Abstract
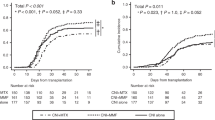
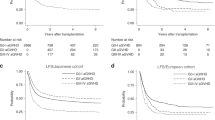
To investigate better GVHD prophylaxis in reduced intensity conditioning umbilical cord blood transplantation (RIC-UCBT), we compared transplant outcomes after UCBT among GvHD prophylaxes using the registry data. We selected patients transplanted for AML or ALL with a calcineurin inhibitor and methotrexate (MTX)/mycophenolate mofetil (MMF) combination. A total of 748 first RIC-UCBT between 2000 and 2012 (MTX+ group, 446, MMF+ group, 302) were included. The cumulative incidence of neutrophil and platelet counts higher than 50 000/μL was significantly better in the MMF+ group (relative risk (RR), 1.55; P<0.001: RR, 1.34; P=0.003, respectively). In multivariate analyses, the risk of grade II–IV and III–IV acute GvHD was significantly higher in the MMF+ group than in the MTX+ group (RR, 1.75; P<0.001: RR, 1.97; P=0.004, respectively). In disease-specific analyses of AML, the risk of relapse of high-risk disease was significantly lower in the MMF+ group (RR, 0.69; P=0.009), whereas no significant difference was observed in the risk of relapse-free and overall survival in high-risk disease. In patients with standard-risk disease, no significant differences were noted in the risk of relapse or survival between the MTX+ and MMF+ groups. Collectively, these results suggest that MMF-containing prophylaxis may be preferable in RIC-UCBT, particularly for high-risk disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Rocha V, Labopin M, Sanz G, Arcese W, Schwerdtfeger R, Bosi A et al. Transplants of umbilical-cord blood or bone marrow from unrelated donors in adults with acute leukemia. N Engl J Med 2004; 351: 2276–2285.
Laughlin MJ, Eapen M, Rubinstein P, Wagner JE, Zhang MJ, Champlin RE et al. Outcomes after transplantation of cord blood or bone marrow from unrelated donors in adults with leukemia. N Engl J Med 2004; 351: 2265–2275.
Ooi J . Cord blood transplantation in adults. Bone Marrow Transplant 2009; 44: 661–666.
Ballen KK, Gluckman E, Broxmeyer HE . Umbilical cord blood transplantation: the first 25 years and beyond. Blood 2013; 122: 491–498.
Takahashi S, Iseki T, Ooi J, Tomonari A, Takasugi K, Shimohakamada Y et al. Single-institute comparative analysis of unrelated bone marrow transplantation and cord blood transplantation for adult patients with hematologic malignancies. Blood 2004; 104: 3813–3820.
Eapen M, Rocha V, Sanz G, Scaradavou A, Zhang MJ, Arcese W et al. Effect of graft source on unrelated donor haemopoietic stem-cell transplantation in adults with acute leukaemia: a retrospective analysis. Lancet Oncol 2010; 11: 653–660.
Tanaka M, Miyamura K, Terakura S, Imai K, Uchida N, Ago H et al. Comparison of cord blood transplantation with unrelated bone marrow transplantation in patients older than fifty years. Biol Blood Marrow Transplant 2015; 21: 517–525.
Majhail NS, Brunstein CG, Shanley R, Sandhu K, McClune B, Oran B et al. Reduced-intensity hematopoietic cell transplantation in older patients with AML/MDS: umbilical cord blood is a feasible option for patients without HLA-matched sibling donors. Bone Marrow Transplant 2012; 47: 494–498.
Pascal L, Tucunduva L, Ruggeri A, Blaise D, Ceballos P, Chevallier P et al. Impact of ATG-containing reduced-intensity conditioning after single- or double-unit allogeneic cord blood transplantation. Blood 2015; 126: 1027–1032.
Mohty M, Gaugler B . Advances in umbilical cord transplantation: the role of thymoglobulin/ATG in cord blood transplantation. Best Pract Res Clin Haematol 2010; 23: 275–282.
Pascal L, Mohty M, Ruggeri A, Tucunduva L, Milpied N, Chevallier P et al. Impact of rabbit ATG-containing myeloablative conditioning regimens on the outcome of patients undergoing unrelated single-unit cord blood transplantation for hematological malignancies. Bone Marrow Transplant 2015; 50: 45–50.
Lindemans CA, Chiesa R, Amrolia PJ, Rao K, Nikolajeva O, de Wildt A et al. Impact of thymoglobulin prior to pediatric unrelated umbilical cord blood transplantation on immune reconstitution and clinical outcome. Blood 2014; 123: 126–132.
