Abstract
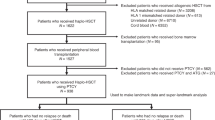
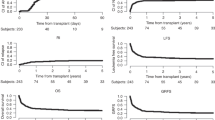
Relapse remains a major cause of mortality among patients receiving allogeneic hematopoietic cell transplantation (HCT). The impact of donor type on post-relapse survival (PRS) has not been widely examined. We compared the survival outcomes for patients relapsing after haploidentical donor transplantation (HIDT) using post-transplant cyclophosphamide with those relapsing after matched-related donor transplantation (MRDT) or matched-unrelated donor transplantation (MUDT) at our institution. Two hundred and thirty-seven consecutive HCT recipients with relapse occurring after HIDT (N=48), MUDT (N=87) and MRDT (N=102) were included in this analysis. Median age was 49 years (19–77 years) and the median time to relapse was 156 days (12–2465) after HCT. HIDT recipients had similar median time to relapse (5.8 vs 4.8 vs 5.5 months, P=0.638) compared with MUDT and MRDT, respectively. One-year PRS was worse among HIDT recipients compared with MRDT and MUDT (17% vs 46% vs 40%, P<0.05). In a multivariate analysis, time to relapse (<3 vs >3 months post transplant), no use of donor lymphocyte infusion (DLI) following relapse, higher Dana Farber disease risk index and HCT comorbidity index scores at the time of transplant and delayed platelet engraftment post transplant were all predictive of worse PRS. This analysis shows that 1-year PRS is inferior among HIDT when compared with MRDT or MUDT. Lower use of DLI after HIDT may have contributed to this inferior survival.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Szydlo R, Goldman JM, Klein JP, Gale RP, Ash RC, Bach FH et al. Results of allogeneic bone marrow transplants for leukemia using donors other than HLA-identical siblings. J Clin Oncol 1997; 15: 1767–1777.
Bashey A, Zhang X, Sizemore CA, Manion K, Brown S, Holland HK et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol 2013; 31: 1310–1316.
Brunstein CG, Fuchs EJ, Carter SL, Karanes C, Costa LJ, Wu J et al. Alternative donor transplantation after reduced intensity conditioning: results of parallel phase 2 trials using partially HLA-mismatched related bone marrow or unrelated double umbilical cord blood grafts. Blood 2011; 118: 282–288.
Luznik L, O'Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant 2008; 14: 641–650.
McCurdy SR, Kanakry JA, Showel MM, Tsai HL, Bolanos-Meade J, Rosner GL et al. Risk-stratified outcomes of nonmyeloablative HLA-haploidentical BMT with high-dose posttransplantation cyclophosphamide. Blood 2015; 125: 3024–3031.
Raiola AM, Dominietto A, di Grazia C, Lamparelli T, Gualandi F, Ibatici A et al. Unmanipulated haploidentical transplants compared with other alternative donors and matched sibling grafts. Biol Blood Marrow Transplant 2014; 20: 1573–1579.
Barrett AJ, Battiwalla M . Relapse after allogeneic stem cell transplantation. Expert Rev Hematol 2010; 3: 429–441.
Bejanyan N, Weisdorf DJ, Logan BR, Wang HL, Devine SM, de Lima M et al. Survival of patients with acute myeloid leukemia relapsing after allogeneic hematopoietic cell transplantation: a center for international blood and marrow transplant research study. Biol Blood Marrow Transplant 2015; 21: 454–459.
Schmid C, Labopin M, Nagler A, Bornhauser M, Finke J, Fassas A et al. Donor lymphocyte infusion in the treatment of first hematological relapse after allogeneic stem-cell transplantation in adults with acute myeloid leukemia: a retrospective risk factors analysis and comparison with other strategies by the EBMT Acute Leukemia Working Party. J Clin Oncol 2007; 25: 4938–4945.
Thanarajasingam G, Kim HT, Cutler C, Ho VT, Koreth J, Alyea EP et al. Outcome and prognostic factors for patients who relapse after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2013; 19: 1713–1718.
Bejanyan N, Oran B, Shanley R, Warlick E, Ustun C, Vercellotti G et al. Clinical outcomes of AML patients relapsing after matched-related donor and umbilical cord blood transplantation. Bone Marrow Transplant 2014; 49: 1029–1035.
Zeidan AM, Forde PM, Symons H, Chen A, Smith BD, Pratz K et al. HLA-haploidentical donor lymphocyte infusions for patients with relapsed hematologic malignancies after related HLA-haploidentical bone marrow transplantation. Biol Blood Marrow Transplant 2014; 20: 314–318.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transplant 2009; 15: 367–369.
Luger SM, Ringden O, Zhang MJ, Perez WS, Bishop MR, Bornhauser M et al. Similar outcomes using myeloablative vs reduced-intensity allogeneic transplant preparative regimens for AML or MDS. Bone Marrow Transplant 2012; 47: 203–211.
Solomon SR, Sizemore CA, Sanacore M, Zhang X, Brown S, Holland HK et al. Haploidentical transplantation using T cell replete peripheral blood stem cells and myeloablative conditioning in patients with high-risk hematologic malignancies who lack conventional donors is well tolerated and produces excellent relapse-free survival: Results of a Prospective Phase II Trial. Biol Blood Marrow Transplant 2012; 18: 1859–1866.
