Abstract
Oxidative stress and nitrosative stress are both suggested to be involved in cardiac ischemia-reperfusion (I/R) injury. Using time-lapse confocal microscopy of cardiomyocytes and high-affinity O2−• and Zn2+ probes, this study is the first to show that I/R, reactive oxygen species (ROS), and reactive nitrogen species (RNS) all cause a marked increase in the [O2−•]i, resulting in cytosolic and mitochondrial Zn2+ release. Exposure to a cell-penetrating, high-affinity Zn2+i chelator, TPEN, largely abolished the Zn2+i release and markedly protected myocytes from I/R-, ROS-, RNS-, or Zn2+/K+ (Zn2+i supplementation)-induced myocyte apoptosis for at least 24 h after TPEN removal. Flavonoids and U0126 (a MEK1/2 inhibitor) largely inhibited the myocyte apoptosis and the TPEN-sensitive I/R- or Zn2+i supplement-induced persistent extracellular signal-regulated kinase 1 and 2 (ERK1/2) phosphorylation, dephosphorylation of p-Ser9 on glycogen synthase kinase 3β (GSK-3β), and the translocation into and accumulation of p-Tyr216 GSK-3β and p53 in, the nucleus. Silencing of GSK-3β or p53 expression was cardioprotective, indicating that activation of the ERK–GSK-3β–p53 signaling pathway is involved in Zn2+-sensitive myocyte death. Moreover, the ERK-dependent Noxa–myeloid cell leukemia-1 (Mcl-1) pathway is also involved, as silencing of Noxa expression was cardioprotective and U0126 abolished both the increase in Noxa expression and in Mcl-1 degradation. Thus, acute upstream Zn2+i chelation at the start of reperfusion and the use of natural products, that is, flavonoids, may be beneficial in the treatment of cardiac I/R injury.
Similar content being viewed by others
Main
Zinc is an element critical to life and is involved in gene transcription and metalloenzyme function. However, the free form of the ion can be toxic and the intracellular free Zn2+ concentration ([Zn2+]i) is tightly regulated by membrane transporters and zinc-binding proteins, including high-affinity zinc-finger proteins and low-affinity cysteine-rich metallothioneins (MTs).1 Using a ratiometric biosensor, the basal [Zn2+]i in PC-12 cells has been shown to be in the picomolar range.2
Reactive oxygen species (ROS) (H2O2, OH•, and O2−•) and reactive nitrogen species (RNS) (NO• and ONOO−) are involved in several myocardial pathophysiological responses, including ischemia/reperfusion (I/R) injury.3, 4, 5 In an MT-overexpressing transgenic mouse model, the heart was found to be highly resistant to I/R-induced myocardial infarction.6 There is also evidence that NO•-induced Zn2+i release in neurons induces cell death, as NO• leads to ONOO− (peroxynitrite) formation and consequent Zn2+i release, followed by opening of the mitochondrial permeability transition pore (mPTP),7 resulting in neuron and glia apoptosis.7, 8 The molecular mechanism of Zn2+i release-induced neuronal cell death is not clear, but may involve activation of either p38-K+ channels or the extracellular signal-regulated kinase (ERK)–lipoxygenase (LOX)–ROS pathway.7, 8
When a non-acetoxymethyl ester Zn2+ indicator, TSQ, is applied to the heart tissues, reperfusion induces a decrease, rather than an increase, in [Zn2+]i levels.9, 10 When a mixture of Zn2+ and the Zn2+ ionophore pyrithione is added to the reperfusion solution for 20–30 min, cardioprotection occurs, and two mechanisms have been suggested, namely preservation of protein kinase C (PKC) isoforms and inhibition of mitochondrial metabolism.9, 10 The molecular mechanism for the effect of the [Zn2+]i increase on cell survival is therefore still debatable.
As the basal [Zn2+]i is extremely low,2 an understanding of the role of free zinc in living cells has been hindered by the lack of suitable imaging reagents. Using time-lapse confocal microscopy of cardiomyocytes and two sensitive Zn2+-selective probes FluoZin-3 AM (Kd=15 nM) and RhodZin3 AM (Kd=65 nM),11 this study is the first to show that I/R, ROS, and RNS all cause significant cytosolic and/or mitochondrial Zn2+i release. The role of altered zinc homeostasis in myocyte survival and the molecular mechanism involved was investigated.
Results
Both ROS and RNS induce intracellular Zn2+ (Zn2+i) release
Both ROS and RNS have been suggested to be involved in cardiac I/R injury.3, 4, 5 We tested whether direct exposure to ROS (e.g. H2O2) or RNS (e.g. ONOO−) stimulated Zn2+i release in normal Zn2+-free medium. Addition of H2O2 induced a marked increase in both the [O2−•]i (red line; ∼25-fold increase; Figures 1a, b and e) and the [Zn2+]i (green line; ∼45-fold increase; Figures 1a, b and f). Addition of ONOO− also induced an increase in the [O2−•]i and [Zn2+]i (Figures 1c, e and f).
A sustained increase in the [O2−•]i and [Zn2+]i is induced in FluoZin-3 AM, MitoSox Red, and MTG triple-loaded cardiomyocytes by addition of ROS, RNS, or Zn2+o. In b–d, the resting level of the [O2−•]i and [Zn2+]i is F/F0=1. (a and b) H2O2 (ROS) induces a sustained increase in the [O2−•]i (upper panels in a, red line in b) and [Zn2+]i (lower panels in a, green line in b). In a, a mitochondrion (MTG) is indicated by the arrowhead, while the region of interest (ROI) analyzed in the nuclei/cytosol (‘N’), but not the mitochondria, is indicated in the last frame. The small effect of baicalein (dotted red and green lines) on the H2O2-induced [O2−•]i and [Zn2+]i increases (solid red and green lines) is shown in b. (c) ONOO− (RNS) also induces a sustained increase in the [O2−•]i and [Zn2+]i. Pretreatment with NAC markedly inhibits both increases. (d) 1 μM Zn2+o/4 μM pyrithione causes a sustained increase in the [O2−•]i and [Zn2+]i (∼45-fold, solid lines). Note that MnTBAP inhibits the Zn2+o-induced [O2−•]i increase (dotted red line), but not the TPEN-sensitive [Zn2+]i increase (dotted green line). The [Zn2+]i increase, but not the [O2−•]I increase, is completely reversed by addition of TPEN at the end of the experiment (post-TPEN, b, c and d). (e and f) Summarized data. The vehicle controls contained 0.1% ethanol. A mitochondrial complex-III inhibitor, antimycin A, markedly inhibited the Zn2+o/K+-induced [O2−•]i increase (e), indicating that the O2−• production may be induced by an increase in [Zn2+]mito (cf. Supplementary Figure S1b), resulting in complex III activation (*P<0.05; n=6–9/group). For the concentrations of all reagents used, see the Supplemental Methods. The color reproduction of this figure is available at the Cell Death and Differention journal online
A cell-penetrating high-affinity Zn2+i chelator, TPEN (Kd for zinc=1.4 × 10−13 M at pH 7.0) was used to chelate release Zn2+i.1 When it was added to the extracellular medium during the plateau of the Zn2+i increase, a rapid decrease in the [Zn2+]i was seen (‘post-TPEN’; Figures 1b and c), indicating that TPEN can easily penetrate the plasmalemma. Cysteine-containing reagents (GSH or N-acetylcysteine (NAC)) and dithiothreitol (DTT) are also suggested to be zinc chelators,1, 12 and all three reagents largely inhibited the H2O2- and ONOO−-induced increases in the [Zn2+]i, whereas only NAC inhibited the [O2−•]i increase (Figures 1c, e and f, Supplementary Figure S1e).
