Abstract
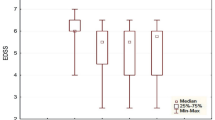
Although allogeneic hematopoietic stem cell transplantation (HSCT) features severe physical and psychological strain, no previous study has prospectively investigated fatigue beyond 3 years after transplantation. We investigated the temporal course of fatigue over 5 years, compared patients with the general population (GP) and tested for treatment- and complication-related risk factors. Patients were assessed before conditioning (T0, N=239) and at 100-day (T1, N=150), 1-year (T2, N=102) and 5-year (T3, N=45) follow-up. We measured fatigue with the Multidimensional Fatigue Inventory-20. Patients were compared with the GP at T0 and at T3. Global fatigue increased from T0 to T1 (t=3.85, P<0.001), decreased from T1 to T2 (t=−2. 92, P=0.004) and then remained stable (t=0.45, P=0.656). No difference in global fatigue was found between T0 and T3 (t=0.68, P=0.497). Compared with the GP, patients showed higher global fatigue at T0 (t=−6.02, P<0.001) and T3 (t=−2.50, P=0.014). These differences reached meaningful effect sizes (d⩾0.5). Acute and chronic GvHD predicted global fatigue at T1 (γ=0.34, P=0.006) and T2 (γ=0.38, P=0.010), respectively. To conclude, fatigue among allogeneic HSCT patients improves with time, finally returning to pretransplantation levels. However, even after 5 years, the difference from the GP remains relevant. Patients with GvHD are at risk for increased fatigue.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Mosher CE, Redd WH, Rini CM, Burkhalter JE, DuHamel KN . Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: a review of the literature. Psychooncology 2009; 18: 113–127.
Müller LP, Müller-Tidow C . The indications for allogeneic stem cell transplantation in myeloid malignancies. Dtsch Arztebl Int 2015; 112: 262–270.
Jacobsohn DA, Vogelsang GB . Acute graft versus host disease. Orphanet J Rare Dis 2007; 2: 35.
Copelan EA . Hematopoietic stem-cell transplantation. N Engl J Med 2006; 354: 1813–1826.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Cancer-Related Fatigue, 2015. Fort Washington, PA, USA, 2015. www.nccn.org.
Grulke N, Albani C, Bailer H . Quality of life in patients before and after haematopoietic stem cell transplantation measured with the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Core Questionnaire QLQ-C30. Bone Marrow Transplant 2012; 47: 473–482.
Anderson KO, Giralt SA, Mendoza TR, Brown JO, Neumann JL, Mobley GM et al. Symptom burden in patients undergoing autologous stem-cell transplantation. Bone Marrow Transplant 2007; 39: 759–766.
Carlson LE, Koski T, Glück S . Longitudinal effects of high-dose chemotherapy and autologous stem cell transplantation on quality of life in the treatment of metastatic breast cancer. Bone Marrow Transplant 2001; 27: 989–998.
Hacker ED, Ferrans C, Verlen E, Ravandi F, van Besien K, Gelms J et al. Fatigue and physical activity in patients undergoing hematopoietic stem cell transplant. Oncol Nurs Forum 2006; 33: 614–624.
El-Banna MM, Berger AM, Farr L, Foxall MJ, Friesth B, Schreiner E . Fatigue and depression in patients with lymphoma undergoing autologous peripheral blood stem cell transplantation. Oncol Nurs Forum 2004; 31: 937–944.
Lee SJ, Fairclough D, Parsons SK, Soiffer RJ, Fisher DC, Schlossman RL et al. Recovery after stem-cell transplantation for hematologic diseases. J Clin Oncol 2001; 19: 242–252.
Conner-Spady BL, Cumming C, Nabholtz J, Jacobs P, Stewart D . A longitudinal prospective study of health-related quality of life in breast cancer patients following high-dose chemotherapy with autologous blood stem cell transplantation. Bone Marrow Transplant 2005; 36: 251–259.
Hjermstad MJ, Knobel H, Brinch L, Fayers PM, Loge JH, Holte H et al. A prospective study of health-related quality of life, fatigue, anxiety and depression 3-5 years after stem cell transplantation. Bone Marrow Transplant 2004; 34: 257–266.
