Abstract
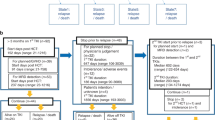
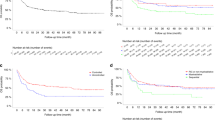
To assess the impact of minimal residual disease (MRD) and tyrosine kinase inhibitor (TKI) administration on allogeneic hematopoietic cell transplantation (allo-HCT) for Ph-positive ALL (Ph+ALL), we retrospectively analyzed data from a registry database for 432 adult Ph+ALL patients in first CR (CR1) who received pre-transplant TKI administration. Negative MRD (MRD(−)) at allo-HCT was achieved in 277 patients. OS in patients transplanted in MRD(−) was significantly better than that in patients transplanted in MRD(+) (MRD(−): 67% vs MRD(+): 55% at 4 years; P=0.001). MRD(−) at allo-HCT was a significant risk factor for survival along with age at allo-HCT in multivariate analyses. Incidence of relapse in patients transplanted in MRD(−) was significantly lower than that in patients transplanted in MRD(+) (MRD(−): 19% vs MRD(+): 29% at 4 years; P=0.006). In multivariate analyses, MRD(+) at allo-HCT was a significant risk factor for relapse. A post-transplant TKI was administered to 103 patients. In subanalyses regarding the effect of post-transplant TKI administration, post-transplant TKI administration was a significant risk factor for relapse in multivariate analyses (P<0.0001). MRD status at allo-HCT is one of the most important predictive factors for Ph+ALL patients transplanted in CR1.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Fielding AK . Current treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia. Hematol ASH Educ Program 2011; 2011: 231–237.
Mizuta S, Matsuo K, Nishiwaki S, Imai K, Kanamori H, Ohashi K et al. Pre-transplant administration of imatinib for allogeneic hematopoietic stem cell transplantation in patients with BCR-ABL-positive acute lymphoblastic leukemia. Blood 2014; 123: 2325–2332.
Zhang FH, Ling YW, Zhai X, Zhang Y, Huang F, Fan ZP et al. The effect of imatinib therapy on the outcome of allogeneic stem cell transplantation in adults with Philadelphia chromosome-positive acute lymphoblastic leukemia. Hematology 2013; 18: 151–157.
Tanguy Schmidt A, Rousselot P, Chalandon Y, Cayuela JM, Hayette S, Vekemans MC et al. Long-term follow-up of the imatinib GRAAPH-2003 study in newly diagnosed patients with de novo Philadelphia chromosome-positive acute lymphoblastic leukemia: a GRAALL study. Biol Blood Marrow Transplant 2013; 19: 150–155.
Biondi A, Schrappe M, De Lorenzo P, Castor A, Lucchini G, Gandemer V et al. Imatinib after induction for treatment of children and adolescents with Philadelphia-chromosome-positive acute lymphoblastic leukaemia (EsPhALL): a randomised, open-label, intergroup study. Lancet Oncol 2012; 13: 936–945.
Yanada M, Takeuchi J, Sugiura I, Akiyama H, Usui N, Yagasaki F et al. High complete remission rate and promising outcome by combination of imatinib and chemotherapy for newly diagnosed BCR-ABL-positive acute lymphoblastic leukemia: a phase II study by the Japan Adult Leukemia Study Group. J Clin Oncol 2006; 24: 460–466.
Schultz KR, Bowman WP, Aledo A, Slayton WB, Sather H, Devidas M et al. Improved early event-free survival with imatinib in Philadelphia chromosome-positive acute lymphoblastic leukemia: a children's oncology group study. J Clin Oncol 2009; 27: 5175–5181.
Yanada M, Sugiura I, Takeuchi J, Akiyama H, Maruta A, Ueda Y et al. Prospective monitoring of BCR-ABL1 transcript levels in patients with Philadelphia chromosome-positive acute lymphoblastic leukaemia undergoing imatinib-combined chemotherapy. Br J Haematol 2008; 143: 503–510.
Ravandi F, Jorgensen JL, Thomas DA, O'Brien S, Garris R, Faderl S et al. Detection of MRD may predict the outcome of patients with Philadelphia chromosome-positive ALL treated with tyrosine kinase inhibitors plus chemotherapy. Blood 2013; 122: 1214–1221.
Hoelzer D . Monitoring and managing minimal residual disease in acute lymphoblastic leukemia. Am Soc Clin Oncol Educ Book 2013, 290–293.
Jeha S, Coustan Smith E, Pei D, Sandlund JT, Rubnitz JE, Howard SC et al. Impact of tyrosine kinase inhibitors on minimal residual disease and outcome in childhood Philadelphia chromosome-positive acute lymphoblastic leukemia. Cancer 2014; 120: 1514–1519.
Lee S, Kim DW, Cho BS, Yoon JH, Shin SH, Yahng SA et al. Impact of minimal residual disease kinetics during imatinib-based treatment on transplantation outcome in Philadelphia chromosome-positive acute lymphoblastic leukemia. Leukemia 2012; 26: 2367–2374.