Admiraal R, van Kesteren C, Jol-van der Zijde CM, Lankester AC, Bierings MB, Egberts TC et al. Association between anti-thymocyte globulin exposure and CD4+ immune reconstitution in paediatric haemopoietic cell transplantation: a multicentre, retrospective pharmacodynamic cohort analysis. Lancet Haematol 2015; 2: e194–e203.
Admiraal R, Lindemans CA, van Kesteren C, Bierings MB, Versluys AB, Nierkens S et al. Excellent T-cell reconstitution and survival provided ATG exposure is low or absent after pediatric cord blood transplantation. Blood 2016; 128: 2734–2741.
Sakai R, Taguri M, Oshima K, Mori T, Ago H, Adachi S et al. A comparison of tacrolimus and cyclosporine combined with methotrexate for graft-versus-host disease prophylaxis, stratified by stem cell source: a retrospective nationwide survey. Int J Hematol 2016; 103: 322–333.
Terakura S, Atsuta Y, Tsukada N, Kobayashi T, Tanaka M, Kanda J et al. Comparison of outcomes of 8/8 and 7/8 allele-matched unrelated bone marrow transplantation and single-unit cord blood transplantation in adults with acute leukemia. Biol Blood Marrow Transplant 2016; 22: 330–338.
Barker JN, Davies SM, DeFor T, Ramsay NK, Weisdorf DJ, Wagner JE . Survival after transplantation of unrelated donor umbilical cord blood is comparable to that of human leukocyte antigen-matched unrelated donor bone marrow: results of a matched-pair analysis. Blood 2001; 97: 2957–2961.
Miyakoshi S, Yuji K, Kami M, Kusumi E, Kishi Y, Kobayashi K et al. Successful engraftment after reduced-intensity umbilical cord blood transplantation for adult patients with advanced hematological diseases. Clin Cancer Res 2004; 10: 3586–3592.
Kishi Y, Kami M, Miyakoshi S, Kanda Y, Murashige N, Teshima T et al. Early immune reaction after reduced-intensity cord-blood transplantation for adult patients. Transplantation 2005; 80: 34–40.
Uchida N, Wake A, Nakano N, Ishiwata K, Takagi S, Tsuji M et al. Mycophenolate and tacrolimus for graft-versus-host disease prophylaxis for elderly after cord blood transplantation: a matched pair comparison with tacrolimus alone. Transplantation 2011; 92: 366–371.
Narimatsu H, Terakura S, Matsuo K, Oba T, Uchida T, Iida H et al. Short-term methotrexate could reduce early immune reactions and improve outcomes in umbilical cord blood transplantation for adults. Bone Marrow Transplant 2007; 39: 31–39.
Murata M . Prophylactic and therapeutic treatment of graft-versus-host disease in Japan. Int J Hematol 2015; 101: 467–486.
Kanda J, Atsuta Y, Wake A, Ichinohe T, Takanashi M, Morishima Y et al. Impact of the direction of HLA mismatch on transplantation outcomes in single unrelated cord blood transplantation. Biol Blood Marrow Transplant 2013; 19: 247–254.
Atsuta Y . Introduction of Transplant Registry Unified Management Program 2 (TRUMP2): scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int J Hematol 2016; 103: 3–10.
Atsuta Y, Suzuki R, Yoshimi A, Gondo H, Tanaka J, Hiraoka A et al. Unification of hematopoietic stem cell transplantation registries in Japan and establishment of the TRUMP System. Int J Hematol 2007; 86: 269–274.
Kanda J . Scripts for TRUMP data analyses. Part II (HLA-related data): statistical analyses specific for hematopoietic stem cell transplantation. Int J Hematol 2016; 103: 11–19.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant 2009; 15: 1628–1633.
Schoemans H, Theunissen K, Maertens J, Boogaerts M, Verfaillie C, Wagner J . Adult umbilical cord blood transplantation: a comprehensive review. Bone Marrow Transplant 2006; 38: 83–93.
Przepiorka D, Weisdorf D, Martin P, Klingemann H, Beatty P, Hows J et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transplant 1995; 15: 825–828.
Lee SJ, Vogelsang G . Flowers MED. Chronic graft-versus-host disease. Biol Blood Marrow Transplant 2003; 9: 215–233.
Kaplan E, Meier P . Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–481.
Gooley TA, Leisenring W, Crowley J, Storer BE . Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 1999; 18: 695–706.
Cox DR . Regression models and life-tables. J R Stat Soc Series B 1972; 34: 187–220.
Fine JP, Gray RJ . A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94: 496–509.
Kanda Y . Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant 2013; 48: 452–458.
Ogata M, Fukuda T, Teshima T . Human herpesvirus-6 encephalitis after allogeneic hematopoietic cell transplantation: what we do and do not know. Bone Marrow Transplant 2015; 50: 1030–1036.
