these polyamines can modulate the activity of ion channels, such as K+ channels and Ca2+ channels;42 spermidine can also directly control the activity of some kinases.43 We found that spermidine downregulates the NF-kB pathway and promotes the expression of arginase 1 in macrophages, which could be due to one or more of the aforementioned functions of spermidine. However, the specific mechanism underling this process still needs to be further investigated.
In summary, our study provides compelling evidence supporting the immunoregulatory role of spermidine in the treatment of autoimmune disease. The therapeutic effect of spermidine on EAE is dependent on macrophages rather than directly regulating T cells. This work suggests that spermidine could be a promising drug candidate for MS intervention.
Materials and Methods
Reagents and mice
Spermidine was obtained from Sigma-Aldrich (St Louis, MO, USA). Antibodies used in the immunoblot analysis, including those specific for phosphorylated IκBα, IκBα, phosphorylated NF-κB, NF-κB, arginase 1 and GAPDH, were from Cell Signaling Technology (Danvers, MA, USA). Fluorochrome-conjugated antibodies specific for CD4, CD8, B220, CD11b, CD115, F4/80, CD80, CD86 and PD-L1 were from eBioscience (San Diego, CA, USA). C57BL/6J mice were purchased from the Shanghai Laboratory Animal Center of Chinese Academy of Sciences (Shanghai, China). The mice were maintained under specific pathogen-free conditions. All experiments were performed on male mice between 8 and 10 weeks old. The health of the mice was monitored periodically by veterinary professionals throughout the experiments, and all animal studies were approved by the Institutional Animal Care and Use Committee of the Institute of Health Sciences, Shanghai Institutes for Biological Sciences of Chinese Academy of Sciences.
Induction and treatment of EAE
Mice were immunized subcutaneously with 300 μg MOG35–55 peptide (MEVGWYRSPFSRVVHLYRNGK) (GL Biochem, Shanghai, China) emulsified in CFA containing 5 mg/ml heat-killed H37Ra strain of Mycobacterium tuberculosis (Difco Laboratories, Detroit, MI, USA). Pertussis toxin (200 ng, List Biological Laboratories, Campbell, CA, USA) in PBS was administered i.v. on days 0 and 2 post immunization. Mice were examined and scored daily for disease severity using the standard scale according to Stromnes et al.:44 0, no clinical signs; 1, limp tail; 2, hind-limb weakness; 3, hind-limb paralysis; 4, hind-limb and forelimb paralysis; 5, moribund/dead state. To examine the therapeutic effect of spermidine on EAE, spermidine or vehicle (PBS) was intraperitoneally administered at a dose of 50 mg/kg daily from day 11 post immunization. To examine the prevention effect of spermidine on EAE, spermidine or vehicle (PBS) was intraperitoneally administered daily from day 1 post immunization. The passive EAE was induced by adoptive transfer of pathogenic CD4+ T cells from EAE mice. Briefly, the splenocytes were isolated from active EAE mice on day 10 post immunization and stimulated with 20 μg/ml of MOG 35–55 in the presence of 10 μM spermidine or vehicle for 3 days. The CD4+ T cells were then purified and transferred i.v. into irradiated (400 cGy) recipient mice (3 × 106 per mice). Pertussis toxin (200 ng) was intraperitoneally administrated to mice on day 0 and day 2 after transfer. To selectively deplete macrophages, EAE mice were injected with clodronate liposome (Encapsula NanoSciences, Brentwood, TN, USA) according to the guidance of manufacturer. Briefly, 1 mg clodronate liposome was intravenously injected to EAE mice on day 7, day 9, day 11 and day 13 post immunization. The administration of spermidine was then performed from day 11 after immunization. All experiments on pathological analysis were performed between day 15 and day 18 post immunization.
Immunohistology
Spermidine- or vehicle-treated EAE mice were fixed in 4% paraformaldehyde immediately after perfusion and spinal cords were isolated. Paraffin-embedded sections of spinal cords were stained with luxol fast blue and H&E to evaluate demyelination and inflammation. For immunofluorescence, fresh spinal cords were embedded in OCT (Tissue Tek, CA, USA) and frozen. The frozen sections were stained with primary antibodies specific for CD11b (BD Biosciences, San Jose, CA, USA) and CD4 (BD Biosciences), and stained with second antibodies (Life Technologies, Carlsbad, CA, USA). Nuclei were counterstained with Hoechst 33342 (Life Technologies). Images were acquired using the axio imager a2 microscope along with ZEN pro 2011 software (Zeiss, Ottawa, ON, Canada).
