Abstract
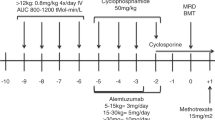
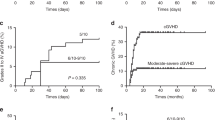
Autoimmune hemolysis (AH) and immune thrombocytopenic purpura (ITP) are recognized complications after cord blood transplantation (CBT). We evaluated the incidence and characteristics of AH/ITP after double-unit CBT in a day 100 landmark analysis of 152 patients (median age 36 years, range 0.9–70 years) transplanted for hematologic malignancies with myeloablative or nonmyeloablative conditioning and calcineurin inhibitor (CNI)/mycophenolate mofetil. With a median 5.2-year (range 1.6–9.7 years) survivor follow-up, 10 patients developed autoimmune cytopenias (8 AH, 1 ITP, 1 both) at a median of 10.4 months (range 5.8–24.5) post CBT for a 7% cumulative incidence 3 years after the day 100 landmark. Six patients presented with severe disease (hemoglobin ⩽6 g/dL and/or platelets <20 × 109/L). All AH patients were direct antiglobulin test positive. All 10 cases developed during immunosuppression taper with 8 having prior acute GVHD. All 10 patients received rituximab 2–18 days after diagnosis, and corticosteroids combined with rituximab within <7 days was the most effective. No patient died of AH/ITP. AH/ITP occurs infrequently after CBT but may be life-threatening requiring emergency therapy. Rituximab combined with corticosteroids at diagnosis is warranted in patients with severe disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Drobyski WR, Potluri J, Sauer D, Gottschall JL . Autoimmune hemolytic anemia following T cell-depleted allogeneic bone marrow transplantation. Bone Marrow Transplant 1996; 17: 1093–1099.
Chen FE, Owen I, Savage D, Roberts I, Apperley J, Goldman JM et al. Late onset haemolysis and red cell autoimmunisation after allogeneic bone marrow transplant. Bone Marrow Transplant 1997; 19: 491–495.
Sanz J, Arriaga F, Montesinos P, Orti G, Lorenzo I, Cantero S et al. Autoimmune hemolytic anemia following allogeneic hematopoietic stem cell transplantation in adult patients. Bone Marrow Transplant 2007; 39: 555–561.
Daikeler T, Tyndall A . Autoimmunity following haematopoietic stem-cell transplantation. Best Pract Res Clin Haematol 2007; 20: 349–360.
Holbro A, Abinun M, Daikeler T . Management of autoimmune diseases after haematopoietic stem cell transplantation. Br J Haematol 2012; 157: 281–290.
Daikeler T, Labopin M, Ruggeri A, Crotta A, Abinun M, Hussein AA et al. New autoimmune diseases after cord blood transplantation: a retrospective study of EUROCORD and the Autoimmune Disease Working Party of the European Group for Blood and Marrow Transplantation. Blood 2013; 121: 1059–1064.
Radhi M, Rumelhart S, Tatman D, Goldman F . Severe autoimmune hemolytic anemia after unrelated umbilical cord blood transplant for familial hemophagocytic lymphohistiocytosis: significant improvement after treatment with rituximab. J Pediatr Hematol Oncol 2007; 29: 125–127.
Page KM, Mendizabal AM, Prasad VK, Martin PL, Parikh S, Wood S et al. Posttransplant autoimmune hemolytic anemia and other autoimmune cytopenias are increased in very young infants undergoing unrelated donor umbilical cord blood transplantation. Biol Blood Marrow Transplant 2008; 14: 1108–1117.
Chao MM, Levine JE, Ferrara JL, Cooling L, Cooke KR, Hutchinson RJ et al. Successful treatment of refractory immune hemolysis following unrelated cord blood transplant with Campath-1H. Pediatr Blood Cancer 2008; 50: 917–919.
Nomura S, Ishii K, Inami N, Matsuzaki T, Yamaoka M, Urase F et al. Antiglycoprotein IIb–IIIa autoantibody in a patient with immune thrombocytopenia after cord blood transplantation. Clin Appl Thromb Hemost 2009; 15: 123–124.
Sanz J, Arango M, Carpio N, Montesinos P, Moscardo F, Martin G et al. Autoimmune cytopenias after umbilical cord blood transplantation in adults with hematological malignancies: a single-center experience. Bone Marrow Transplant 2014; 49: 1084–1088.
