Abstract
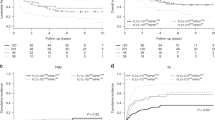
Emerging molecular studies have identified a subgroup of patients with unfavorable core-binding factor-positive (CBF)-AML who should be treated by intensified post-remission treatments. We analyzed 264 adults with CBF-AML from 2002 to 2011, and focused on 206 patients who achieved CR after standard ‘3+7’ induction chemotherapy. Patients who achieved CR with an available donor were treated with allogeneic hematopoietic SCT (allo-HSCT, n=115) and the rest were treated with autologous (auto) HSCT (n=72) or chemotherapy alone (n=19). OS was not significantly different between CBFβ/MYH11 (n=62) and RUNX1/RUNX1T1 (n=144), and auto-HSCT showed favorable OS compared with allo-HSCT or chemotherapy alone. Cytogenetic analysis identified that inv(16) without trisomy had a favorable OS and t(8;21) with additional chromosomes had an unfavorable OS, but multivariate analysis revealed those were NS. Patients with c-kit mutation showed inferior OS. For transplanted patients, residual post-transplant CBF-minimal residual disease quantitative PCR with higher WT1 expression at D+60 showed the worst OS with a higher incidence of relapse. Conclusively, we found that unfavorable CBF-AML can be defined with risk stratification using cytogenetic and molecular studies, and a careful risk-adapted treatment approach using frontline transplantation with novel therapies should be evaluated for this particular risk subgroup.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children's Leukaemia Working Parties. Blood 1998; 92: 2322–2333.
Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, Mohamed A et al. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood 2000; 96: 4075–4083.
Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood 2010; 116: 354–365.
O'Donnell MR, Abboud CN, Altman J, Appelbaum FR, Arber DA, Attar E et al. Acute myeloid leukemia. J Natl Compr Canc Netw 2012; 10: 984–1021.
Kurosawa S, Yamaguchi T, Miyawaki S, Uchida N, Sakura T, Kanamori H et al. Prognostic factors and outcomes of adult patients with acute myeloid leukemia after first relapse. Haematologica 2010; 95: 1857–1864.
Schlenk RF, Benner A, Krauter J, Buchner T, Sauerland C, Ehninger G et al. Individual patient data-based meta-analysis of patients aged 16 to 60 years with core binding factor acute myeloid leukemia: a survey of the German Acute Myeloid Leukemia Intergroup. J Clin Oncol 2004; 22: 3741–3750.
Appelbaum FR, Kopecky KJ, Tallman MS, Slovak ML, Gundacker HM, Kim HT et al. The clinical spectrum of adult acute myeloid leukaemia associated with core binding factor translocations. Br J Haematol 2006; 135: 165–173.
Marcucci G, Mrozek K, Ruppert AS, Maharry K, Kolitz JE, Moore JO et al. Prognostic factors and outcome of core binding factor acute myeloid leukemia patients with t(8;21) differ from those of patients with inv(16): a Cancer and Leukemia Group B study. J Clin Oncol 2005; 23: 5705–5717.
Billstrom R, Ahlgren T, Bekassy AN, Malm C, Olofsson T, Hoglund M et al. Acute myeloid leukemia with inv(16)(p13q22): involvement of cervical lymph nodes and tonsils is common and may be a negative prognostic sign. Am J Hematol 2002; 71: 15–19.
Markova J, Trnkova Z, Michkova P, Maaloufova J, Stary J, Cetkovsky P et al. Monitoring of minimal residual disease in patients with core binding factor acute myeloid leukemia and the impact of C-KIT, FLT3, and JAK2 mutations on clinical outcome. Leuk Lymphoma 2009; 50: 1448–1460.
Park SH, Chi HS, Min SK, Park BG, Jang S, Park CJ Prognostic impact of c-KIT mutations in core binding factor acute myeloid leukemia. Leuk Res 2011; 35: 1376–1383.
Schnittger S, Kohl TM, Haferlach T, Kern W, Hiddemann W, Spiekermann K et al. KIT-D816 mutations in AML1-ETO-positive AML are associated with impaired event-free and overall survival. Blood 2006; 107: 1791–1799.
Care RS, Valk PJ, Goodeve AC, Abu-Duhier FM, Geertsma-Kleinekoort WM, Wilson GA et al. Incidence and prognosis of c-KIT and FLT3 mutations in core binding factor (CBF) acute myeloid leukaemias. Br J Haematol 2003; 121: 775–777.
Cairoli R, Beghini A, Grillo G, Nadali G, Elice F, Ripamonti CB et al. Prognostic impact of c-KIT mutations in core binding factor leukemias: an Italian retrospective study. Blood 2006; 107: 3463–3468.
Kim HJ, Ahn HK, Jung CW, Moon JH, Park CH, Lee KO et al. KIT D816 mutation associates with adverse outcomes in core binding factor acute myeloid leukemia, especially in the subgroup with RUNX1/RUNX1T1 rearrangement. Ann Hematol 2013; 92: 163–171.
Medeiros BC, Othus M, Fang M, Appelbaum FR, Estey EH Impact of residual normal metaphases in core binding factor acute myeloid leukemia. Cancer 2012; 118: 2420–2423.