Nishiwaki S, Miyamura K, Kato C, Terakura S, Ohashi K, Sakamaki H et al. Impact of post-transplant imatinib administration on Philadelphia chromosome-positive acute lymphoblastic leukaemia. Anticancer Res 2010; 30: 2415–2418.
Bachanova V, Marks DI, Zhang MJ, Wang H, de Lima M, Aljurf MD et al. Ph+ ALL patients in first complete remission have similar survival after reduced intensity and myeloablative allogeneic transplantation: impact of tyrosine kinase inhibitor and minimal residual disease. Leukemia 2014; 28: 658–665.
Ribera JM, Oriol A, Gonzalez M, Vidriales B, Brunet S, Esteve J et al. Concurrent intensive chemotherapy and imatinib before and after stem cell transplantation in newly diagnosed Philadelphia chromosome-positive acute lymphoblastic leukemia. Final results of the CSTIBES02 trial. Haematologica 2010; 95: 87–95.
Burke MJ, Trotz B, Luo X, Baker KS, Weisdorf DJ, Wagner JE et al. Allo-hematopoietic cell transplantation for Ph chromosome-positive ALL: impact of imatinib on relapse and survival. Bone Marrow Transplant 2009; 43: 107–113.
Caocci G, Vacca A, Ledda A, Murgia F, Piras E, Greco M et al. Prophylactic and preemptive therapy with dasatinib after hematopoietic stem cell transplantation for Philadelphia chromosome-positive acute lymphoblastic leukemia. Biol Blood Marrow Transplant 2012; 18: 652–654.
Watanabe A, Chansu S, Ogawa A, Asami K, Imamura M . Prophylactic post-transplant dasatinib administration in a pediatric patient with Philadelphia chromosome-positive acute lymphoblastic leukemia. Pediatr Int 2013; 55: e56–e58.
Pfeifer H, Wassmann B, Bethge W, Dengler J, Bornhauser M, Stadler M et al. Randomized comparison of prophylactic and minimal residual disease-triggered imatinib after allogeneic stem cell transplantation for BCR-ABL1-positive acute lymphoblastic leukemia. Leukemia 2013; 27: 1254–1262.
Mizuta S, Matsuo K, Maeda T, Yujiri T, Hatta Y, Kimura Y et al. Prognostic factors influencing clinical outcome of allogeneic hematopoietic stem cell transplantation following imatinib-based therapy in BCR-ABL-positive ALL. Blood Cancer J 2012; 2: e72.
Fujisawa S, Matsuo K, Mizuta S, Akiyama H, Ueda Y, Aoyama Y et al. Imatinib-based chemotherapy for newly diagnosed BCR–ABL positive acute lymphoblastic leukemia: Japan Adult Leukemia Study Group (JALSG) Ph+ALL208 Study. Blood 2014; 124: 932.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant 1995; 15: 825–828.
Sullivan KM, Shulman HM, Storb R, Weiden PL, Witherspoon RP, McDonald GB et al. Chronic graft-versus-host disease in 52 patients: adverse natural course and successful treatment with combination immunosuppression. Blood 1981; 57: 267–276.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transplant 2009; 15: 367–369.
Sasazuki T, Juji T, Morishima Y, Kinukawa N, Kashiwabara H, Inoko H et al. Effect of matching of class I HLA alleles on clinical outcome after transplantation of hematopoietic stem cells from an unrelated donor. Japan Marrow Donor Program. N Engl J Med 1998; 339: 1177–1185.
Morishima Y, Sasazuki T, Inoko H, Juji T, Akaza T, Yamamoto K et al. The clinical significance of human leukocyte antigen (HLA) allele compatibility in patients receiving a marrow transplant from serologically HLA-A, HLA-B, and HLA-DR matched unrelated donors. Blood 2002; 99: 4200–4206.
Atsuta Y, Morishima Y, Suzuki R, Nagamura Inoue T, Taniguchi S, Takahashi S et al. Comparison of unrelated cord blood transplantation and HLA-mismatched unrelated bone marrow transplantation for adults with leukemia. Biol Blood Marrow Transplant 2012; 18: 780–787.
Matsuno N, Wake A, Uchida N, Ishiwata K, Araoka H, Takagi S et al. Impact of HLA disparity in the graft-versus-host direction on engraftment in adult patients receiving reduced-intensity cord blood transplantation. Blood 2009; 114: 1689–1695.
Ooi J, Takahashi S, Tomonari A, Tsukada N, Konuma T, Kato S et al. Unrelated cord blood transplantation after myeloablative conditioning in adults with acute myelogenous leukemia. Biol Blood Marrow Transplant 2008; 14: 1341–1347.
Nishiwaki S, Miyamura K, Ohashi K, Kurokawa M, Taniguchi S, Fukuda T et al. Impact of a donor source on adult Philadelphia chromosome-negative acute lymphoblastic leukemia: a retrospective analysis from the Adult Acute Lymphoblastic Leukemia Working Group of the Japan Society for Hematopoietic Cell Transplantation. Ann Oncol 2013; 24: 1594–1602.
Kaplan EL, Meier P . Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–481.