Solomon SR, Sizemore CA, Sanacore M, Zhang X, Brown S, Holland HK et al. Total body irradiation-based myeloablative haploidentical stem cell transplantation is a safe and effective alternative to unrelated donor transplantation in patients without matched sibling donors. Biol Blood Marrow Transplant 2015; 21: 1299–1307.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 2005; 106: 2912–2919.
Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME et al. Validation and refinement of the Disease Risk Index for allogeneic stem cell transplantation. Blood 2014; 123: 3664–3671.
Bashey A, Zhang X, Jackson K, Brown S, Ridgeway M, Solh M et al. Comparison of outcomes of hematopoietic cell transplants from t-replete haploidentical donors using post-transplantation cyclophosphamide with 10 of 10 HLA-A, -B, -C, -DRB1, and -DQB1 allele-matched unrelated donors and HLA-identical sibling donors: a multivariable analysis including disease risk index. Biol Blood Marrow Transplant 2015; 22: 125–133.
de Lima M, Giralt S, Thall PF, de Padua Silva L, Jones RB, Komanduri K et al. Maintenance therapy with low-dose azacitidine after allogeneic hematopoietic stem cell transplantation for recurrent acute myelogenous leukemia or myelodysplastic syndrome: a dose and schedule finding study. Cancer 2010; 116: 5420–5431.
Lewalle P, Triffet A, Delforge A, Crombez P, Selleslag D, De Muynck H et al. Donor lymphocyte infusions in adult haploidentical transplant: a dose finding study. Bone Marrow Transplant 2003; 31: 39–44.
Ghiso A, Raiola AM, Gualandi F, Dominietto A, Varaldo R, Van Lint MT et al. DLI after haploidentical BMT with post-transplant CY. Bone Marrow Transplant 2015; 50: 56–61.
Chang YJ, Huang XJ . Donor lymphocyte infusions for relapse after allogeneic transplantation: when, if and for whom? Blood Rev 2013; 27: 55–62.
Vago L, Perna SK, Zanussi M, Mazzi B, Barlassina C, Stanghellini MT et al. Loss of mismatched HLA in leukemia after stem-cell transplantation. N Engl J Med 2009; 361: 478–488.
Bolanos-Meade J, Smith BD, Gore SD, McDevitt MA, Luznik L, Fuchs EJ et al. 5-Azacytidine as salvage treatment in relapsed myeloid tumors after allogeneic bone marrow transplantation. Biol Blood Marrow Transplant 2011; 17: 754–758.
Sharma M, Ravandi F, Bayraktar UD, Chiattone A, Bashir Q, Giralt S et al. Treatment of FLT3-ITD-positive acute myeloid leukemia relapsing after allogeneic stem cell transplantation with sorafenib. Biol Blood Marrow Transplant 2011; 17: 1874–1877.
Tischer J, Engel N, Fritsch S, Prevalsek D, Hubmann M, Schulz C et al. Second haematopoietic SCT using HLA-haploidentical donors in patients with relapse of acute leukaemia after a first allogeneic transplantation. Bone Marrow Transplant 2014; 49: 895–901.
Solh MCK, Zhang X, Brown S, Morris L, Holland K, Solomon SR et al. T cell replete HLA-haploidentical donor transplantation (HIDT) with post-transplant cyclophosphamide (pTcy) is an effective salvage for patients relapsing after a matched sibling or a matched unrelated donor transplantation. Blood 2015; 126: 23.
de Lima M, Porter DL, Battiwalla M, Bishop MR, Giralt SA, Hardy NM et al. Proceedings from the National Cancer Institute's Second International Workshop on the Biology, Prevention, and Treatment of Relapse After Hematopoietic Stem Cell Transplantation: part III. Prevention and treatment of relapse after allogeneic transplantation. Biol Blood Marrow Transplant 2014; 20: 4–13.
Scott BPM, Logan B, Wu J, Devine S, Porter D, Maziarz R et al. Results of a phase III randomized, multi-center study of allogeneic stem cell transplantation after high vs reduced intensity conditioning in patients with myelodysplastic syndrome (MDS) or acute myeloid leukemia (AML): Blood and Marrow Transplant Clinical Trials Network (BMT CTN) 0901. Blood 2015; 126: 23.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Solh, M., Zhang, X., Connor, K. et al. Post-relapse survival after haploidentical transplantation vs matched-related or matched-unrelated hematopoietic cell transplantation. Bone Marrow Transplant 51, 949–954 (2016). https://doi.org/10.1038/bmt.2016.62
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.62
This article is cited by
-
Prognosis and risk factors for central nervous system relapse after allogeneic hematopoietic stem cell transplantation in acute myeloid leukemia
Annals of Hematology (2021)
-
Leukemia relapse following unmanipulated haploidentical transplantation: a risk factor analysis on behalf of the ALWP of the EBMT
Journal of Hematology & Oncology (2019)
-
Assessing the efficacy of an ambulatory peripheral blood hematopoietic stem cell transplant program using reduced intensity conditioning in a low-middle-income country
Bone Marrow Transplantation (2019)
-
Comparison of outcomes following transplantation with T-replete HLA-haploidentical donors using post-transplant cyclophosphamide to matched related and unrelated donors for patients with AML and MDS aged 60 years or older
Bone Marrow Transplantation (2018)
-
Comparable post-relapse outcomes between haploidentical and matched related donor allogeneic stem cell transplantation
Bone Marrow Transplantation (2017)