Worel N, Biener D, Kalhs P, Mitterbauer M, Keil F, Schulenburg A et al. Quality of life: Long-term outcome and quality of life of patients who are alive and in complete remission more than two years after allogeneic and syngeneic stem cell transplantation. Bone Marrow Transplant 2002; 30: 619–626.
Schulz-Kindermann F, Mehnert A, Scherwath A, Schirmer L, Schleimer B, Zander AR et al. Cognitive function in the acute course of allogeneic hematopoietic stem cell transplantation for hematological malignancies. Bone Marrow Transplant 2007; 39: 789–799.
Syrjala KL, Langer SL, Abrams JR, Storer BE, Martin PJ . Late effects of hematopoietic cell transplantation among 10-year adult survivors compared with case-matched controls. J Clin Oncol 2005; 23: 6596–6606.
Andrykowski MA, Bishop MM, Hahn EA, Cella DF, Beaumont JL, Brady MJ et al. Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. J Clin Oncol 2005; 23: 599–608.
Kopp M, Holzner B, Meraner V, Sperner‐Unterweger B, Kemmler G, Nguyen‐Van‐Tam DP et al. Quality of life in adult hematopoietic cell transplant patients at least 5 yr after treatment: a comparison with healthy controls. Eur J Haematol 2005; 74: 304–308.
Knobel H, Loge JH, Nordøy T, Kolstad AL, Espevik T, Kvaløy S et al. High level of fatigue in lymphoma patients treated with high dose therapy. J Pain Symptom Manage 2000; 19: 446–456.
Hann DM, Garovoy N, Finkelstein B, Jacobsen PB, Azzarello LM, Fields KK . Fatigue and quality of life in breast cancer patients undergoing autologous stem cell transplantation. J Pain Symptom Manage 1999; 17: 311–319.
Brandberg Y, Michelson H, Nilsson B, Bolund C, Erikstein B, Hietanen P et al. Quality of life in women with breast cancer during the first year after random assignment to adjuvant treatment with marrow-supported high-dose chemotherapy with cyclophosphamide, thiotepa, and carboplatin or tailored therapy with Fluorouracil, epirubicin, and cyclophosphamide: Scandinavian Breast Group Study 9401. J Clin Oncol 2003; 21: 3659–3664.
Prieto JM, Blanch J, Atala J, Carreras E, Rovira M, Cirera E et al. Clinical factors associated with fatigue in haematologic cancer patients receiving stem-cell transplantation. Eur J Cancer 2006; 42: 1749–1755.
Diez-Campelo M, Perez-Simon JA, Gonzalez-Porras JR, Garcia-Cecilia JM, Salinero M, Caballero MD et al. Quality of life assessment in patients undergoing reduced intensity conditioning allogeneic as compared to autologous transplantation: results of a prospective study. Bone Marrow Transplant 2004; 34: 729–738.
Lee SJ, Kim HT, Ho VT, Cutler C, Alyea EP, Soiffer RJ et al. Quality of life associated with acute and chronic graft-versus-host disease. Bone Marrow Transplant 2006; 38: 305–310.
Scherwath A, Schirmer L, Kruse M, Ernst G, Eder M, Dinkel A et al. Cognitive functioning in allogeneic hematopoietic stem cell transplantation recipients and its medical correlates: a prospective multicenter study. Psychooncology 2013; 22: 1509–1516.
Bacigalupo A . Hematopoietic stem cell transplants after reduced intensity conditioning regimen (RI-HSCT): report of a workshop of the European group for Blood and Marrow Transplantation (EBMT). Bone Marrow Transplant 2000; 25: 803–805.
Smets E, Garssen B, Bonke B, de Haes J . The multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res 1995; 39: 315–325.
Smets EM, Garssen B, Cull A, de Haes JC . Application of the multidimensional fatigue inventory (MFI-20) in cancer patients receiving radiotherapy. Br J Cancer 1996; 73: 241–245.
Schwarz R, Krauss O, Hinz A . Fatigue in the general population. Onkologie 2003; 26: 140–144.
