Abstract
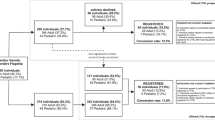
Informed consent (IC) struggles to meet the ethical principles it strives to embody in the context of hematopoietic cell transplantation (HCT). Patients often participate in multiple clinical trials making it difficult to effectively inform the participants and fulfill complex regulations. The recent Notice of Proposed Rule Making would make major changes to federal requirements, providing a timely opportunity to evaluate existing practice. Twenty health care professionals within a Midwest Academic Medical Center involved in obtaining IC in the HCT clinic or involved in patient care during or after the IC process were interviewed to understand: (1) how they approached the IC process; (2) how they described a ‘successful’ IC process; and (3) opportunities for innovation. Narrative and discourse analyses of interviews indicate that providers understand IC to be a collaborative process requiring engagement and participation of providers, patients and caregivers. ‘Markers of success’ were identified including cognitive, affective and procedural markers focusing on patient understanding and comfort with the decision to participate. Opportunities for innovating the process included use of decision aids and tablet-based technology, and better use of patient portals. Our findings suggest specific interventions for the IC process that could support the process of consent for providers, patients and caregivers.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Kline RM . Pediatric Hematopoietic Stem Cell Transplantation. Informa Healthcare USA, Inc.: New York, NY, USA, 2006.
Nakamura R, Forman SJ . Reduced intensity conditioning for allogeneic hematopoietic cell transplantation: considerations for evidence-based GVHD prophylaxis. Expert Rev Hematol 2014; 7: 407–421.
Stevens PE, Pletsch PK . Ethical issues of informed consent: mothers’ experiences enrolling their children in bone marrow transplantation research. Cancer Nurs 2002; 25: 81–87.
Gemmill R, Cooke L, Williams AC, Grant M . Informal caregivers of hematopoietic cell transplant patients: a review and recommendations for interventions and research. Cancer Nurs 2011; 34: E13–E21.
Keusch F, Rao R, Chang L, Lepkowski J, Reddy P, Choi SW . Participation in clinical research: perspectives of adult patients and parents of pediatric patients undergoing hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2014; 20: 1604–1611.
Mosher CE, Redd WH, Rini CM, Burkhalter JE, DuHamel KN . Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: a review of the literature. Psychooncology 2009; 18: 113–127.
Arora NK . Interacting with cancer patients: the significance of physicians’ communication behavior. Soc Sci Med 2003; 57: 791–806.
Rao JK, Anderson LA, Inui TS, Frankel RM . Communication interventions make a difference in conversations between physicians and patients: a systematic review of the evidence. Med Care 2007; 45: 340–349.
Epstein RM, Street RL . Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering 2007. http://appliedresearch.cancer.gov/areas/pcc/communication/pcc_monograph.pdf.
Juraskova I, Butow P, Bonner C, Bell ML, Smith AB, Seccombe M et al. Improving decision making about clinical trial participation- a randomised controlled trial of a decision aid for women considering participation in the IBIS-II breast cancer prevention trial. Br J Cancer 2014; 111: 1–7.
Denzen EM, Santibáñez MEB, Moore H, Foley A, Gersten ID, Gurgol C et al. Easy-to-read informed consent forms for hematopoietic cell transplantation clinical trials. Biol Blood Marrow Transplant 2012; 18: 183–189.
Stewart MA . Effective physician-patient communication and health outcomes: a review. CMAJ 1995; 152: 1423–1433.
Hekkenberg RJ, Irish JC, Rotstein LE, Brown DH, Gullane PJ . Informed consent in head and neck surgery: how much do patients actually remember? J Otolaryngol 1997; 26: 155–159.
Fayter D, McDaid C, Eastwood A . A systematic review highlights threats to validity in studies of barriers to cancer trial participation. J Clin Epidemiol 2007; 60: 990–1001.
Albala I, Doyle M, Appelbaum PS . The evolution of consent forms for research: a quarter century of changes. IRB 2010; 32: 7–11.
Burgess MM . Proposing modesty for informed consent. Soc Sci Med 2007; 65: 2284–2295.
Platt J, Thiel DB, Kardia SLR, Choi SW . Innovating consent for pediatric HCT patients. Bone Marrow Transplant 2016; 51: 885–888.
Lo B . Resolving Ethical Dilemmas: A Guide for Clinicians, 2nd edn. Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2000.
Emanuel EJ . Reform of clinical research regulations, finally. N Engl J Med 2015; 373: 2296–2299.
US Department of Health and Human Services. The Belmont Report. 1979. http://www.hhs.gov/ohrp/humansubjects/guidance/belmont.html.
Feldman MS, Skoldberg K, Brown RN, Horner D . Making sense of stories: a rhetorical approach to narrative analysis. J Public Adm Res Theory 2004; 14: 147–170.
Edwards D . Discourse and Cognition. SAGE Publications: London, UK and Thousand Oaks, CA, USA, 1997.
Jorgensen M, Phillips L . Discourse Analysis as Theory and Method. SAGE Publications: London, UK, 2002.
Flory J, Emanuel E . Interventions to improve research participants' understanding in informed consent for research: a systematic review. JAMA 2004; 292: 1593–1601.
Rao KHS . Informed consent: an ethical obligation or legal compulsion? J Cutan Aesthet Surg 2008; 1: 33–35.
Charles C, Gafni A, Whelan T, O’Brien MA . Cultural influences on the physician-patient encounter: the case of shared treatment decision-making. Patient Educ Couns 2006; 63: 262–267.
Roberts KJ, Revenson TA, Urken ML, Fleszar S, Cipollina R, Rowe ME et al. Testing with feedback improves recall of information in informed consent: a proof of concept study. Patient Educ Couns 2016; 99: 1377–1381.
Rowbotham MC, Astin J, Greene K, Cummings SR . Interactive informed consent: randomized comparison with paper consents. PLoS ONE 2013; 8: e58603.
Brehaut JC, Lott A, Fergusson DA, Shojania KG, Kimmelman J, Saginur R . Can patient decision aids help people make good decisions about participating in clinical trials? A study protocol. Implement Sci 2008; 3: 38.
Nishimura A, Carey J, Erwin PJ, Tilburt JC, Murad MH, McCormick JB . Improving understanding in the research informed consent process: a systematic review of 54 interventions tested in randomized control trials. BMC Med Ethics 2013; 14: 28.
Acknowledgements
This work was supported by grants from the National Institute of Health (5R01HD067264-04 to JP and K23A1091623 to SWC) and the A. Alfred Taubman Medical Research Institute Emerging Scholar/Edith Briskin Shirly K. Schlafer Foundation Award (to SWC).
Author contributions
MR performed all the health care provider interviews. MR, SWC and JP designed the research and analyzed the data. MR wrote the manuscript and produced the figures and tables. JP and SWC also wrote, edited and approved the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Raj, M., Choi, S. & Platt, J. A qualitative exploration of the informed consent process in hematopoietic cell transplantation clinical research and opportunities for improvement. Bone Marrow Transplant 52, 292–298 (2017). https://doi.org/10.1038/bmt.2016.252
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.252