Ponce DM, Zheng J, Gonzales AM, Lubin M, Heller G, Castro-Malaspina H et al. Reduced late mortality risk contributes to similar survival after double-unit cord blood transplantation compared with related and unrelated donor hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2011; 17: 1316–1326.
Ponce DM, Sauter C, Devlin S, Lubin M, Gonzales AM, Kernan NA et al. A novel reduced-intensity conditioning regimen induces a high incidence of sustained donor-derived neutrophil and platelet engraftment after double-unit cord blood transplantation. Biol Blood Marrow Transplant 2013; 19: 799–803.
Ponce DM, Gonzales A, Lubin M, Castro-Malaspina H, Giralt S, Goldberg JD et al. Graft-versus-host disease after double-unit cord blood transplantation has unique features and an association with engrafting unit-to-recipient HLA match. Biol Blood Marrow Transplant 2013; 19: 904–911.
Harnicar S, Ponce DM, Hilden P, Zheng J, Devlin SM, Lubin M et al. Intensified mycophenolate mofetil dosing and higher mycophenolic acid trough levels reduce severe acute graft-versus-host disease after double-unit cord blood transplantation. Biol Blood Marrow Transplant 2015; 21: 920–925.
Rowlings PA, Przepiorka D, Klein JP, Gale RP, Passweg JR, Henslee-Downey PJ et al. IBMTR Severity Index for grading acute graft-versus-host disease: retrospective comparison with Glucksberg grade. Br J Haematol 1997; 97: 855–864.
Bass GF, Tuscano ET, Tuscano JM . Diagnosis and classification of autoimmune hemolytic anemia. Autoimmun Rev 2014; 13: 560–564.
Zantek ND, Koepsell SA, Tharp DR Jr, Cohn CS . The direct antiglobulin test: a critical step in the evaluation of hemolysis. Am J Hematol 2012; 87: 707–709.
Neunert C, Lim W, Crowther M, Cohen A, Solberg L Jr, Crowther MA et al. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood 2011; 117: 4190–4207.
Brighton TA, Evans S, Castaldi PA, Chesterman CN, Chong BH . Prospective evaluation of the clinical usefulness of an antigen-specific assay (MAIPA) in idiopathic thrombocytopenic purpura and other immune thrombocytopenias. Blood 1996; 88: 194–201.
Warner MN, Moore JC, Warkentin TE, Santos AV, Kelton JG . A prospective study of protein-specific assays used to investigate idiopathic thrombocytopenic purpura. Br J Haematol 1999; 104: 442–447.
Penalver FJ, Alvarez-Larran A, Diez-Martin JL, Gallur L, Jarque I, Caballero D et al. Rituximab is an effective and safe therapeutic alternative in adults with refractory and severe autoimmune hemolytic anemia. Ann Hematol 2010; 89: 1073–1080.
Acknowledgements
This work was supported, in part, by the Gabrielle’s Angel Foundation for Cancer Research (to JNB), the Society of Memorial Sloan Kettering Cancer Center (to JNB and SG), the Memorial Sloan Kettering Cancer Center Translational and Integrative Medicine Research Program (to JNB), P01 CA23766 from the National Cancer Institute, National Institutes of Health and the Memorial Sloan Kettering Cancer Center Support Grant/Core Grant (P30 CA008748).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bhatt, V., Shune, L., Lauer, E. et al. Autoimmune hemolysis and immune thrombocytopenic purpura after cord blood transplantation may be life-threatening and warrants early therapy with rituximab. Bone Marrow Transplant 51, 1579–1583 (2016). https://doi.org/10.1038/bmt.2016.228
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.228
This article is cited by
-
Immune-mediated cytopenias (IMCs) after HSCT for pediatric non-malignant disorders: epidemiology, risk factors, pathogenesis, and treatment
European Journal of Pediatrics (2023)
-
Applying Rituximab During the Conditioning Regimen Prevents Epstein–Barr Virus Infection Following Allogeneic Hematopoietic Stem Cell Transplant in a Children’s Cohort: A Retrospective Case–Control Study
Infectious Diseases and Therapy (2023)
-
Consensus opinion on immune-mediated cytopenias after hematopoietic cell transplant for inherited metabolic disorders
Bone Marrow Transplantation (2021)
-
Eltrombopag is an effective and safe therapy for refractory thrombocytopenia after haploidentical hematopoietic stem cell transplantation
Bone Marrow Transplantation (2019)
-
Immune-Mediated Cytopenias After Hematopoietic Cell Transplantation: Pathophysiology, Clinical Manifestations, Diagnosis, and Treatment Strategies
Current Oncology Reports (2019)