An O2−•i chelator, MnTBAP, abolished both the H2O2- and the ONOO−-induced increase in the [O2−•]i and [Zn2+]i (Figures 1e and f), indicating that the [O2−•]i increase is upstream of the [Zn2+]i increase. Post-TPEN inhibited the [Zn2+]i increase, but not the [O2−•]i increase (Figures 1b, e and f), suggesting that the Zn2+i increase caused by the oxidants also induces the [O2−•]i increase and that both are prevented by pretreatment with TPEN (‘pre-TPEN’; Figures 1e and f), whereas post-TPEN occurs too late to prevent the [O2−•]i increase.
Positive feedback between the [O2−•]i and [Zn2+]i increases
Addition of either 20 μM Zn2+o to 100 mM K+/Ca2+-free EGTA medium11 (i.e. Zn2+i supplementation) or of 1 μM Zn2+o/4 μM pyrithione to normal medium9, 10 (Figure 1d) induced similar increases in the [O2−•]i and [Zn2+]i (Figures 1e and f) to those produced by H2O2 or ONOO−, and, when 10 μM Zn2+o in 40 mM K+/Ca2+-free EGTA medium was used, there was a smaller increase in the [O2−•]i and [Zn2+]i (∼20-fold, Figures 1e and f). MnTBAP abolished 20 μM Zn2+o-induced [O2−•]i increase, but not the [Zn2+]i increase (dashed lines; Figures 1d, e and f), showing that the Zn2+o influx is upstream of the [O2−•]i increase. These results thus suggest the existence of a positive feedback loop between the [Zn2+]i and [O2−•]i increases (Figure 8e).
The Zn2+i release induces TPEN-, flavonoid-, and ERK-glycogen synthase kinase-3β-sensitive myocyte apoptosis
When myocytes were exposed to H2O2 or ONOO−, or to 10 μM Zn2+/K+ for 4 h (Figure 2), and were returned to normal medium for 24 h after 4-h exposure to these reagents (Supplementary Figure S2c), marked TPEN-sensitive cytC release (Figures 2a and b), activation of z-DEVD.fmk-/z-VAD-sensitive caspases, nuclear condensation (Figure 2d, Supplementary Figures S2c and d), and nuclear fragmentation (TUNEL (+), Supplementary Figures S2a and b) were seen. Thus, oxidative stress, nitrosative stress, or Zn2+i supplementation all stimulated TPEN-sensitive myocyte apoptosis.
Exposure to ROS, RNS, or Zn2+o causes TPEN-, NAC-, DTT-, U0126-, and flavonoid-sensitive cytC release and caspase-dependent nuclear condensation. (a and b) CytC release. Anti-cytC antibody (green fluorescence within intact mitochondria, see ai: vehicle) was used to detect cytC release (arrowheads in aii) after addition of H2O2, ONOO−, or 10 ìM Zn2+/K+ for 4 h with or without inhibitors (b). (c and d) After addition of H2O2, ONOO−, or 10 ìM Zn2+/K+ for 4 h with or without inhibitors, caspase activation (green in c, arrowheads in cii) and nuclear condensation (condensed light blue nuclei, cii) were measured. (e) After transfection with siGSK-3ß or scrambled siRNA (marked ‘siControl’) for 72 h, cells were treated for 4 h with or without inhibitors, then caspase activation and nuclear condensation were measured. In b, d, and e, n=5–10/group. The color reproduction of this figure is available at the Cell Death and Differention journal online
We therefore examined possible molecular mechanism for the Zn2+i release-induced caspase-dependent apoptosis and found that three potent flavonoids (baicalein, luteolin, and fisetin) and commonly used antioxidants or Zn2+i chelators (MnTBAP, GSH, NAC, or DTT) all abolished the ROS/H2O2-, RNS/ONOO−, or Zn2+o-induced cytC release (Figures 2a and b) and caspase activation at 4 h (Figures 2c and d) or 24 h (Supplementary Figure S2c). Moreover, both baicalein and U0126, which failed to inhibit the H2O2-, ONOO−, or Zn2+o-induced ROS increase (in O2−• (Figure 1e); in H2O2 and OH• (Supplementary Figure S1g)) and Zn2+i release (Figure 1f), had a marked protective effect (Figures 2b and d, Supplementary Figure S2c). Another MEK/ERK inhibitor, PD98059, also inhibited cytC release (Figure 2b).
Glycogen synthase kinase-3β (GSK-3β) was recently suggested to have an important role in cardiac I/R injury. When the reperfusion injury salvage kinase (RISK) family members PKA, PKB/Akt, PKC, and MEK-ERK are activated by pre- or post-conditioning, a common downstream protein, GSK-3β, is phosphorylated at Ser9, resulting in GSK-3β inhibition (both events occurring within 20 min of the end of conditioning), leading to the inhibition of mPTPs and the salvaging of 20–50% live myocardium.4, 5, 13, 14, 15, 16 A potent GSK-3 inhibitor, SB216763 (SB21),4, 13 had a relatively weak protective effect against H2O2-, ONOO−-induced myocyte death (Supplementary Figure S2c), but gave better protection against 10 μM Zn2+-induced cell toxicity at 4 h (Figure 2d) or 24 h (Supplementary Figure S2c) of Zn2+o exposure. Transfection of cardiomyocytes with siGSK-3β for 48 or 72 h resulted, respectively, in knockdown of GSK-3β mRNA or protein (Figure 4d). After knockdown for 72 h, siGSK-3β had a significant protective effect against Zn2+/K+-induced myocyte apoptosis (Figure 2e), but little protective effect against H2O2- or ONOO−-induced apoptosis (2nd versus 3rd (+ siGSK-3β) paired bars, Figure 2e). Interestingly, TPEN or baicalein remained cardioprotective in the presence of GSK-3β knockdown (#P<0.05, Figure 2e), indicating that another Zn2+i-dependent, but GSK-3β-independent pathway may exist.
