Abstract
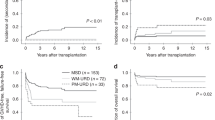
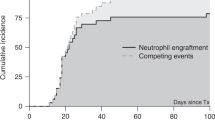
Allogeneic stem cell transplantation from HLA-matched siblings (MSD-SCT) for elderly patients with severe aplastic anemia (SAA) is not a widely accepted first-line treatment. Recently, fludarabine, lower-dose cyclophosphamide and antithymocyte globulin conditioning (Flu/lower-dose Cy/ATG) with lower toxicities has been investigated. To determine whether this regimen can overcome the negative effects of age, we analyzed 117 adult patients with SAA who received MSD-SCT using Flu/lower-dose Cy/ATG, and compared outcomes between 63 younger age group (YAG; ⩽40 years) and 54 older age group (OAG; >40 years) patients. No primary graft failure was observed. Neutrophil engraftment was significantly faster in the YAG compared with the OAG (12 vs 13 days; P=0.04). The incidences of acute grade II–IV (9.5% vs 9.3% at day 100; P=0.42) and chronic GVHD (8.1% vs 9.5% at 5 years; P=0.80), secondary graft failure (20.8% vs 7.9% at 5 years; P=0.11) and transplant-related mortality (5.4% and 11.1% at 5 years; P=0.91) were not significantly different between the YAG and OAG. In addition, failure-free (73.7% vs 81.0% at 5 years; P=0.73) and overall survival rates (93.7% vs 88.9% at 5 years; P=0.20) were comparable. Our results suggest that MSD-SCT using Flu/lower-dose Cy/ATG may be a feasible first-line treatment even in older patients with SAA.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Shin SH, Lee SE, Lee JW . Recent advances in treatment of aplastic anemia. Korean J Intern Med 2014; 29: 713–726.
Marsh JC, Ball SE, Cavenagh J, Darbyshire P, Dokal I, Gordon-Smith EC et al. Guidelines for the diagnosis and management of aplastic anaemia. Br J Haematol 2009; 147: 43–70.
Scheinberg P, Young NS . How I treat acquired aplastic anemia. Blood 2012; 120: 1185–1196.
Young NS . Current concepts in the pathophysiology and treatment of aplastic anemia. Hematology Am Soc Hematol Educ Program 2013; 2013: 76–81.
Doney K, Leisenring W, Storb R, Appelbaum FR . Primary treatment of acquired aplastic anemia: outcomes with bone marrow transplantation and immunosuppressive therapy. Seattle Bone Marrow Transplant Team. Ann Intern Med 1997; 126: 107–115.
Gupta V, Eapen M, Brazauskas R, Carreras J, Aljurf M, Gale RP et al. Impact of age on outcomes after bone marrow transplantation for acquired aplastic anemia using HLA-matched sibling donors. Haematologica 2010; 95: 2119–2125.
Bacigalupo A, Brand R, Oneto R, Bruno B, Socie G, Passweg J et al. Treatment of acquired severe aplastic anemia: bone marrow transplantation compared with immunosuppressive therapy—The European Group for Blood and Marrow Transplantation experience. Semin Hematol 2000; 37: 69–80.
Bacigalupo A, Socie G, Hamladji RM, Aljurf M, Maschan A, Kyrcz-Krzemien S et al. Current outcome of HLA identical sibling versus unrelated donor transplants in severe aplastic anemia: an EBMT analysis. Haematologica 2015; 100: 696–702.
Sangiolo D, Storb R, Deeg HJ, Flowers ME, Martin PJ, Sandmaier BM et al. Outcome of allogeneic hematopoietic cell transplantation from HLA-identical siblings for severe aplastic anemia in patients over 40 years of age. Biol Blood Marrow Transplant 2010; 16: 1411–1418.
Socie G . Allogeneic BM transplantation for the treatment of aplastic anemia: current results and expanding donor possibilities. Hematology Am Soc Hematol Educ Program 2013; 2013: 82–86.
Storb R, Etzioni R, Anasetti C, Appelbaum FR, Buckner CD, Bensinger W et al. Cyclophosphamide combined with antithymocyte globulin in preparation for allogeneic marrow transplants in patients with aplastic anemia. Blood 1994; 84: 941–949.