MNC analysis
To analyze MNCs in spleen and spinal cord, mice were anesthetized and perfused to remove peripheral blood on day 15 post immunization. Spleen and spinal cord were then isolated and homogenized. Single-cell suspensions were obtained by filtering through 70 μm cell strainers. CNS MNCs were purified using a 37/70% (vol/vol) discontinuous Percoll gradient (GE Healthcare, Piscataway, NJ, USA), and viable cells were counted by 0.4% Trypan blue exclusion. Splenic CD4+ T cells and monocytes/macrophages were purified with CD4 and CD11b MicroBeads according to the manufacturer’s instructions (Miltenyi Biotec, Auburn, CA, USA). For surface marker analysis, MNCs were incubated with fluorescence-conjugated antibodies. Flow-cytometric analysis was performed on an FACS Calibur flow cytometer (Becton Dickinson, San Jose, CA, USA).
Proliferation and cytokine assays
To assess the response of splenocytes to MOG peptide, splenocytes (5 × 105 per well) from EAE mice were stimulated with the MOG35–55 peptide for up to 72 h. For ex vivo antigen-presenting assay, CD4+ T cells from spermidine- or vehicle-treated mice were incubated with irradiated (18 Gy) splenic macrophage from spermidine- or vehicle-treated EAE mice at a ratio of 1 : 2 in the presence of MOG peptide for 72 h. [3H] thymidine was added at the last 16 h of the above culture systems, and was measured by scintillation counting (Wallac Microbeta Perkin-Elmer, Waltham, MA, USA). The cytokines and chemokines in culture supernatants and serum were analyzed with multiplex immunoassay (Bio-Plex System, Bio-Rad, Hercules, CA, USA).
Preparation of bone marrow-derived macrophages
To obtain BMDMs, bone marrow was isolated from femurs and tibias of C57BL/6J mice, and cultured in DMEM/F12 with additive of 10% FBS and 20% L929 conditioned media for 7 days. The adherent cells were harvested and analyzed for purity with flow cytometry before carried out for further studies, and the F4/80+ CD11b+ macrophages were always above 95%.
Immunoblot analysis
Cells were lysed with RIPA lysis buffer (Millipore, Billerica, MA, USA) supplemented with protease inhibitor cocktails (Roche Applied Science, Mannheim, Germany). Proteins were separated by SDS-PAGE, and transferred onto nitrocellulose membrane. The membranes were blocked with 5% non-fat dried milk for 1 h and incubated with primary antibodies against p-Ikkα/β, p-IκBα, IκBα, p-NFκB, NFκB, arginase 1 and GAPDH overnight at 4 °C. After washing with Tris-buffered saline with Tween 20 (TBST) buffer, the membranes were incubated with HRP-conjugated secondary antibody (Cell Signaling) and then subjected to chemiluminescent detection according to the manufacturer’s instructions (Millipore).
Polyamine analysis
To analyze polyamine levels in splenocytes and macrophages, spleens were harvested and cells were isolated at various points during EAE procession. Single-cell suspension was lysed and centrifuged (10 min at 14 000g). The supernatant was collected for polyamine analysis, and aliquots containing 1 mg of protein were loaded onto LC/MS/MS instruments (AB SCIEX Triple Quad 5500, Framingham, MA, USA). To determine arginase-1 activity, BMDMs (1 × 106 cells/ml) were incubated in 12-well tissue culture plates in the presence or absence of spermidine for 24 h, and arginase-1 activity in cell lysate was determined using an arginase assay kit (BioAssay Systems, Hayward, CA, USA).
