Abstract
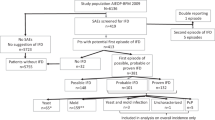
Invasive aspergillosis (IA) has been reported to yield high mortality rates. Patients with an unfavourable prognostic haematological disease not only have a higher probability of developing IA but are also more likely to die due to causes directly related to the underlying disease. This complexity of risk mechanisms confounds the causal interpretation of IA occurrence and mortality. Full consideration of the changing patient characteristics over time is necessary to obtain reliable estimates of the correlation of IA with mortality. We studied the effect of IA on mortality in 167 consecutive patients starting with remission–induction therapy for AML or of whom most patients continued to haematopoietic stem cell transplantation (HSCT). No standard antifungal prophylaxis was administered in the period before HSCT. Survival analyses were performed to determine risk estimates of IA for different phases of treatment before and after HSCT. Time-dependent adjustment for confounding variables was performed using Cox proportional hazards models. In 55 of 167 enroled patients, IA was diagnosed. Before HSCT, adjusted hazard ratios and 95% confidence intervals on mortality after the diagnosis of IA were 3.5 (1.7–7.5), 2.0 (0.69–5.9), 2.3 (0.79–6.8) and 0.80 (0.49–1.4) within 30 days, between 30 and 60 days, between 60 and 90 days or more than 90 days, respectively. A similar pattern was observed after HSCT. The occurrence of IA did not significantly influence the decision to follow through with HSCT. The results provide new insights in short- and long-term survival of patients diagnosed with IA. A significantly increased mortality risk was only observed in the first month after diagnosis of IA. No unfavourable association with mortality was observed in the later course of treatment. The occurrence of IA did not affect the probability of attaining HSCT in our population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Bower H, Andersson TM, Bjorkholm M, Dickman PW, Lambert PC, Derolf AR . Continued improvement in survival of acute myeloid leukemia patients: an application of the loss in expectation of life. Blood Cancer J 2016; 6: e390.
Shah BK, Ghimire KB . Improved survival among older acute myeloid leukemia patients-a population-based study. Acta Oncol 2014; 53: 935–938.
Auberger J, Lass-Florl C, Ulmer H, Nogler-Semenitz E, Clausen J, Gunsilius E et al. Significant alterations in the epidemiology and treatment outcome of invasive fungal infections in patients with hematological malignancies. Int J Hematol 2008; 88: 508–515.
Lin SJ, Schranz J, Teutsch SM . Aspergillosis case-fatality rate: systematic review of the literature. Clin Infect Dis 2001; 32: 358–366.
Mirkov I, Stosic-Grujicic S, Kataranovski M . Host immune defense against Aspergillus fumigatus: insight from experimental systemic (disseminated) infection. Immunol Res 2012; 52: 120–126.
Tokarski C, Hummert S, Mech F, Figge MT, Germerodt S, Schroeter A et al. Agent-based modeling approach of immune defense against spores of opportunistic human pathogenic fungi. Front Microbiol 2012; 3: 129.
Baddley JW . Clinical risk factors for invasive aspergillosis. Med Mycol 2011; 49 (Suppl 1): S7–S12.
Caira M, Mancinelli M, Leone G, Pagano L . Invasive aspergillosis in acute leukemias: old and new risk factors and epidemiological trends. Med Mycol 2011; 49 (Suppl 1): S13–S16.
van de Peppel RJ, Dekkers OM, von dem Borne PA, de Boer MG . Relapsed and secondary disease drive the risk profile for invasive aspergillosis prior to stem cell transplantation in patients with acute myeloid leukemia or myelodysplastic syndrome. Med Mycol 2014; 52: 699–705.
Meijer E, Cornelissen JJ . Allogeneic stem cell transplantation in acute myeloid leukemia in first or subsequent remission: weighing prognostic markers predicting relapse and risk factors for non-relapse mortality. Semin Oncol 2008; 35: 449–457.
Tawfik B, Pardee TS, Isom S, Sliesoraitis S, Winter A, Lawrence J et al. Comorbidity, age, and mortality among adults treated intensively for acute myeloid leukemia (AML). J Geriatr Oncol 2016; 7: 24–31.
Tsimberidou AM, Estey E . Induction mortality risk in adult acute myeloid leukemia. Leuk Lymphoma 2006; 47: 1199–1200.
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 2008; 46: 1813–1821.
VanderWeele TJ, Hernan MA, Robins JM . Causal directed acyclic graphs and the direction of unmeasured confounding bias. Epidemiology 2008; 19: 720–728.
Burghi G, Lemiale V, Seguin A, Lambert J, Lacroix C, Canet E et al. Outcomes of mechanically ventilated hematology patients with invasive pulmonary aspergillosis. Intensive Care Med 2011; 37: 1605–1612.
Gregg KS, Kauffman CA . Invasive aspergillosis: epidemiology, clinical aspects, and treatment. Semin Respir Crit Care Med 2015; 36: 662–672.