Locatelli F, Bruno B, Zecca M, Van-Lint MT, McCann S, Arcese W et al. Cyclosporin A and short-term methotrexate versus cyclosporin A as graft versus host disease prophylaxis in patients with severe aplastic anemia given allogeneic bone marrow transplantation from an HLA-identical sibling: results of a GITMO/EBMT randomized trial. Blood 2000; 96: 1690–1697.
Ades L, Mary JY, Robin M, Ferry C, Porcher R, Esperou H et al. Long-term outcome after bone marrow transplantation for severe aplastic anemia. Blood 2004; 103: 2490–2497.
Kahl C, Leisenring W, Deeg HJ, Chauncey TR, Flowers ME, Martin PJ et al. Cyclophosphamide and antithymocyte globulin as a conditioning regimen for allogeneic marrow transplantation in patients with aplastic anaemia: a long-term follow-up. Br J Haematol 2005; 130: 747–751.
Champlin RE, Perez WS, Passweg JR, Klein JP, Camitta BM, Gluckman E et al. Bone marrow transplantation for severe aplastic anemia: a randomized controlled study of conditioning regimens. Blood 2007; 109: 4582–4585.
Resnick IB, Aker M, Shapira MY, Tsirigotis PD, Bitan M, Abdul-Hai A et al. Allogeneic stem cell transplantation for severe acquired aplastic anaemia using a fludarabine-based preparative regimen. Br J Haematol 2006; 133: 649–654.
George B, Mathews V, Viswabandya A, Kavitha ML, Srivastava A, Chandy M . Fludarabine and cyclophosphamide based reduced intensity conditioning (RIC) regimens reduce rejection and improve outcome in Indian patients undergoing allogeneic stem cell transplantation for severe aplastic anemia. Bone Marrow Transplant 2007; 40: 13–18.
Kim H, Lee JH, Joo YD, Bae SH, Hyun MS, Lee JH et al. A randomized comparison of cyclophosphamide vs reduced dose cyclophosphamide plus fludarabine for allogeneic hematopoietic cell transplantation in patients with aplastic anemia and hypoplastic myelodysplastic syndrome. Ann Hematol 2012; 91: 1459–1469.
Srinivasan R, Takahashi Y, McCoy JP, Espinoza-Delgado I, Dorrance C, Igarashi T et al. Overcoming graft rejection in heavily transfused and allo-immunised patients with bone marrow failure syndromes using fludarabine-based haematopoietic cell transplantation. Br J Haematol 2006; 133: 305–314.
Gomez-Almaguer D, Vela-Ojeda J, Jaime-Perez JC, Gutierrez-Aguirre CH, Cantu-Rodriguez OG, Sobrevilla-Calvo P et al. Allografting in patients with severe, refractory aplastic anemia using peripheral blood stem cells and a fludarabine-based conditioning regimen: the Mexican experience. Am J Hematol 2006; 81: 157–161.
Cho BS, Eom KS, Kim YJ, Kim HJ, Lee S, Min CK et al. HLA-matched sibling transplantation with BM and CD34(+)-purified PBSCs in adult patients with high-risk severe aplastic anemia to overcome graft rejection without an increase in GVHD. Bone Marrow Transplant 2010; 45: 1497–1501.
Choi SM, Lee DG, Lim J, Park SH, Choi JH, Yoo JH et al. Comparison of quantitative cytomegalovirus real-time PCR in whole blood and pp65 antigenemia assay: clinical utility of CMV real-time PCR in hematopoietic stem cell transplant recipients. J Korean Med Sci 2009; 24: 571–578.
Maury S, Bacigalupo A, Anderlini P, Aljurf M, Marsh J, Socie G et al. Improved outcome of patients older than 30 years receiving HLA-identical sibling hematopoietic stem cell transplantation for severe acquired aplastic anemia using fludarabine-based conditioning: a comparison with conventional conditioning regimen. Haematologica 2009; 94: 1312–1315.
Oelschlaegel U, Besson I, Arnoulet C, Sainty D, Nowak R, Naumann R et al. A standardized flow cytometric method for screening paroxysmal nocturnal haemoglobinuria (PNH) measuring CD55 and CD59 expression on erythrocytes and granulocytes. Clin Lab Haematol 2001; 23: 81–90.
Battiwalla M, Hepgur M, Pan D, McCarthy PL, Ahluwalia MS, Camacho SH et al. Multiparameter flow cytometry for the diagnosis and monitoring of small GPI-deficient cellular populations. Cytometry B Clin Cytom B 2010; 78: 348–356.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 2005; 106: 2912–2919.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant 1995; 15: 825–828.