Terakura S, Wake A, Inamoto Y, Murata M, Sakai R, Yamaguchi T et al. Exploratory research for optimal GvHD prophylaxis after single unit CBT in adults: short-term methotrexate reduced the incidence of severe GvHD more than mycophenolate mofetil. Bone Marrow Transplant 2017; 52: 423–430.
Koyama M, Hashimoto D, Nagafuji K, Eto T, Ohno Y, Aoyama K et al. Expansion of donor-reactive host T cells in primary graft failure after allogeneic hematopoietic SCT following reduced-intensity conditioning. Bone Marrow Transplant 2014; 49: 110–115.
Martin P . Donor CD8 cells prevent allogeneic marrow graft rejection in mice: potential implications for marrow transplantation in humans. J Exp Med 1993; 178: 703–712.
Moscardo F, Sanz J, Carbonell F, Sanz MA, Larrea L, Montesinos P et al. Effect of CD8 cell content on umbilical cord blood transplantation in adults with hematological malignancies. Biol Blood Marrow Transplant 2014; 20: 1744–1750.
Terakura S, Azuma E, Murata M, Kumamoto T, Hirayama M, Atsuta Y et al. Hematopoietic engraftment in recipients of unrelated donor umbilical cord blood is affected by the CD34+ and CD8+ cell doses. Biol Blood Marrow Transplant 2007; 13: 822–830.
Vogelsang GB, Arai S . Mycophenolate mofetil for the prevention and treatment of graft-versus-host disease following stem cell transplantation: preliminary findings. Bone Marrow Transplant 2001; 27: 1255–1262.
Storb R, Yu C, Wagner JL, Deeg HJ, Nash RA, Kiem H-P et al. Stable Mixed hematopoietic chimerism in DLA-identical littermate dogs given sublethal total body irradiation before and pharmacological immunosuppression after marrow transplantation. Blood 1997; 89: 3048–3054.
Teshima T, Reddy P, Zeiser R . Acute graft-versus-host disease: novel biological insights. Biol Blood Marrow Transplant 2016; 22: 11–16.
Kanda J, Morishima Y, Terakura S, Wake A, Uchida N, Takahashi S et al. Impact of graft-versus-host disease on outcomes after unrelated cord blood transplantation. Leukemia 2017; 31: 663–668.
Horowitz MM, Gale RP, Sondel PM, Goldman JM, Kersey J, Kolb HJ et al. Graft-versus-leukemia reactions after bone marrow transplantation. Blood 1990; 75: 555–562.
Storb R, Gyurkocza B, Storer BE, Sorror ML, Blume K, Niederwieser D et al. Graft-versus-host disease and graft-versus-tumor effects after allogeneic hematopoietic cell transplantation. J Clin Oncol 2013; 31: 1530–1538.
Acknowledgements
We thank all the physicians and data managers at the institutes that contributed the valuable data on transplantation to the JSHCT and all the members of the data management committees of the JSHCT. This study was supported in part by a Grant-in-Aid for Scientific Research (KAKENHI 15K09497 to ST) from the Japan Society for the Promotion of Science (JSPS).
Author contributions
ST designed the research, analyzed the data, and wrote the manuscript. YKu, SY, AW, JK, YI and TY analyzed the data and helped write the manuscript. SMiz, NU, YKo, NA, HO, HK, YN, SMiy, MO, and IA collected the patient data. TF, TI and YA supervised the data management. MM and TT designed and supervised the research. All authors reviewed and approved the final version of the manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Bone Marrow Transplantation website
Rights and permissions
About this article
Cite this article
Terakura, S., Kuwatsuka, Y., Yamasaki, S. et al. GvHD prophylaxis after single-unit reduced intensity conditioning cord blood transplantation in adults with acute leukemia. Bone Marrow Transplant 52, 1261–1267 (2017). https://doi.org/10.1038/bmt.2017.116
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2017.116
This article is cited by
-
Safety of romiplostim administered immediately after cord-blood transplantation: a phase 1 trial
Annals of Hematology (2023)
-
Impact of donor types on reduced-intensity conditioning allogeneic stem cell transplant for mature lymphoid malignancies
Bone Marrow Transplantation (2022)
-
Improved outcomes of single-unit cord blood transplantation for acute myeloid leukemia by killer immunoglobulin-like receptor 2DL1-ligand mismatch
Bone Marrow Transplantation (2022)
-
Improved survival after single-unit cord blood transplantation using fludarabine and melphalan-based reduced-intensity conditioning for malignant lymphoma: impact of melphalan dose and graft-versus-host disease prophylaxis with mycophenolate mofetil
Annals of Hematology (2022)
-
Comparison of immunosuppressant regimens in salvage cord blood transplantation for graft failure after allogeneic hematopoietic stem cell transplantation
Bone Marrow Transplantation (2021)