Garcia-Vidal C, Peghin M, Cervera C, Gudiol C, Ruiz-Camps I, Moreno A et al. Causes of death in a contemporary cohort of patients with invasive aspergillosis. PLoS ONE 2015; 10: e0120370.
Kurosawa M, Yonezumi M, Hashino S, Tanaka J, Nishio M, Kaneda M et al. Epidemiology and treatment outcome of invasive fungal infections in patients with hematological malignancies. Int J Hematol 2012; 96: 748–757.
Lee JY, Jung CW, Kim K, Jang JH . Impact of previous invasive pulmonary aspergillosis on the outcome of allogeneic hematopoietic stem cell transplantation. Korean J Hematol 2012; 47: 255–259.
Michallet M, Benet T, Sobh M, Kraghel S, El Hamri M, Cannas G et al. Invasive aspergillosis: an important risk factor on the short- and long-term survival of acute myeloid leukemia (AML) patients. Eur J Clin Microbiol Infect Dis 2012; 31: 991–997.
Salmeron G, Porcher R, Bergeron A, Robin M, Peffault de Latour R, Ferry C et al. Persistent poor long-term prognosis of allogeneic hematopoietic stem cell transplant recipients surviving invasive aspergillosis. Haematologica 2012; 97: 1357–1363.
Girmenia C, Micozzi A, Piciocchi A, Gentile G, Di Caprio L, Nasso D et al. Invasive fungal diseases during first induction chemotherapy affect complete remission achievement and long-term survival of patients with acute myeloid leukemia. Leuk Res 2014; 38: 469–474.
Li L, Wang J, Zhang W, Yang J, Chen L, Lv S . Risk factors for invasive mold infections following allogeneic hematopoietic stem cell transplantation: a single center study of 190 recipients. Scand J Infect Dis 2012; 44: 100–107.
Mikulska M, Raiola AM, Bruno B, Furfaro E, Van Lint MT, Bregante S et al. Risk factors for invasive aspergillosis and related mortality in recipients of allogeneic SCT from alternative donors: an analysis of 306 patients. Bone Marrow Transplant 2009; 44: 361–370.
Hardak E, Avivi I, Berkun L, Raz-Pasteur A, Lavi N, Geffen Y et al. Polymicrobial pulmonary infection in patients with hematological malignancies: prevalence, co-pathogens, course and outcome. Infection 2016; 44: 491–497.
Kikuchi M, Nakasone H, Mitani K, Gotoh M, Kobayashi A, Kurita N et al. Retrospective assessment of secondary prophylaxis for invasive aspergillosis in neutropenic hematology patients and identification of risk factors for relapse of fungal disease. Scand J Infect Dis 2013; 45: 531–536.
Basara N, Schulze A, Wedding U, Mohren M, Gerhardt A, Junghanss C et al. Early related or unrelated haematopoietic cell transplantation results in higher overall survival and leukaemia-free survival compared with conventional chemotherapy in high-risk acute myeloid leukaemia patients in first complete remission. Leukemia 2009; 23: 635–640.
Jourdan E, Maraninchi D, Reiffers J, Gluckman E, Rio B, Jouet JP et al. Early allogeneic transplantation favorably influences the outcome of adult patients suffering from acute myeloid leukemia. Societe Francaise de Greffe de Moelle (SFGM). Bone Marrow Transplant 1997; 19: 875–881.
Busca A, Tortorano AM, Pagano L . Reviewing the importance and evolution of fungal infections and potential antifungal resistance in haematological patients. J Glob Antimicrob Resist 2015; 3: 237–241.
Herbrecht R, Patterson TF, Slavin MA, Marchetti O, Maertens J, Johnson EM et al. Application of the 2008 definitions for invasive fungal diseases to the trial comparing voriconazole versus amphotericin B for therapy of invasive aspergillosis: a collaborative study of the Mycoses Study Group (MSG 05) and the European Organization for Research and Treatment of Cancer Infectious Diseases Group. Clin Infect Dis 2015; 60: 713–720.
Acknowledgements
We thank Professor Dr LG Visser for reading and critical appraisal of the pre-final version of the manuscript.
Author contributions
RP and MB initiated the study and were involved in the design. RP and PB contributed to the data collection. SC contributed to the study design and statistical analysis. All authors were actively involved in manuscript preparation and have read and approved the final manuscript.
The study, in preliminary form, was presented at the Trends in Medical Mycology Congress in Lisbon, Portugal, October 2015 (abstract number P290), and awarded with a ‘Young Investigator Award’ for author RJ van de Peppel.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
van de Peppel, R., von dem Borne, P., le Cessie, S. et al. A new time-dependent approach for assessment of the impact of invasive aspergillosis shows effect on short- but not on long-term survival of patients with AML or high-risk MDS. Bone Marrow Transplant 52, 883–888 (2017). https://doi.org/10.1038/bmt.2017.71
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2017.71