TPEN, NAC, DTT, U0126, flavonoids, or GSK-3β inhibitors abolish simulated I/R-induced apoptosis. (a and b) If not otherwise specified, the inhibitor was only present during the 4-h reperfusion. Caspase activation (green and arrowheads) and nuclear condensation (light blue and condensed nuclei) are shown in aii. (c–e) Myocytes were transfected with 100 nM siGSK-3β for 48 or 72 h, respectively, resulting in knockdown of GSK-3β mRNA or protein (d and inset). At 72 h after transfection with siRNA or control scrambled siRNA, inhibitors were added for 4 h during the reperfusion period. (e) Summarized data; n=7–10/group
Simulated I/R also induces Zn2+i release, resulting in TPEN-, ERK-, GSK-3β-, and flavonoids-sensitive myocyte apoptosis
After continuous perfusion with simulated ischemic solution for 40 min (starting at ‘I’ in Figures 3a and b), the perfusate was switched to oxygen-containing reperfusion solution for ∼50–60 min (starting at ‘R’), and a sustained increase in both the [O2−•]i (upper panels) and [Zn2+]i (lower panels, Figures 3a and b) was seen, which was similar in size to the [O2−•]i and [Zn2+]i increases (∼20-fold) caused by exposure to 10 μM Zn2+. Again, post-TPEN largely reversed the reperfusion-induced [Zn2+]i overload, but not the [O2−•]i overload (Figures 3b, e and f).
Simulated I/R also induces increases in the [O2−•]i and [Zn2+]i. (a and b) Simulated ischemia (‘I’) has little effect on the [O2−•]i and [Zn2+]i, while reperfusion (‘R’) induces a similar increase in the [O2−•]i and [Zn2+]i (∼20-fold) to that induced by 10 μM Zn2+/40 mM K+ (cf. Figures 1e and f). The reperfusion-induced [O2−•]i increase (solid or dashed red line) is not inhibited by baicalein (dashed red line in b) or post-treatment with TPEN (solid and dashed red lines in b), by SB21 (solid red line in c), or by GSH (solid red line in d), but is inhibited by NAC (dashed red line in d). The [Zn2+]i increase (solid and dashed green lines) is inhibited by post-treatment with TPEN (b), GSH (solid green line in d), or NAC (dashed green line in d), but not by baicalein (dashed green line in b) or SB21 (c). (e and f) Summarized data. The data are the mean±SEM; n=6–8/group
Pretreatment with MnTBAP also markedly inhibited the reperfusion-induced [O2−•]i and [Zn2+]i overloads (Figures 3e and f), again, indicating that the [O2−•]i overload is upstream of the Zn2+i release. Pretreatment with GSH markedly inhibited the [Zn2+]i overload, but not the [O2−•]i overload, while NAC inhibited both overloads (Figure 3d). As GSH and NAC are both cysteine-rich reagents, the inhibitory effect on the [Zn2+]i increase, but not the [O2−•]i overload, was possibly due to acceleration of Zn2+ re-uptake by cysteines, as shown in an in vitro study.1 In contrast, when a mixture of 1 μM Zn2+/4 μM pyrithione was added for ∼30 min at the start of reperfusion, [O2−•]i overload and a more marked increase in the [Zn2+]i (>65-fold) were seen (Figures 3e and f), indicating additional Zn2+o influx when Zn2+o/pyrithione was applied.
We next investigated whether the TPEN-/NAC-/GSH-sensitive Zn2+i increase/release (Figures 3d and f) had an effect on cell survival after simulated I/R exposure. The experiments shown in Figures 4a and b (caspase activation and nuclear condensation) and supplemental Figures S2a and b (TUNEL test) were performed as follows: after ischemia for 40 min, followed by reperfusion for 4 h, myocytes were returned to normal medium without inhibitors for 24 h, then were examined for apoptotic markers. Compared with I/R alone (‘I/R’, Figure 4b), the presence of 15 μM TPEN at the start of reperfusion for only ∼20 min (‘TPEN (20 min)’) markedly inhibited I/R injury at 24 h after TPEN removal, suggesting that the reperfusion-induced initial Zn2+i release (Figure 3b) is important in I/R injury. When 15–50 μM TPEN was present throughout the 4 h reperfusion period, surprisingly, it almost completely abolished apoptosis at 24 h (Figures 4a and b, Supplementary Figures S2a and b). In contrast, when Zn2+/pyrithione was added for only ∼20 min at the beginning of reperfusion, it had little protective effect for both cardiomyocytes and H9c2 cells (Figures 4a and b; Supplementary Figures S2a and b). Inclusion of any of three potent flavonoids or U0126 for 4 h in the reperfusion solution again had a marked cardioprotective effect for at least 24 h (Figures 4a and b; Supplementary Figures S2a and b), while Ca2+-free medium (inhibition of I/R-induced Ca2+i overload),5 CsA (an mPTP inhibitor),13 diazoxide (an mKATP opener),7 or MK886 (a selective 5-LOX inhibitor8) were less protective (Figures 4a and b).
We confirmed that GSK-3 inhibitors (SB21 or LiCl) and antioxidants exhibited significant cardioprotection in myocytes (Figure 4b). When GSK-3β was selectively knocked down by transfection with siGSK-3β (Figure 4d), significant protection against I/R injury for 24 h was seen (Figures 4c and e, 4th versus 3rd groups of darker paired bars). TPEN treatment with or without protein knockdown was again more cardioprotective than SB21 treatment (#P<0.05; Figure 4e), while LiCl, baicalein, or fisetin had a similar protective effect to SB21.
The Zn2+i release may also be involved in I/R injury in adult-rat hearts
Figure 5 shows that, when 15, 30, and 50 μM TPEN was used, 15 μM TPEN was the most effective, with a reduction in global infarct area of ∼65%. The protective effect of baicalein was similar to that of the GSK-3 inhibitor LiCl. Compared with LiCl alone, co-addition of TPEN resulted in a small, but significant, additional protective effect (11.5±0.4%, #P<0.05), again suggesting that another Zn2+i-dependent, but GSK-3β-independent pathway may exist.