Gene expression analysis
Real-time quantitative PCR was performed with 7900 HT Fast Real-Time PCR system (Applied Biosystems, Foster City, CA, USA) using FastStart Universal SYBR Green Master (Roche). Oligonucleotide primers were as follows: Il1b, 5′-AAGTTGACGGACCCCAAAAGAT-3′, 5′-TGTTGATGTGCTGCTGCGA-3′; Il12a, 5′-CAATCACGCTACCTCCTCTTTT-3′, 5′-CAGCAGTGCAGGAATAATGTTTC-3′; Il12b, 5′-GTCCTCAGAAGCTAACCATCTCC-3′, 5′-CCAGAGCCTATGACTCCATGTC-3′; Tnfa, 5′-ATGGCCTCCCTCTCATCAGTTC-3′, 5′-GGCTACAGGCTTGTCACTCGAA-3′; Il6, 5′-AGATAAGCTGGAGTCACAGAAGGAG-3′, 5′-CGCACTAGGTTTGCCGAGTAG-3′; Arg1, 5′-CTCCAAGCCAAAGTCCTTAGAG-3′, 5′-AGGAGCTGTCATTAGGGACATC-3′; Retnla, 5′-GGATGCCAACTTTGAATAGGA-3′, 5′-GGATAGTTAGCTGGATTGGCA-3′; Ym1, 5′-CAGGTCTGGCAATTCTTCTGAA-3′, 5′-GTCTTGCTCATGTGTGTAAGTGA-3′; Actb, 5′-CCACGAGCGGTTCCGATG-3′, 5-GCCACAGGATTCCATACCCA-3′. Total amount of mRNA was normalized with Actb mRNA.
Statistical analysis
Data were presented as means±S.E.M., and the significance of difference was assessed by unpaired two-tailed t-test unless otherwise indicated. The P-values of clinical scores were determined by two-way multiple-range ANOVA for multiple comparisons. A P-value of <0.05 was considered as statistically significant.
Abbreviations
- MS:
-
multiple sclerosis
- EAE:
-
experimental autoimmune encephalomyelitis
- SPD:
-
spermidine
- CNS:
-
central nervous system
- TNF-α:
-
tumor necrosis factor-alpha
- IFN-γ:
-
interferon-gamma
- IL-1β:
-
interleukin-1beta
- IL-12:
-
interleukin-12
- IL-17:
-
interleukin-17
- APC:
-
antigen-presenting cell
- Arg1:
-
Arginase 1
References
Bar-Or A . Immunology of multiple sclerosis. Neurol Clin 2005; 23: 149–175.
Steinman L . Immunology of relapse and remission in multiple sclerosis. Annu Rev Immunol 2014; 32: 257–281.
Franklin RJM, Ffrench-Constant C . Remyelination in the CNS: from biology to therapy. Nat Rev Neurosci 2008; 9: 839–855.
Inoue M, Shinohara ML . The role of interferon-beta in the treatment of multiple sclerosis and experimental autoimmune encephalomyelitis - in the perspective of inflammasomes. Immunology 2013; 139: 11–18.
Malpass K . Disease mechanisms in MS: a role for sodium channels in regulation of macrophage-mediated pathology in multiple sclerosis lesions. Nat Rev Neurol 2012; 8: 592.
Bogie JF, Stinissen P, Hendriks JJ . Macrophage subsets and microglia in multiple sclerosis. Acta Neuropathol 2014; 128: 191–213.
Bauer J, Berkenbosch F, Van Dam AM, Dijkstra CD . Demonstration of interleukin-1 beta in Lewis rat brain during experimental allergic encephalomyelitis by immunocytochemistry at the light and ultrastructural level. J Neuroimmunol 1993; 48: 13–21.
Villarroya H, Marie Y, Ouallet JC, Le Saux F, Tchelingerian JL, Baumann N . Expression of TNF alpha in central neurons of Lewis rat spinal cord after EAE induction. J Neurosci Res 1997; 49: 592–599.
Okuda Y, Nakatsuji Y, Fujimura H, Esumi H, Ogura T, Yanagihara T et al. Expression of the inducible isoform of nitric oxide synthase in the central nervous system of mice correlates with the severity of actively induced experimental allergic encephalomyelitis. J Neuroimmunol 1995; 62: 103–112.
Anthony DC, Miller KM, Fearn S, Townsend MJ, Opdenakker G, Wells GM et al. Matrix metalloproteinase expression in an experimentally-induced DTH model of multiple sclerosis in the rat CNS. J Neuroimmunol 1998; 87: 62–72.
Raine CS . Analysis of autoimmune demyelination - its impact upon multiple-sclerosis. Lab Invest 1984; 50: 608–635.
Huitinga I, Vanrooijen N, Degroot CJA, Uitdehaag BMJ, Dijkstra CD . Suppression of experimental allergic encephalomyelitis in Lewis rats after elimination of macrophages. J Exp Med 1990; 172: 1025–1033.
