Abstract
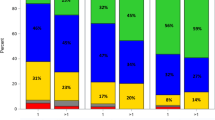
We investigated the prognostic relevance of IKZF1 deletions in 118 adult Ph-positive ALL patients who had minimal residual disease (MRD) data under a uniform treatment of allo-SCT following first-line imatinib-based chemotherapy. IKZF1 deletions were identified in 93 patients (78.8%). IKZF1-deleted patients had a lower proportion of early-stable molecular responders compared with wild-type patients (28.0 vs 56.0%, P=0.028). After a median follow-up of 72 months, IKZF1-deleted patients had a trend for higher cumulative incidence of relapse (CIR) (38.0 vs 13.3%, P=0.052), particularly in a subgroup of early-stable molecular responders (n=40; 21.4 vs 0%, P=0.088), but comparable disease-free survival to wild-type patients. Patients with biallelic-null deletions showed higher CIR (74.6 vs 13.3%, P=0.003) and lower disease-free survival (20.0 vs 67.5%, P=0.022) than wild-type patients. In multivariate analysis, MRD kinetics were closely related to outcomes, while neither IKZF1 deletions nor their functional subtypes retained an independent statistical power. Within the limitation of sample size, however, considering both the negative impact of IKZF1 deletions on MRD kinetics and a trend for relationship between IKZF1 deletions and relapse in early-stable molecular responders, IKZF1 deletions may have a potentially additive effect on unfavorable prognosis in a specific MRD-based subgroup of adult Ph-positive ALL transplants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Thomas DA, Faderl S, Cortes J, O'Brien S, Giles FJ, Kornblau SM et al. Treatment of Philadelphia chromosome-positive acute lymphocytic leukemia with hyper-CVAD and imatinib mesylate. Blood 2004; 103: 4396–4407.
Lee S, Kim YJ, Min CK, Kim HJ, Eom KS, Kim DW et al. The effect of first-line imatinib interim therapy on the outcome of allogeneic stem cell transplantation in adults with newly diagnosed Philadelphia chromosome-positive acute lymphoblastic leukemia. Blood 2005; 105: 3449–3457.
Yanada M, Takeuchi J, Sugiura I, Akiyama H, Usui N, Yagasaki F et al. High complete remission rate and promising outcome by combination of imatinib and chemotherapy for newly diagnosed BCR-ABL-positive acute lymphoblastic leukemia: a phase II study by the Japan Adult Leukemia Study Group. J Clin Oncol 2006; 24: 460–466.
Wassmann B, Pfeifer H, Goekbuget N, Beelen DW, Beck J, Stelljes M et al. Alternating versus concurrent schedules of imatinib and chemotherapy as front-line therapy for Philadelphia-positive acute lymphoblastic leukemia (Ph+ ALL). Blood 2006; 108: 1469–1477.
de Labarthe A, Rousselot P, Huguet-Rigal F, Delabesse E, Witz F, Maury S et al. Imatinib combined with induction or consolidation chemotherapy in patients with de novo Philadelphia chromosome-positive acute lymphoblastic leukemia: results of the GRAAPH-2003 study. Blood 2007; 109: 1408–1413.
Bassan R, Rossi G, Pogliani EM, Di Bona E, Angelucci E, Cavattoni I et al. Chemotherapy-phased imatinib pulses improve long-term outcome of adult patients with Philadelphia chromosome-positive acute lymphoblastic leukemia: Northern Italy Leukemia Group protocol 09/00. J Clin Oncol 2010; 28: 3644–3652.
Ribera JM, Oriol A, González M, Vidriales B, Brunet S, Esteve J et al. Concurrent intensive chemotherapy and imatinib before and after stem cell transplantation in newly diagnosed Philadelphia chromosome-positive acute lymphoblastic leukemia. Final results of the CSTIBES02 trial. Haematologica 2010; 95: 87–95.
Fielding AK, Rowe JM, Buck G, Foroni L, Gerrard G, Litzow MR et al. UKALLXII/ECOG2993: addition of imatinib to a standard treatment regimen enhances long-term outcomes in Philadelphia positive acute lymphoblastic leukemia. Blood 2014; 123: 843–850.
Ravandi F, O'Brien S, Thomas D, Faderl S, Jones D, Garris R et al. First report of phase 2 study of dasatinib with hyper-CVAD for the frontline treatment of patients with Philadelphia chromosome-positive (Ph+) acute lymphoblastic leukemia. Blood 2010; 116: 2070–2077.
Foà R, Vitale A, Vignetti M, Meloni G, Guarini A, De Propris MS et al. Dasatinib as first-line treatment for adult patients with Philadelphia chromosome-positive acute lymphoblastic leukemia. Blood 2011; 118: 6521–6528.
Yanada M, Sugiura I, Takeuchi J, Akiyama H, Maruta A, Ueda Y et al. Prospective monitoring of BCR-ABL1 transcript levels in patients with Philadelphia chromosome-positive acute lymphoblastic leukaemia undergoing imatinib-combined chemotherapy. Br J Haematol 2008; 143: 503–510.