Both TPEN and baicalein have a marked protective effect in adult-rat hearts. (a) After 30 min of ischemia, TPEN or baicalein was added to the reperfusion solution for 2 h. The vehicle was 0.1% ethanol. In the group receiving LiCl (a GSK-3 inhibitor), 10 mM NaCl in the reperfusion solution was replaced with 10 mM LiCl. (b) Compared with the LiCl group, the mixture of LiCl and TPEN provides extra protection (#P<0.05). Infarct size was determined as the percentage of white tissue in the total cross-section area (arrowheads in a)
The ERK-dependent GSK-3β–p53 pathway and Noxa–myeloid cell leukemia signaling are both involved in the Zn2+i increase-induced myocyte death
In neurons, it has been suggested that the Zn2+i release activates the ERK–LOX–ROS cascade, resulting in neuronal apoptosis.8 In Supplementary Figures S4 and S5, we have ruled out a possible role for lipoxygenase, nuclear factor κB (NFκB), or hypoxia-inducible factor-1 (HIF1α) on the Zn2+i increase-induced myocyte death. As U0126 and TPEN were both cardioprotective and also there is little information whether the I/R-induced Zn2+i increase activates both ERK and GSK-3β, resulting in myocyte apoptosis, we tested this hypothesis.
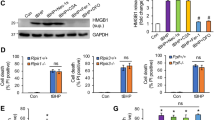
In cardiomyocytes (Figure 6A) or H9c2 cells (Supplementary Figure S3b), Zn2+i supplementation caused an early increase in p-ERK1/2 levels at 2 h or 20 min, respectively, and p-ERK1/2 levels remained high for 2–5 h thereafter. This persistent increase in p-ERK1/2 levels was abolished by TPEN or U0126, but not by baicalein or MnTBAP (Figures 6a and b; Supplementary Figures S3a and b).
Inhibitory effects of TPEN, U0126, or flavonoids on the I/R- and Zn2+o-induced activation of ERK1/2 and GSK-3β in cardiomyocytes. (A) Western blot showing the time course of the effect of Zn2+i supplementation on ERK1/2 and GSK-3β activity. (B) TPEN, U0126, or baicalein inhibits the 10 μM Zn2+/K+-induced activation of ERK1/2 and GSK-3β (i.e. p-Ser9 decrease and p-Try216 increase) at 4 h of treatment. (C and D) Time course of the simulated I/R-induced activation of ERK1/2 (Ca) and GSK-3β (Cb) and the summarized data (D). (E) TPEN and baicalein abolish the I/R-induced activation of p-ERK1/2 (Ea) and GSK-3β (Eb) at 4 h of reperfusion. (F) Summarized data for the phosphorylation of GSK-3β. Data are taken from B and E. In D and F, n=5–8/group
In non-cardiac cells, it has been suggested that GSK-3β dephosphorylation at Ser9 and/or its phosphorylation at Tyr216 increases the activity of the enzyme.17, 18 In adult-rat hearts, however, phosphorylation of Tyr216 in GSK-3β does not change after 5 min of reperfusion.14 After short Zn2+i supplementation of cardiomyocytes for 2 h (Figure 6A) or of H9c2 cells for 20 min (Supplementary Figure S3b), a simultaneous increase in p-ERK1/2 and p-Ser9 GSK-3β (GSK-3β inhibition) was seen. However, when the p-ERK1/2 increase lasted for 3–5 h, dephosphorylation of p-Ser9 and phosphorylation of p-Try216 on GSK-3β were seen (Figure 6A, Supplementary Figure S3b), indicating that a long-lasting [Zn2+]i increase unexpectedly activated both ERK1/2 and GSK-3β. Moreover, TPEN (Figure 6B, Supplementary Figure S3b), U0126 (Figure 6B), or baicalein (Figure 6F) largely inhibited GSK-3β activation in cardiomyocytes by increasing p-Ser9 GSK-3β levels, but there was no statistically significant reduction in p-Tyr216 GSK-3β levels (Figure 6F, Zn2+o versus inhibitors, #P<0.05).
Using I/R in cardiomyocytes, a similar response of a persistent p-ERK1/2 increase (Figure 6Ca) and dephosphorylation of Ser9 and phosphorylation of Tyr216 on GSK-3β (Figures 6Cb–D) was seen during 2–5 h of reperfusion. TPEN abolished the I/R-induced persistent p-ERK1/2 increase (Figure 6Ea) and reversed the Ser9 dephosphorylation and Tyr216 phosphorylation (Figures 6Eb–F). Baicalein (Figures 6Eb–F) or leuteolin (data not shown) reversed the dephosphorylation of p-Ser9. Thus, the target of the flavonoids is probably a protein downstream of ERK1/2, for example, GSK-3β (Figure 8e). All three inhibitors reduced the mean p-Tyr216 GSK-3β value, but only TPEN had a significant effect (Figure 6F), as the intensity of the p-Tyr216 band varied between batches of primary myocytes.
Figure 7a shows confocal images demonstrating that I/R treatment for 4 h induced an increase in p-Tyr216 GSK-3β levels in myocyte nuclei (arrow in Aii; 26.7±1.8%, n=6) and that this increase was abolished by TPEN (3.5±0.6%, n=6) or baicalein (8.6±0.6%, n=6). A similar inhibitory effect of TPEN or U0126 (both <5%, n=5, Figure 7biii) on Zn2+/K+-induced p-Tyr216 GSK-3β translocation in myocyte nuclei was also seen (arrow in Figure 7bii; 23.6(3.8%, n=5). After I/R exposure for 4 h, followed by a return to normal medium for 24 h (Figure 7cii), an increase in co-expression of GSK-3β (green) and p53, a GSK-3β substrate protein (red), was seen in nuclei (overlay/yellow: I/R: 25.5±3.1%, n=6), and this effect was again inhibited by TPEN (5.1±2.4%, n=5, Figure 7ciii) or baicalein (7.3±2.6%, n=4). A similar inhibitory effect of TPEN (3.4±1.7%, n=4) or baicalein (11.3±2.6%, n=4) was also seen after Zn2+/K+ exposure for 4 h and return to normal medium for 24 h (36.3±2.5%, n=9, Figure 7dii).