Gordon S, Martinez FO . Alternative activation of macrophages: mechanism and functions. Immunity 2010; 32: 593–604.
Rodriguez PC, Quiceno DG, Zabaleta J, Ortiz B, Zea AH, Piazuelo MB et al. Arginase I production in the tumor microenvironment by mature myeloid cells inhibits T-cell receptor expression and antigen-specific T-cell responses. Cancer Res 2004; 64: 5839–5849.
Iarashi K, Kashiwagi K . Modulation of cellular function by polyamines. Int J Biochem Cell Biol 2010; 42: 39–51.
Merentie M, Uimari A, Pietila M, Sinervirta R, Keinanen TA, Vepsalainen J et al. Oxidative stress and inflammation in the pathogenesis of activated polyamine catabolism-induced acute pancreatitis. Amino Acids 2007; 33: 323–330.
Thomas TJ, Gunnia UB, Seibold JR, Thomas T . Defective signal-transduction pathways in T-cells from autoimmune Mrl-Lpr/Lpr mice are associated with increased polyamine concentrations. Biochem J 1995; 311: 175–182.
Choi YH, Park HY . Anti-inflammatory effects of spermidine in lipopolysaccharide-stimulated BV2 microglial cells. J Biomed Sci 2012; 19: 31.
Zhu S, Ashok M, Li JH, Li W, Yang H, Wang P et al. Spermine protects mice against lethal sepsis partly by attenuating surrogate inflammatory markers. Mol Med 2009; 15: 275–282.
Franca-Costa J, Van Weyenbergh J, Boaventura VS, Luz NF, Malta-Santos H, Oliveira MC et al. Arginase I, polyamine, and prostaglandin E2 pathways suppress the inflammatory response and contribute to diffuse cutaneous leishmaniasis. J Infect Dis 2015; 211: 426–435.
Weiss TS, Herfarth H, Obermeier F, Ouart J, Vogl D, Scholmerich J et al. Intracellular polyamine levels of intestinal epithelial cells in inflammatory bowel disease. Inflamm Bowel Dis 2004; 10: 529–535.
Jones MV, Nguyen TT, Deboy CA, Griffin JW, Whartenby KA, Kerr DA et al. Behavioral and pathological outcomes in MOG 35-55 experimental autoimmune encephalomyelitis. J Neuroimmunol 2008; 199: 83–93.
Huitinga I, van Rooijen N, de Groot CJ, Uitdehaag BM, Dijkstra CD . Suppression of experimental allergic encephalomyelitis in Lewis rats after elimination of macrophages. J Exp Med 1990; 172: 1025–1033.
Gordon S, Taylor PR . Monocyte and macrophage heterogeneity. Nat Rev Immunol 2005; 5: 953–964.
Hayden MS, Ghosh S . NF-kappaB in immunobiology. Cell Res 2011; 21: 223–244.
Zou GM, Hu WY . LIGHT regulates CD86 expression on dendritic cells through NF-kappaB, but not JNK/AP-1 signal transduction pathway. J Cell Physiol 2005; 205: 437–443.
Zhao JL, Freeman GJ, Gray GS, Nadler LM, Glimcher LH . A cell type-specific enhancer in the human B7.1 gene regulated by NF-kappa B. J Exp Med 1996; 183: 777–789.
Rodriguez PC, Zea AH, DeSalvo J, Culotta KS, Zabaleta J, Quiceno DG et al. L-arginine consumption by macrophages modulates the expression of CD3 zeta chain in T lymphocytes. J Immunol 2003; 171: 1232–1239.
Sahin E, Haubenwallner S, Kuttke M, Kollmann I, Halfmann A, Dohnal AM et al. Macrophage PTEN regulates expression and secretion of arginase I modulating innate and adaptive immune responses. J Immunol 2014; 193: 1717–1727.
Newman TA, Woolley ST, Hughes PM, Sibson NR, Anthony DC, Perry VH . T-cell- and macrophage-mediated axon damage in the absence of a CNS-specific immune response: involvement of metalloproteinases. Brain 2001; 124 (Pt 11): 2203–2214.
Rawji KS, Yong VW . The benefits and detriments of macrophages/microglia in models of multiple sclerosis. Clin Dev Immunol 2013; 2013: 948976.