Peto R, Peto J . Asymptotically efficient rank invariant test procedures. J R Stat Soc A 1972; 135: 185–207.
Gooley TA, Leisenring W, Crowley J, Storer BE . Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 1999; 18: 695–706.
Scrucca L, Santucci A, Aversa F . Competing risk analysis using R: an easy guide for clinicians. Bone Marrow Transplant 2007; 40: 381–387.
Cox DR . Regression models and life tables. J R Stat Soc B 1972; 34: 187–220.
Fine J, Gray R . A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94: 496–509.
Talpaz M, Shah NP, Kantarjian H, Donato N, Nicoll J, Paquette R et al. Dasatinib in imatinib-resistant Philadelphia chromosome-positive leukemias. N Engl J Med 2006; 354: 2531–2541.
Soverini S, De Benedittis C, Papayannidis C, Paolini S, Venturi C, Iacobucci I et al. Drug resistance and BCR-ABL kinase domain mutations in Philadelphia chromosome-positive acute lymphoblastic leukemia from the imatinib to the second-generation tyrosine kinase inhibitor era: the main changes are in the type of mutations, but not in the frequency of mutation involvement. Cancer 2014; 120: 1002–1009.
Kantarjian HM, Cortes JE, Kim DW, Khoury HJ, Brummendorf TH, Porkka K et al. Bosutinib safety and management of toxicity in leukemia patients with resistance or intolerance to imatinib and other tyrosine kinase inhibitors. Blood 2014; 123: 1309–1318.
Quintas Cardama A, Kantarjian H, Cortes J . Third-generation tyrosine kinase inhibitors and beyond. Semin Hematol 2010; 47: 371–380.
Cortes JE, Kim DW, Pinilla Ibarz J, le Coutre P, Paquette R, Chuah C et al. A phase 2 trial of ponatinib in Philadelphia chromosome-positive leukemias. N Engl J Med 2013; 369: 1783–1796.
Kebriaei P, Saliba R, Rondon G, Chiattone A, Luthra R, Anderlini P et al. Long-term follow-up of allogeneic hematopoietic stem cell transplantation for patients with Philadelphia chromosome-positive acute lymphoblastic leukemia: impact of tyrosine kinase inhibitors on treatment outcomes. Biol Blood Marrow Transplant 2012; 18: 584–592.
Wassmann B, Pfeifer H, Stadler M, Bornhauser M, Bug G, Scheuring UJ et al. Early molecular response to posttransplantation imatinib determines outcome in MRD+ Philadelphia-positive acute lymphoblastic leukemia (Ph+ ALL). Blood 2005; 106: 458–463.
Acknowledgements
This study was supported in part by the Japan Leukemia Research Fund grant to SN, by a Research Grand for Allergic Disease and Immunology from the Japanese Ministry of Health, Labor and Welfare to YA and by a Japanese Grant-in-Aid for Scientific Research to JT.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
YO has received honoraria from Novartis and Bristol-Myers Squibb. ST has received honoraria and research funding from Novartis. NU has received honoraria from Otsuka Pharmaceutical Co., Kyowa Hakko Kirin Co., Chugai Pharmaceutical Co., Sumitomo Dainippon Pharma, Bristol-Myers Squibb, Daiichi Sankyo Company and Yakult Honsha, and travel, accommodations, expenses from Yakult Honsha and Kyowa Hakko Kirin Co. HN has received honoraria, speaker’s bureau, research funding, and travel, accommodations, expenses from Novartis and Bristol-Myers Squibb. TN-I has research funding from Tsubakimoto Co. and Wanbishi Archives Co. and patent pending with Tsubakimoto Co. YA has received honoraria from Otsuka Pharmaceutical Co., MDS Co. Ltd, Meiji Seika Pharma and Chugai Pharmaceutical Co., and travel, accommodations, expenses from Kyowa Hakko Kirin Co. The remaining authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Nishiwaki, S., Imai, K., Mizuta, S. et al. Impact of MRD and TKI on allogeneic hematopoietic cell transplantation for Ph+ALL: a study from the adult ALL WG of the JSHCT. Bone Marrow Transplant 51, 43–50 (2016). https://doi.org/10.1038/bmt.2015.217
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2015.217
This article is cited by
-
One novel ACOT7–NPHP4 fusion gene identified in one patient with acute lymphoblastic leukemia: a case report
BMC Medical Genomics (2022)
-
MRD in ALL: Optimization and Innovations
Current Hematologic Malignancy Reports (2022)
-
Machine learning-aided risk stratification in Philadelphia chromosome-positive acute lymphoblastic leukemia
Biomarker Research (2021)
-
A new pre-emptive TKIs strategy for preventing relapse based on BCR/ABL monitoring for Ph+ALL undergoing allo-HCT: a prospective clinical cohort study
Leukemia (2021)
-
Minimal residual disease (MRD) positivity at allogeneic hematopoietic cell transplantation, not the quantity of MRD, is a risk factor for relapse of Philadelphia chromosome-positive acute lymphoblastic leukemia
International Journal of Hematology (2021)