Simultaneous activation of GSK-3β and p53 and an increase in Noxa expression are involved in Zn2+i increase-induced myocyte death. (a–d) Representative confocal microscopic images of p-Tyr216 GSK-3β translocation into the myocyte nucleus (a and b) and GSK-3β–p53 activation (c and d). TPEN, U0126, baicalein, or PFT-α (a p53 inhibitor) inhibit the increase in p-Tyr216 in myocyte nuclei (punctate green fluorescence, arrowhead in a and b) or the colocalization of GSK-3β (green) and p53 (red) in nuclei (yellow, arrowhead in c and d). (e) Treatment with either PFT-α or sip53 is protective against I/R-, 10 μM Zn2+/K+-, H2O2-, or ONOO−-induced myocyte death. n=4–8/group. (f) Time course of the induction of an increase in Noxa mRNA caused by 10 μM Zn2+/K+ exposure measured by quantitative real-time PCR (qPCR). (g) U0126 or SB21, but not PFT-α, abolishes the increase in Noxa expression at 4 h of Zn2+i supplementation
Pifithrin-α PFT-α inhibits the p53-dependent transactivation of p53-responsive genes and reversibly blocks p53-mediated apoptosis.19 Pretreatment with PFT-α largely inhibited the Zn2+/K+-induced p53 expression (P<0.05; 55.0±2.7% versus 25.8±1.9%, n=5) and GSK-3β/p53 co-expression in nuclei (P<0.05; 36.3±2.5% versus 19±1.5%, n=9 and 5, respectively, Figure 7diii), but had little effect on the expression of GSK-3β per se (P>0.05; 68.5±2.7% versus 60±4.1%, n=5). PFT-α also significantly inhibited TPEN-sensitive I/R-, H2O2-, ONOO−-, or Zn2+/K+-induced myocyte death (*P<0.05, 2nd versus 4th groups of lighter paired bars (−siRNA) in Figure 7e). Moreover, silencing of p53 expression by sip53 transfection also provided significant cardioprotection (#P<0.05, 1st versus 2nd groups of darker paired bars (+siRNA) in Figure 7e). Taken together, these data suggest that activation of ERK-dependent GSK-3β–p53 signaling is involved in the Zn2+i increase-induced myocyte death.
It has been suggested that the apoptotic protein Noxa is a transcriptional target of p53.20 An anti-apoptotic Bcl-2 family protein, myeloid cell leukemia-1 (Mcl-1), has a high affinity for Noxa and binds to it, thus decreasing its apoptotic activity.20, 21 Moreover, activation of the Noxa–Mcl-1 pathway was recently implicated in non-cardiac cell death caused by DNA-damaging agents, including H2O2 and cisplatin.21, 22 Figures 7f and g show that exposure to Zn2+/K+ resulted in a transient increase in Noxa mRNA levels, which peaked at 4 h. The I/R or H2O2 exposure also induced a marked increase in Noxa mRNA levels (Supplementary Figures S3c and d). Interestingly, this increase was largely inhibited by U0126 or SB21, but not by PFT-α (Figure 7g, Supplementary Figure S3c), suggesting that the Zn2+i increase induces ERK-/GSK-3-dependent, but p53-independent, Noxa expression (Figure 8e). Furthermore, TPEN, U0126, SB21 (Figures 8b and c), or baicalein (Supplementary Figure S3f) simultaneously abolished the I/R- or Zn2+i supplement-induced increase in Noxa protein levels, and decrease in Mcl-1 protein levels. Moreover, the Zn2+i supplementation-induced Mcl-1 decrease was inhibited by a proteosomal inhibitor MG132 (Figure 8a), indicating that the decrease is due to an increase in proteosomal degradation (Figure 8e). The cell death assay also demonstrated that silencing of Noxa expression resulted in significant cardioprotection against I/R-, H2O2-, ONOO−-, or Zn2+/K+-induced apoptosis (Figure 8d), while knockdown of Mcl-1 did not. Interestingly, an additional small protective effect was consistently observed when SB21 or PFT-α was present after silencing Noxa expression for 65–72 h (Figure 8d), indicating that both the Noxa–Mcl-1 and GSK-3β–p53 axes, which are downstream of the activated ERK1/2, are involved in the myocyte death (Figure 8e). We did not perform double knockdown experiments in Figure 8d, as cardiomyocytes transfected with both siRNAs were not healthy after 65–72 h transfection. SB21 or siGSK-3β had only a small, or no, protective effect against H2O2-/ONOO−-induced cell death (Figures 2d and e, Supplementary Figure S2c); the reason for this is not known, but the larger Zn2+i release caused by exposure to H2O2- or ONOO− may activate ERK–p53–Noxa-dependent, but GSK-3β-independent, signaling (Figures 7e, 8d and e).
(a–c) The Zn2+i increase induces both Noxa protein expression and MG132-sensitive Mcl-1 protein degradation, and these effects are blocked by pretreatment with TPEN, U0126, or SB21 (a and b). Zn2+i supplementation induces p-ERK activation and GSK-3β dephosphorylation/inhibition (b and c). (d) Noxa expression is involved in the I/R-, 10 μM Zn2+/K+-, H2O2-, or ONOO−-induced myocyte death. Silencing of Noxa expression for 65–72 h (marked siNoxa) induces significant protection against myocyte apoptosis (*P<0.05). SB21 or PFT-α provides additional myocyte protection after silencing of Noxa protein (#P<0.05). (e) Schematic diagram showing that oxidative stress and nitrosative stress both induce Zn2+i release, resulting in TPEN- and flavonoid-sensitive myocyte apoptosis. There is a positive feedback loop between the [Zn2+]i and [O2−•]i increases. Two independent pathways downstream of the Zn2+i increase-induced ERK activation are probably involved in the myocyte death, although other mechanisms are not ruled out (see Discussion). The flat-tipped blue arrows represent inhibition, while the red arrows represent stimulation or an increase
Discussion
Oxidative stress and nitrosative stress are both considered as major causes of cardiac I/R injury.3, 4, 5 This study provides two novel results: (i) using time-lapse confocal microscopy and high-affinity Zn2+-selective fluorescent probes, I/R, ROS, and RNS were found to cause marked endogenous Zn2+i release, which increased ERK1/2 activity, resulting in the activation of both GSK-3β–p53 and Noxa–Mcl-1 signaling and myocyte death (Figure 8e); and (ii) short exposure to TPEN or flavonoids at the start of reperfusion may have beneficial therapeutic potential.