Hilliard B, Samoilova EB, Liu TS, Rostami A, Chen Y . Experimental autoimmune encephalomyelitis in NF-kappa B-deficient mice:roles of NF-kappa B in the activation and differentiation of autoreactive T cells. J Immunol 1999; 163: 2937–2943.
Qiu F, Huang J, Sui M . Targeting arginine metabolism pathway to treat arginine-dependent cancers. Cancer Lett 2015; 364: 1–7.
Burrack KS, Tan JJ, McCarthy MK, Her Z, Berger JN, Ng LF et al. Myeloid cell Arg1 inhibits control of arthritogenic alphavirus infection by suppressing antiviral T cells. PLoS Pathog 2015; 11: e1005191.
Shearer JD, Richards JR, Mills CD, Caldwell MD . Differential regulation of macrophage arginine metabolism: a proposed role in wound healing. Am J Physiol 1997; 272 (2 Pt 1): E181–E190.
Rodriguez PC, Zea AH, Culotta KS, Zabaleta J, Ochoa JB, Ochoa AC . Regulation of T cell receptor CD3zeta chain expression by L-arginine. J Biol Chem 2002; 277: 21123–21129.
Gerner EW, Meyskens FL Jr . Polyamines and cancer: old molecules, new understanding. Nat Rev Cancer 2004; 4: 781–792.
Minois N, Carmona-Gutierrez D, Madeo F . Polyamines in aging and disease. Aging 2011; 3: 716–732.
Igarashi K, Kashiwagi K . Characteristics of cellular polyamine transport in prokaryotes and eukaryotes. Plant Physiol Biochem 2010; 48: 506–512.
Guo X, Harada C, Namekata K, Kimura A, Mitamura Y, Yoshida H et al. Spermidine alleviates severity of murine experimental autoimmune encephalomyelitis. Invest Ophthalmol Vis Sci 2011; 52: 2696–2703.
Panagiotidis CA, Artandi S, Calame K, Silverstein SJ . Polyamines alter sequence-specific DNA-protein interactions. Nucleic Acids Res 1995; 23: 1800–1809.
Williams K . Interactions of polyamines with ion channels. Biochem J 1997; 325 (Pt 2): 289–297.
Landau G, Bercovich Z, Park MH, Kahana C . The role of polyamines in supporting growth of mammalian cells is mediated through their requirement for translation initiation and elongation. J Biol Chem 2010; 285: 12474–12481.
Stromnes IM, Goverman JM . Active induction of experimental allergic encephalomyelitis. Nat Protoc 2006; 1: 1810–1819.
Acknowledgements
We thank Dr. Douglas Green for comments and suggestions. This study was supported by grants from the Programs of National Natural Science of China (81330046, 81273316, 81571612, 81530043, 31200680), the Scientific Innovation Project of the Chinese Academy of Science (XDA 01040100), the Ministry of Science and Technology of China (2015CB964400).
Author contributions
Research studies were designed by YS, YW, WC and QY; experiments were conducted by QY, CZ, JC, LL and YH; FL bred the mice; QY, CZ, WC, PS, TV, MJ and QC were responsible for acquiring data and analyzing data; QY, CZ, GC, WC and YS wrote the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by G Kroemer
Supplementary Information accompanies this paper on Cell Death and Differentiation website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Yang, Q., Zheng, C., Cao, J. et al. Spermidine alleviates experimental autoimmune encephalomyelitis through inducing inhibitory macrophages. Cell Death Differ 23, 1850–1861 (2016). https://doi.org/10.1038/cdd.2016.71
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cdd.2016.71
This article is cited by
-
Polyamine metabolite spermidine rejuvenates oocyte quality by enhancing mitophagy during female reproductive aging
Nature Aging (2023)
-
Spermidine protects cartilage from IL-1β-mediated ferroptosis
Molecular and Cellular Biochemistry (2023)
-
Spermidine protects against acute kidney injury by modulating macrophage NLRP3 inflammasome activation and mitochondrial respiration in an eIF5A hypusination-related pathway
Molecular Medicine (2022)
-
Spermidine reduces neuroinflammation and soluble amyloid beta in an Alzheimer’s disease mouse model
Journal of Neuroinflammation (2022)
-
Gut microbiome profiles and associated metabolic pathways in patients of adult-onset immunodeficiency with anti-interferon-gamma autoantibodies
Scientific Reports (2022)