Elbers RG, van Wegen EE, Verhoef J, Kwakkel G . Reliability and structural validity of the Multidimensional Fatigue Inventory (MFI) in patients with idiopathic Parkinson's disease. Parkinsonism Relat Disord 2012; 18: 532–536.
Herrmann-Lingen C, Buss U, Snaith P Hospital Anxiety and Depression Scale-Deutsche Version (HADS-D). Huber: Bern, Switzerland, 2011.
Zigmond AS, Snaith RP . The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983; 67: 361–370.
Jacobsen PB, Donovan KA, Weitzner MA . Distinguishing fatigue and depression in patients with cancer. Semin Clin Neuropsychiatry 2003; 8: 229–240.
Cohen J . A power primer. Psychol Bull 1992; 112: 155.
Lakens D . Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol 2013; 4: 863.
Norman GR, Sloan JA, Wyrwich KW . Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 2003; 41: 582–592.
SPSS Statistics for Windows. Version 20. IBM Corporation: Armonk, NY, USA, 2011.
R. R Project for Statistical Computing. Version 3.2.2. Vienna, Austria, 2010. https://www.R-project.org/.
Larsen J, Nordström G, Björkstrand B, Ljungman P, Gardulf A . Symptom distress, functional status and health‐related quality of life before high‐dose chemotherapy with stem‐cell transplantation. Eur J Cancer Care 2003; 12: 71–80.
Sherman AC, Simonton S, Latif U, Spohn R, Tricot G . Psychosocial adjustment and quality of life among multiple myeloma patients undergoing evaluation for autologous stem cell transplantation. Bone Marrow Transplant 2004; 33: 955–962.
Heinonen H, Volin L, Uutela A, Zevon M, Barrick C, Ruutu T . Quality of life and factors related to perceived satisfaction with quality of life after allogeneic bone marrow transplantation. Ann Hematol 2001; 80: 137–143.
Baker KS, Gurney JG, Ness KK, Bhatia R, Forman SJ, Francisco L et al. Late effects in survivors of chronic myeloid leukemia treated with hematopoietic cell transplantation: results from the Bone Marrow Transplant Survivor Study. Blood 2004; 104: 1898–1906.
Sprague S, Matta JM, Bhandari M, Dodgin D, Clark CR, Kregor P et al. Multicenter collaboration in observational research: improving generalizability and efficiency. J Bone Joint Surg Am 2009; 91 (Suppl 3): 80–86.
Buffart LM, Ros WJG, Chinapaw MJM, Brug J, Knol DL, Korstjens I et al. Mediators of physical exercise for improvement in cancer survivors' quality of life. Psycho-Oncology 2014; 23: 330–338.
Acknowledgements
This work was supported by the German foundation José Carreras Leukämie-Stiftung e.V. (grant nos. DJCLS R 04/29pf, DJCLS R 07/37pf and DJCLS R 10/38p). The funding source was not involved in any stage of the research process.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Esser, P., Kuba, K., Mehnert, A. et al. Investigating the temporal course, relevance and risk factors of fatigue over 5 years: a prospective study among patients receiving allogeneic HSCT. Bone Marrow Transplant 52, 753–758 (2017). https://doi.org/10.1038/bmt.2016.344
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.344
This article is cited by
-
International recommendations for screening and preventative practices for long-term survivors of transplantation and cellular therapy: a 2023 update
Bone Marrow Transplantation (2024)
-
Cognitive impairments correlate with increased central nervous system immune activation after allogeneic haematopoietic stem cell transplantation
Leukemia (2023)
-
Impact of chronic graft-versus-host disease on quality of life and cognitive function of long-term transplant survivors after allogeneic hematopoietic stem cell transplantation with total body irradiation
Radiation Oncology (2022)
-
Reduced prefrontal cortex and sympathetic nervous system activity correlate with fatigue after aHSCT
Bone Marrow Transplantation (2022)
-
Clinical characterization and cytokine profile of fatigue in hematologic malignancy patients with chronic graft-versus-host disease
Bone Marrow Transplantation (2021)