When myocytes were treated with simulated I/R, ROS, or RNS, all caused significant TPEN-sensitive Zn2+i release, with positive feedback between the [Zn2+]i and [O2−•]i increases (Figures 1d and 8e). At least two independent Zn2+i pools were found to be located in the cytosolic and mitochondrial compartments, respectively, and the released Zn2+ translocated between the two compartments (Supplementary Figures S1c and d), as shown previously in neurons.11
When TPEN was applied for only 20 min at the beginning of the 4-h reperfusion, there was a marked protective effect that lasted for at least 24 h (Figure 4b, Supplementary Figure S2b), suggesting that the initial Zn2+i release, evoked by a burst of O2−•i at the beginning of reperfusion (Figure 3b), is an important early death signal for the I/R injury seen at 24 h. When TPEN was applied throughout the 4-h reperfusion period, it provided more cardioprotection than other treatments, including GSK-3 inhibition, flavonoids, Ca2+-free medium, CsA, or diazoxide (Figure 4b). TPEN also markedly abolished the Zn2+i-dependent H2O2- or ONOO−-induced apoptosis. Moreover, three membrane-permeating thiols (GSH, NAC. and DTT), which prevent oxidation of protein sulfhydryl groups,1, 12 all abolished the marked Zn2+i release, but only NAC inhibited the [O2−•]i increase. As these reagents were all cardioprotective, again, this indicates that NAC-/GSH-/DTT-induced intracellular Zn2+ chelation may prevent the myocyte death. In contrast, when a Zn2+/pyrithione mixture was added to the reperfusion solution for ∼30 min, a much larger [Zn2+]i increase was seen, and marked apoptosis was seen at 24 h after its addition to the reperfusion solution for only 20 min (Figure 4b, Supplementary Figure S2b).
There is mounting evidence in adult-rat hearts that within 20–30 min of the end of pre- or post-conditioning, RISK family members are activated, resulting in phosphorylation of GSK-3β at Ser9 (i.e. GSK-3β inhibition), which protects the adult-rat heart from I/R injury for 2–4 h.4, 13, 14, 15, 16 This study showed a link between the Zn2+i release/increase and the activation of GSK-3β, resulting in myocyte apoptosis. We observed an early increase in p-Ser9 GSK-3β levels after Zn2+i supplementation of cardiomyocytes for 2 h or of H9c2 cells for 20 min, in agreement with the results of Xu and co-workers23, 24 in H9c2 cells that Zn2+i supplementation for 20 min induces phosphorylation at Ser9. However, we found that this increase disappeared after 3–5 h of Zn2+i supplementation and was followed by full activation of GSK-3β by dephosphorylation of Ser9 and phosphorylation/translocation of Tyr216 (Figure 6A, Supplementary Figure S3b), resulting in the accumulation of both GSK-3β and PFT-α-sensitive p53 in myocyte nuclei. TPEN, U0126, or flavonoids abolished the I/R- or Zn2+i supplementation-induced GSK-3β activation and the accumulation of GSK-3β and p53 in the nucleus (Figures 7A–D). Moreover, treatment with PFT-α or silencing of p53 expression significantly protected myocytes from TPEN-sensitive I/R-, H2O2-, ONOO−-, or Zn2+/K+-induced cell death (Figure 7e). These data indicate that the GSK-3β–p53 pathway may be involved in the myocyte death. As short exposure to 0.1–10 ìM Zn2+o alone or its addition to the reperfusion solution for 20 min both induced significant TPEN-/NAC-/DTT-sensitive apoptosis at 24 h (Figure 4b, Supplementary Figure S2b), we conclude that Zn2+i supplementation-induced early phosphorylation at Ser9 is not necessarily cardioprotective and may induce cytotoxicity after return to normal medium for 4 or 24 h. In support of the above conclusions, Tyr216 phosphorylation is required for nuclear GSK-3β accumulation in neurons and fibroblasts,17, 18 as mutation of Tyr216 to phenylalanine or its dephosphorylation results in less GSK-3β being found in nuclei.17 In addition, the increase in GSK-3β in the nucleus stabilizes one of its substrate proteins, p53, which forms a complex and promotes neuronal apoptosis.18, 25 Thus, the modulation of Tyr216 GSK-3β may be as important as that of Ser9 in myocyte apoptosis.
Early activation of MEK1/2–ERK1/2 signaling is a protective upstream signal that induces phosphorylation of GSK-3β Ser9, resulting in cardioprotection.5, 16 However, a sustained p-ERK1/2 increase has been demonstrated to induce cell apoptosis in many non-cardiac cells.21, 22, 26 We found that both TPEN and U0126 inhibited not only the persistent p-ERK1/2 increase but also reversed Ser9 dephosphorylation and Tyr216 phosphorylation, resulting in an inhibition of the I/R- and Zn2+i supplement-induced GSK-3β activation (Figure 6). As TPEN, U0126, and PD98059 were all cardioprotective, one possible explanation is that the Zn2+i increase-stimulated persistent ERK1/2 activation, resulting in fully activated GSK-3β (e.g. at Try216), has a role in the myocyte apoptosis (Figure 8e). However, it is currently unclear how zinc causes ERK activation/phosphorylation. It has been suggested that, in non-cardiac cells, Ras and/or Raf might be the upstream kinases causing zinc-induced ERK phosphorylation, as treatment with a Raf-1 kinase inhibitor or infection with recombinant virus expressing dominant-negative mutants of MEK both attenuate Zn2+-dependent ERK phosphorylation.8, 27 However, further studies are required as regards cardiac I/R injury.
The Noxa–Mcl-1 pathway was recently implicated in cell death caused by DNA-damaging agents, for example, H2O2 or cisplatin.21, 22 This study showed that TPEN or U0126 was consistently more protective against H2O2- or ONOO−-induced myocyte apoptosis than SB21 or siGSK-3β, indicating that a GSK-3β-insensitive mechanism is involved. As we found that (i) U0126 abolished the I/R or Zn2+i supplementation-induced Noxa mRNA/protein expression and MG132-sensitive Mcl-1 degradation (Figures 7g, 8b and c, Supplementary Figure S3c), and (ii) significant myocyte protection was seen after silencing of Noxa expression, but not of Mcl-1 expression (Figure 8d), the ERK-dependent Noxa–Mcl-1 pathway is also involved in myocyte death (Figure 8e). Furthermore, activation of GSK-3β–p53 and Noxa–Mcl-1 signaling are two independent pathways downstream of the Zn2+-dependent ERK1/2 activation (Figure 8e), as PFT-α had little effect on Noxa mRNA expression and additional cardioprotection by either SB21 or PFT-α was observed after knockdown of Noxa (Figures 7g and 8d).