Tanguy-Schmidt A, Rousselot P, Chalandon Y, Cayuela JM, Hayette S, Vekemans MC et al. Long-term follow-up of the imatinib GRAAPH-2003 study in newly diagnosed patients with de novo Philadelphia chromosome-positive acute lymphoblastic leukemia: a GRAALL study. Biol Blood Marrow Transplant 2013; 19: 150–155.
Ravandi F, Jorgensen JL, Thomas DA, O'Brien S, Garris R, Faderl S et al. Detection of MRD may predict the outcome of patients with Philadelphia chromosome-positive ALL treated with tyrosine kinase inhibitors plus chemotherapy. Blood 2013; 122: 1214–1221.
Lee S, Kim YJ, Chung NG, Lim J, Lee DG, Kim HJ et al. The extent of minimal residual disease reduction after the first 4-week imatinib therapy determines outcome of allogeneic stem cell transplantation in adults with Philadelphia chromosome-positive acute lymphoblastic leukemia. Cancer 2009; 115: 561–570.
Lee S, Kim DW, Cho BS, Yoon JH, Shin SH, Yahng SA et al. Impact of minimal residual disease kinetics during imatinib-based treatment on transplantation outcome in Philadelphia chromosome-positive acute lymphoblastic leukemia. Leukemia 2012; 26: 2367–2374.
Mullighan CG, Goorha S, Radtke I, Miller CB, Coustan-Smith E, Dalton JD et al. Genome-wide analysis of genetic alterations in acute lymphoblastic leukaemia. Nature 2007; 446: 758–764.
Kuiper RP, Schoenmakers EF, van Reijmersdal SV, Hehir-Kwa JY, van Kessel AG, van Leeuwen FN et al. High-resolution genomic profiling of childhood ALL reveals novel recurrent genetic lesions affecting pathways involved in lymphocyte differentiation and cell cycle progression. Leukemia 2007; 21: 1258–1266.
Kawamata N, Ogawa S, Zimmermann M, Kato M, Sanada M, Hemminki K et al. Molecular allelokaryotyping of pediatric acute lymphoblastic leukemias by high-resolution single nucleotide polymorphism oligonucleotide genomic microarray. Blood 2008; 111: 776–784.
Mullighan CG, Miller CB, Radtke I, Phillips LA, Dalton J, Ma J et al. BCR-ABL1 lymphoblastic leukaemia is characterized by the deletion of Ikaros. Nature 2008; 453: 110–114.
Iacobucci I, Lonetti A, Cilloni D, Messa F, Ferrari A, Zuntini R et al. Identification of different Ikaros cDNA transcripts in Philadelphia-positive adult acute lymphoblastic leukemia by a high-throughput capillary electrophoresis sizing method. Haematologica 2008; 93: 1814–1821.
Iacobucci I, Lonetti A, Messa F, Cilloni D, Arruga F, Ottaviani E et al. Expression of spliced oncogenic Ikaros isoforms in Philadelphia-positive acute lymphoblastic leukemia patients treated with tyrosine kinase inhibitors: implications for a new mechanism of resistance. Blood 2008; 112: 3847–3855.
Iacobucci I, Storlazzi CT, Cilloni D, Lonetti A, Ottaviani E, Soverini S et al. Identification and molecular characterization of recurrent genomic deletions on 7p12 in the IKZF1 gene in a large cohort of BCR-ABL1-positive acute lymphoblastic leukemia patients: on behalf of Gruppo Italiano Malattie Ematologiche dell'Adulto Acute Leukemia Working Party (GIMEMA AL WP). Blood 2009; 114: 2159–2167.
Den Boer ML, van Slegtenhorst M, De Menezes RX, Cheok MH, Buijs-Gladdines JG, Peters ST et al. A subtype of childhood acute lymphoblastic leukaemia with poor treatment outcome: a genome-wide classification study. Lancet Oncol 2009; 10: 125–134.
Iacobucci I, Iraci N, Messina M, Lonetti A, Chiaretti S, Valli E et al. IKAROS deletions dictate a unique gene expression signature in patients with adult B-cell acute lymphoblastic leukemia. PLoS ONE 2012; 7: e40934.
Dupuis A, Gaub MP, Legrain M, Drenou B, Mauvieux L, Lutz P et al. Biclonal and biallelic deletions occur in 20% of B-ALL cases with IKZF1 mutations. Leukemia 2013; 27: 503–507.
Mullighan CG, Su X, Zhang J, Radtke I, Phillips LA, Miller CB et al. Deletion of IKZF1 and prognosis in acute lymphoblastic leukemia. N Engl J Med 2009; 360: 470–480.
Kuiper RP, Waanders E, van der Velden VH, van Reijmersdal SV, Venkatachalam R, Scheijen B et al. IKZF1 deletions predict relapse in uniformly treated pediatric precursor B-ALL. Leukemia 2010; 24: 1258–1264.