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant 2005; 11: 945–956.
McDonald GB, Hinds MS, Fisher LD, Schoch HG, Wolford JL, Banaji M et al. Veno-occlusive disease of the liver and multiorgan failure after bone marrow transplantation: a cohort study of 355 patients. Ann Intern Med 1993; 118: 255–267.
Silva Lde P, Patah PA, Saliba RM, Szewczyk NA, Gilman L, Neumann J et al. Hemorrhagic cystitis after allogeneic hematopoietic stem cell transplants is the complex result of BK virus infection, preparative regimen intensity and donor type. Haematologica 2010; 95: 1183–1190.
The National Cancer Institute Common Terminology Criteria for adverse events version 3.0. Available at: http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf (accessed 14 December 2015).
Copelan E, Casper JT, Carter SL, van Burik JA, Hurd D, Mendizabal AM et al. A scheme for defining cause of death and its application in the T cell depletion trial. Biol Blood Marrow Transplant 2007; 13: 1469–1476.
Deeg HJ, Maris MB, Scott BL, Warren EH . Optimization of allogeneic transplant conditioning: not the time for dogma. Leukemia 2006; 20: 1701–1705.
Slattery JT, Kalhorn TF, McDonald GB, Lambert K, Buckner CD, Bensinger WI et al. Conditioning regimen-dependent disposition of cyclophosphamide and hydroxycyclophosphamide in human marrow transplantation patients. J Clin Oncol 1996; 14: 1484–1494.
Morandi P, Ruffini PA, Benvenuto GM, Raimondi R, Fosser V . Cardiac toxicity of high-dose chemotherapy. Bone Marrow Transplant 2005; 35: 323–334.
Seber A, Shu XO, Defor T, Sencer S, Ramsay N . Risk factors for severe hemorrhagic cystitis following BMT. Bone Marrow Transplant 1999; 23: 35–40.
Or R, Weiss L, Amir G, Tejman S, Polliack A . The prophylactic potential of fludarabine monophosphate in graft-versus-host disease after bone marrow transplantation in murine models. Bone Marrow Transplant 2000; 25: 263–266.
Weiss L, Abdul-Hai A, Or R, Amir G, Polliack A . Fludarabine in combination with cyclophosphamide decreases incidence of GVHD and maintains effective graft-versus-leukemia effect after allogeneic stem cell transplantation in murine lymphocytic leukemia. Bone Marrow Transplant 2003; 31: 11–15.
Morishima Y, Kawase T, Malkki M, Morishima S, Spellman S, Kashiwase K et al. Significance of ethnicity in the risk of acute graft-versus-host disease and leukemia relapse after unrelated donor hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2013; 19: 1197–1203.
Remberger M, Aschan J, Lonnqvist B, Carlens S, Gustafsson B, Hentschke P et al. An ethnic role for chronic, but not acute, graft-versus-host disease after HLA-identical sibling stem cell transplantation. Eur J Haematol 2001; 66: 50–56.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Shin, S., Jeon, Y., Yoon, J. et al. Comparable outcomes between younger (⩽40 years) and older (>40 years) adult patients with severe aplastic anemia after HLA-matched sibling stem cell transplantation using fludarabine-based conditioning. Bone Marrow Transplant 51, 1456–1463 (2016). https://doi.org/10.1038/bmt.2016.171
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.171
This article is cited by
-
Incidence and risk factors of hepatic veno-occlusive disease/sinusoidal obstruction syndrome after allogeneic hematopoietic cell transplantation in adults with prophylactic ursodiol and intravenous heparin or prostaglandin E1
Bone Marrow Transplantation (2021)
-
Excellent outcomes of hematopoietic stem cell transplantation with total nodal irradiation and antithymocyte globulin conditioning in severe aplastic anemia with advanced age and/or severe comorbidity
Bone Marrow Transplantation (2020)
-
Posttransplant cyclophosphamide in allogeneic bone marrow transplantation for the treatment of nonmalignant hematological diseases
Bone Marrow Transplantation (2020)
-
Comparison of HLA-matched sibling and unrelated donor transplantation in adult patients with acquired severe aplastic anemia
Bone Marrow Transplantation (2020)
-
Successful outcomes of second hematopoietic stem cell transplantation with total nodal irradiation and ATG conditioning for graft failure in adult patients with severe aplastic anemia
Bone Marrow Transplantation (2018)