There is evidence that Mcl-1 contains an evolutionarily conserved GSK-3 site,28 and activated GSK-3β has been suggested to physically associate with, and phosphorylate, Mcl-1 at Ser159, which then facilitates the ubiquitination and degradation of p-Mcl-1 and contributes to GSK-3β-induced apoptosis.28, 29 Surprisingly, we found that baicalein or SB21 had a similar inhibitory effect against the Zn2+i-dependent GSK-3β activation and both abolished the increase in Noxa mRNA/protein and the decrease in Mcl-1 protein (Figures 6F, 7g, 8b and c, Supplementary Figures S3c and f). The cell death assay showed that knockdown of the apoptotic protein Noxa resulted in cardioprotection, while knockdown of the anti-apoptotic protein Mcl-1 resulted in increased myocyte death. As baicalein and SB21 were both cardioprotective, inhibition of the activated GSK-3β–Noxa–Mcl-1 signaling might be involved in the cardioprotection (Figure 8e). The molecular mechanism is unclear, and possible interactions between GSK-3β, Noxa, and Mcl-1 contribute to the myocyte death need further investigation. However, other possibilities cannot be ruled out at present. For example, the larger Zn2+i release, induced by H2O2 or ONOO− exposure, activated ERK–p53–Noxa-dependent, but GSK-3β-independent, signaling (Figures 7e, 8d and e).
In summary, this study shows that I/R or oxidative and nitrosative stress all induce marked Zn2+i release, resulting in ERK1/2-activated GSK-3β–p53 and Noxa–Mcl-1 signaling and myocyte death. Inhibition of the reperfusion-induced upstream Zn2+i release or the use of natural products, flavonoids, are potentially promising strategies for the treatment of cardiac I/R injury.
Materials and Methods
Solutions and chemicals
The Zn2+o-free normal Tyrode solution used was (in mM): NaCl 118, KCl 4. 5, MgCl2 1.0, CaCl2 1.8, glucose 10, and HEPES 10, pH 7.4 at 37 °C. See the Supplemental Materials for the concentration of the reagents used in this study.
Protocols for simulating I/R in cardiomyocytes or I/R in adult-rat hearts
Cultured neonatal ventricular myocytes
All procedures were performed in accordance with the Animal Care Guidelines of the National Taiwan University. The protocol for simulated I/R was modified from that described previously.4 In brief, myocytes were stabilized in O2 (21%)-Tyrode solution for 10 min, then were switched to 100% N2-saturated Tyrode solution for 30 min, followed by reperfusion for 4 h with O2-Tyrode solution.
Isolated adult-rat hearts
Adult rats were anesthetized and the isolated hearts retrogradely perfused in Langendorff mode. Adult-rat hearts were then subjected to 30 min of global ischemia by halting perfusion, followed by 2 h of reperfusion with Krebs–Henseleit bicarbonate buffer gassed with 95% O2/5% CO2 at 37 °C (pH 7.4).
Simultaneous measurement of changes in the [O2−•]i and [Zn2+]i using time-lapse confocal microscopy
A Leica SP confocal laser scanning imaging system (Leica Microsystems, Wetzlar, Germany) equipped with a 63 × oil-immersion objective was used. FluoZin-3 AM (green) and MitoSox Red (red) were co-loaded with MTG into cardiomyocytes to simultaneously detect dynamic changes in the [O2−•]i and [Zn2+]i. MitoSox Red is a high affinity and selective fluorescent probe for the [O2−•]i. TSQ is a non-acetoxymethyl ester Zn2+ indicator. Although it is a very sensitive Zn2+ probe (Kd=10 nM),10 it does not depend on cleavage of an acetoxymethyl ester group for uptake and fluorescence, so intracellular TSQ leaks out within a few minutes and it is not possible to measure sequential fluorescent changes.30 The rest of recording detail, please see Supplemental Methods.
For western blot analysis, siRNA transfection, qPCR measurement, and detection of apoptosis, see the Supplemental Materials.
Statistics
All values are presented as the mean±SEM of N independent experiments. All data were subjected to one-way ANOVA followed by a post hoc test with the Bonferroni's correction. P<0.05 was considered to be statistically significant.
Abbreviations
- I/R injury:
-
ischemia/reperfusion injury
- ROS:
-
reactive oxygen species
- RNS:
-
reactive nitrogen species
- Zn2+i:
-
intracellular free Zn2+ ions
- TPEN, N,N,N′,N′:
-
tetrakis (2-pyridylmethyl) ethylenediaminepentaethylene
- NAC:
-
N-acetylcysteine
- DTT:
-
dithiothreitol
- MT:
-
metallothionein
- mPTP:
-
mitochondrial permeability transition pore
- PFT-α:
-
pifithrin-α
- MEK1/2:
-
kinase mitogen protein kinase kinase 1 and 2
- ERK1/2:
-
extracellular signal-regulated kinase 1 and 2
- GSK-3β:
-
glycogen synthase kinase-3β
- Mcl-1:
-
myeloid cell leukemia-1
- LOX:
-
lipoxygenase
- NFκB:
-
nuclear factor κB
- HIF1α:
-
hypoxia-inducible factor-1
- PKC:
-
protein kinase C
References
Maret W, Vallee BL . Thiolate ligands in metallothionein confor redox activity on Zn2+ chelators. Proc Natl Acad Sci 1998; 95: 3478–3482.
Bozym RA, Thompson RB, Stoddard AK, Fierke CA . Measuring picomolar intracellular exchangeable zinc in PC-12 cells using a ratiometric fluorescence biosensor. ACS Chem Biol 2006; 1: 103–111.
Cheung P-Y, Wang W, Schulz R . Glutathione protects against myocardial ischemia-reperfusion injury by detoxifying peroxynitrite. J Mol Cell Cardiol 2000; 32: 1669–1678.
Juhaszova M, Zorov DB, Kim S-H, Pepe S, Fu Q, Fishbein KW et al. Glycogen synthase kinase-3β mediates convergence of protection signaling to inhibit the mitochondrial permeability transition pore. J Clin Invest 2004; 113: 1535–1549.
Yellon DM, Hausenloy DJ . Myocardial Reperfusion Injury. N Engl J Med 2007; 357: 1121–1135.
Kang YJ, Li G, Saari JT . Metallothionein inhibits ischemia-reperfusion injury in mouse heart. Am J Physiol 1999; 26: H993–H997.
Bossy-Wetzel E, Talantova MV, Lee WD, Schölzke MN, Harrop A, Mathews E et al. Crosstalk between nitric oxide and zinc pathways to neuronal cell death involving mitochondrial dysfunction and p38-activated K+ channels. Neuron 2004; 41: 351–365.
Zhang Y, Wang H, Li J, Dong L, Xu P, Chen W et al. Intracellular zinc release and ERK phosphorylation are required upstream of 12-lipoxygenease activation in peroxynitrite toxicity to mature rat oligodendrocytes. J Biol Chem 2006; 281: 9460–9470.