Yang YL, Hung CC, Chen JS, Lin KH, Jou ST, Hsiao CC et al. IKZF1 deletions predict a poor prognosis in children with B-cell progenitor acutelymphoblastic leukemia: a multicenter analysis in Taiwan. Cancer Sci 2011; 102: 1874–1881.
Chen IM, Harvey RC, Mullighan CG, Gastier-Foster J, Wharton W, Kang H et al. Outcome modeling with CRLF2, IKZF1, JAK, and minimal residual disease in pediatric acute lymphoblastic leukemia: a Children's Oncology Group study. Blood 2012; 119: 3512–3522.
Dörge P, Meissner B, Zimmermann M, Möricke A, Schrauder A, Bouquin JP et al. IKZF1 deletion is an independent predictor of outcome in pediatric acute lymphoblastic leukemia treated according to the ALL-BFM 2000 protocol. Haematologica 2013; 98: 428–432.
van der Veer A, Waanders E, Pieters R, Willemse ME, Van Reijmersdal SV, Russell LJ et al. Independent prognostic value of BCR-ABL1-like signature and IKZF1 deletion, but not high CRLF2 expression, in children with B-cell precursor ALL. Blood 2013; 122: 2622–2629.
Cho BS, Lee S, Kim YJ, Chung NG, Eom KS, Kim HJ et al. Reduced-intensity conditioning allogeneic stem cell transplantation is a potential therapeutic approach for adults with high-risk acute lymphoblastic leukemia in remission: results of a prospective phase 2 study. Leukemia 2009; 23: 1763–1770.
Lee S, Chung NG, Cho BS, Eom KS, Kim YJ, Kim HJ et al. Donor-specific differences in long-term outcomes of myeloablative transplantation in adults with Philadelphia-negative acute lymphoblastic leukemia. Leukemia 2010; 24: 2110–2119.
Eom KS, Shin SH, Yoon JH, Yahng SA, Lee SE, Cho BS et al. Comparable long-term outcomes after reduced-intensity conditioning versus myeloablative conditioning allogeneic stem cell transplantation for adult high-risk acute lymphoblastic leukemia in complete remission. Am J Hematol 2013; 88: 634–641.
Shin SH, Yoon JH, Yahng SA, Lee SE, Cho BS, Eom KS et al. PBSC vs BM grafts with myeloablative conditioning for unrelated donor transplantation in adults with high-risk ALL. Bone Marrow Transplant 2014; 49: 773–779.
van der Veer A, Zaliova M, Mottadelli F, De Lorenzo P, Te Kronnie G, Harrison CJ et al. IKZF1 status as a prognostic feature in BCR-ABL1-positive childhood ALL. Blood 2014; 123: 1691–1698.
Martinelli G, Iacobucci I, Storlazzi CT, Vignetti M, Paoloni F, Cilloni D et al. IKZF1 (Ikaros) deletions in BCR-ABL1-positive acute lymphoblastic leukemia are associated with short disease-free survival and high rate of cumulative incidence of relapse: a GIMEMA AL WP report. J Clin Oncol 2009; 27: 5202–5207.
Waanders E, van der Velden VH, van der Schoot CE, van Leeuwen FN, van Reijmersdal SV, de Haas V et al. Integrated use of minimal residual disease classification and IKZF1 alteration status accurately predicts 79% of relapses in pediatric acute lymphoblastic leukemia. Leukemia 2011; 25: 254–258.
Moorman AV, Schwab C, Ensor HM, Russell LJ, Morrison H, Jones L et al. IGH@ translocations, CRLF2 deregulation, and microdeletions in adolescents and adults with acute lymphoblastic leukemia. J Clin Oncol 2012; 30: 3100–3108.
Acknowledgements
This study was supported by a grant of the Korea Health technology R&D Project, Ministry of Health & Welfare, Republic of Korea (A120175). Statistical analyses performed in this article were advised by the Catholic Medical Center Clinical Research Coordinating Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kim, M., Park, J., Kim, DW. et al. Impact of IKZF1 deletions on long-term outcomes of allo-SCT following imatinib-based chemotherapy in adult Philadelphia chromosome-positive ALL. Bone Marrow Transplant 50, 354–362 (2015). https://doi.org/10.1038/bmt.2014.281
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2014.281
This article is cited by
-
Dominant-negative type of IKZF1 deletion showed a favorable prognosis in adult B-cell acute lymphoblastic leukemia
Annals of Hematology (2023)
-
Genetic correlates in patients with Philadelphia chromosome-positive acute lymphoblastic leukemia treated with Hyper-CVAD plus dasatinib or ponatinib
Leukemia (2022)
-
Comparative study on allogeneic with autologous hematopoietic stem cell transplantation in adult patients with Philadelphia chromosome–positive acute lymphoblastic leukemia in the era of TKIs: a systematic review and meta-analysis
Annals of Hematology (2020)
-
Prognostic significance of IKZF1 deletion in adult B cell acute lymphoblastic leukemia: a meta-analysis
Annals of Hematology (2017)