Mclntosh R, Lee SY, Ghio AJ, Xi J, Zhu M, Shen X et al. The critical role of intracellular zinc in adenosine A2 receptor activation induced cardioprotection against reperfusion injury. J Mol Cell Cardiol 2010; 49: 41–47.
Karagulova G, Yue Y, Moreyra A, Boutjdir M, Korichneva I . Protective role of intracellular zinc in myocardial ischemia/reperfusion is associated with preservation of protein kinase C isoforms. JPET 2007; 321: 517–525.
Sensi SL, Ton-That D, Sullivan PG, Jonas EA, Gee KR, Kaczmarek LK et al. Modulation of mitochondrial function by endogenous Zn2+ pools. Proc Natl Acad Sci 2003; 100: 6157–6162.
Cornell NW, Crivaro KE . Stability constant for the zinc-dithiothreitol complex. Analy Biochem 1972; 47: 203–208.
Das S, Wong R, Rajapakse N, Murphy E, Steenbergen C . Glycogen synthase kinase 3 inhibition slows mitochondrial adenine nucleotide transport and regulates voltage-dependent anion channel phosphorylation. Circ Res 2008; 103: 983–991.
Gross ER, Hsu AK, Gross GJ . Opioid-Induced cardioprotection occurs via glycogen synthase Kinase β inhibition during reperfusion in intact rat hearts. Circ Res 2004; 94: 960–966.
Gomez L, Paillard M, Thibault H, Derumeaux G, Ovize M . Inhibition of GSK-3β by postconditioning is required to prevent opening of the mitochondrial permeability transition pore during reperfusion. Circulation 2008; 117: 2761–2768.
Miura T, Miki T . GSK-3β, a therapeutic target for cardiomyocyte protection. Circ J 2009; 73: 1184–1192.
Yook JI, Li X-Y, Ota I, Hu C, Kim HS, Kim NH et al. A Wnt–Axin2–GSK3β cascade regulates Snail1 activity in breast cancer cells. Nat Cell Biol 2006; 8: 1398–1406.
Beurel E, Jope BS . The paradoxical pro-and anti-apoptotic actions of GSK3 in the intrinsic and extrinsic apoptosis signaling pathways. Prog in Neurobiol 2006; 79: 173–189.
Lin T, Mak NK, Yang MS . MAPK regulate p53-dependent cell death induced by benzo[a]pyrene: involvement of p53 phosphorylation and acetylation. Toxicology 2008; 247: 145–153.
Taylor RC, Cullen SP, Martin SJ . Apoptosis: controlled demolition at the cellular level. Nat Rev Mol Cell Biol 2008; 9: 231–241.
Sheridan C, Brumatti G, Elgendy M, Brunet M, Martin SJ . An ERK-dependent pathway to Noxa expression regulates apoptosis by platinum-based chemotherapeutic drugs. Oncogene 2010; 29: 6428–6441.
Aikawa T, Shinzawa K, Tanaka N, Tsujimoto Y . Noxa is necessary for hydrogen peroxide-induced caspase-dependent cell death. FEBS Letters 2010; 584: 681–688.
Chanoit G, Lee SR, Xi J, Zhu M, McIntosh RA, Mueller RA et al. Exogenous zinc protects cardiac cells from reperfusion injury by targeting mitochondrial permeability transition pore through inactivation of glycogen synthase kinase-3β. Am J Physiol 2008; 295: H1227–H1233.
Lee SY, Chanoit G, McIntosh R, Zvara DA, Xu Z . Molecular mechanism underlying Akt activation in zinc-induced cardioprotection. Am J Physiol 2009; 297: H569–H575.
Eom TY, Roth KA, Jope RS . Neural precursor cells are protected from apoptosis induced by trophic factor withdrawal or genotoxic stress by inhibitors of glycogen synthase kinase 3. J Biol Chem 2007; 282: 22856–22864.
Cagnol S, Chambard J-C . ERK and cell death: mechanisms of ERK-induced cell death–apoptosis, autophagy and senescence. FEBS J 2010; 277: 2–21.
Kohda Y, Matsunaga Y, Shiota R, Satoh T, Kishi Y, Kawai Y et al. Raf-1/Mek/ERK1/2 signaling pathway in zinc-induced injury in rat renal cortical slices. J Toxicol Sci 2006; 31: 207–217.
Maurer U, Charvet C, Wagman AS, Dejardin E, Green DR . Glycogen synthase kinase-3 regulates mitochondrial outer membrane permeabilization and apoptosis by destabilization of Mcl-1. Mol Cell 2006; 21: 749–760.
Ding Q, He X, Hsu J-M, Xia W, Chen C-T, Li L-Y et al. Degradation of Mcl-1 by β-TrCP mediates glycogen synthase kinase 3-induced tumor suppression and chemosensitization. Mol Cell Biol 2007; 27: 4006–4017.
Frederickson CJ, Burdette SC, Frederickson CJ, Sensi SL, Weiss JH, Yin HZ et al. Method for identifying neuronal cells suffering zinc toxicity by use of a novel fluorescent sensor. J Neurosci Methods 2004; 139: 79–89.
Acknowledgements
We gratefully thank the National Science Council of Taiwan for financial support (grants: NSC-98-2320-B-002-042-MY3 and NSC 99-2314-B-166-001-MY3). We also gratefully acknowledge the Second Core Laboratory of Department of Medical Research, National Taiwan University Hospital for expert technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by A Finazzi-Agró
Supplementary Information accompanies the paper on Cell Death and Differentiation website
Supplementary information
Rights and permissions
About this article
Cite this article
Lin, CL., Tseng, HC., Chen, WP. et al. Intracellular zinc release-activated ERK-dependent GSK-3β–p53 and Noxa–Mcl-1 signaling are both involved in cardiac ischemic-reperfusion injury. Cell Death Differ 18, 1651–1663 (2011). https://doi.org/10.1038/cdd.2011.80
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cdd.2011.80
Keywords
This article is cited by
-
The Role of P53 in Myocardial Ischemia-Reperfusion Injury
Cardiovascular Drugs and Therapy (2023)
-
The Role of ERK1/2 Pathway in the Pathophysiology of Alzheimer’s Disease: An Overview and Update on New Developments
Cellular and Molecular Neurobiology (2023)
-
Autophagy-mediated expression clusters are involved in immunity regulation of coronary artery disease
BMC Genomic Data (2022)
-
Comparative Response of Cardiomyocyte ZIPs and ZnTs to Extracellular Zinc and TPEN
Biological Trace Element Research (2019)
-
Zinc Dyshomeostasis in Cardiomyocytes after Acute Hypoxia/Reoxygenation
Biological Trace Element Research (2017)