Delaunay J, Vey N, Leblanc T, Fenaux P, Rigal-Huguet F, Witz F et al. Prognosis of inv(16)/t(16;16) acute myeloid leukemia (AML): a survey of 110 cases from the French AML Intergroup. Blood 2003; 102: 462–469.
Yin JA, O'Brien MA, Hills RK, Daly SB, Wheatley K, Burnett AK Minimal residual disease monitoring by quantitative RT–PCR in core binding factor AML allows risk stratification and predicts relapse: results of the United Kingdom MRC AML-15 trial. Blood 2012; 120: 2826–2835.
Yoon JH, Kim HJ, Shin SH, Yahng SA, Lee SE, Cho BS et al. BAALC and WT1 expressions from diagnosis to hematopoietic stem cell transplantation: consecutive monitoring in adult patients with core-binding-factor-positive AML. Eur J Haematol 2013; 91: 112–121.
Shaffer LG Slovak ML Campbell LJ . ISCN: An International System for Human Cytogenetic Nomenclature. S Krager: Basel, Switzerland, 2009.
Yoon JH, Kim HJ, Shin SH, Yahng SA, Cho BS, Eom KS et al. Normal karyotype mosaicism in adult AML patients with adverse-risk and undefined karyotype: preliminary report of treatment outcomes after hematopoietic stem cell transplantation. Int J Hematol 2013; 97: 773–781.
Yoon JH, Kim HJ, Shin SH, Yahng SA, Lee SE, Cho BS et al. Serial measurement of WT1 expression and decrement ratio until hematopoietic cell transplantation as a marker of residual disease in patients with cytogenetically normal acute myelogenous leukemia. Biol Blood Marrow Transplant 2013; 19: 958–966.
Park HS, Kim DW, Kim CC, Kim HK, Kim JS, Hwang TJ et al. Induction chemotherapy with idarubicin plus N4-behenoyl-1-beta-D-arabinofuranosylcytosine in acute myelogenous leukemia: a newly designed induction regimen—a prospective, cooperative multicenter study. Semin hematol 1996; 33: 24–29.
Kim HJ, Min WS, Eom KS, Park SJ, Park YH, Kim DW et al. Autologous stem cell transplantation using modified TAM or combination of triple-alkylating agents conditioning regimens as one of the post-remission treatments in patients with adult acute myeloid leukemia in first complete remission. Bone Marrow Transplant 2004; 34: 215–220.
Gray RJ A class of k-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 1988; 16: 1141–1154.
Shin HJ, Kim HJ, Sohn SK, Min YH, Won JH, Kim I et al. Re-analysis of the outcomes of post-remission therapy for acute myeloid leukemia with core binding factor according to years of patient enrollment. Jpn J Clin Oncol 2010; 40: 556–566.
Kurosawa S, Miyawaki S, Yamaguchi T, Kanamori H, Sakura T, Moriuchi Y et al. Prognosis of patients with core binding factor acute myeloid leukemia after first relapse. Haematologica 2013; 98: 1525–1531.
Peniket A, Wainscoat J, Side L, Daly S, Kusec R, Buck G et al. Del (9q) AML: clinical and cytological characteristics and prognostic implications. Br J Haematol 2005; 129: 210–220.
Raanani P, Ben-Bassat I Detection of minimal residual disease in acute myelogenous leukemia. Acta Haematol 2004; 112: 40–54.
Marcucci G, Livak KJ, Bi W, Strout MP, Bloomfield CD, Caligiuri MA Detection of minimal residual disease in patients with AML1/ETO-associated acute myeloid leukemia using a novel quantitative reverse transcription polymerase chain reaction assay. Leukemia 1998; 12: 1482–1489.
Cilloni D, Renneville A, Hermitte F, Hills RK, Daly S, Jovanovic JV et al. Real-time quantitative polymerase chain reaction detection of minimal residual disease by standardized WT1 assay to enhance risk stratification in acute myeloid leukemia: a European LeukemiaNet study. J Clin Oncol 2009; 27: 5195–5201.
Cilloni D, Gottardi E, De Micheli D, Serra A, Volpe G, Messa F et al. Quantitative assessment of WT1 expression by real time quantitative PCR may be a useful tool for monitoring minimal residual disease in acute leukemia patients. Leukemia 2002; 16: 2115–2121.
Weisser M, Kern W, Rauhut S, Schoch C, Hiddemann W, Haferlach T et al. Prognostic impact of RT–PCR-based quantification of WT1 gene expression during MRD monitoring of acute myeloid leukemia. Leukemia 2005; 19: 1416–1423.
Kim HJ, Choi EJ, Sohn HJ, Park SH, Min WS, Kim TG Combinatorial molecular marker assays of WT1, survivin, and TERT at initial diagnosis of adult acute myeloid leukemia. Eur J Haematol 2013; 91: 411–422.
Hashii Y, Sato-Miyashita E, Matsumura R, Kusuki S, Yoshida H, Ohta H et al. WT1 peptide vaccination following allogeneic stem cell transplantation in pediatric leukemic patients with high risk for relapse: successful maintenance of durable remission. Leukemia 2012; 26: 530–532.
Tsuboi A, Oka Y, Kyo T, Katayama Y, Elisseeva OA, Kawakami M et al. Long-term WT1 peptide vaccination for patients with acute myeloid leukemia with minimal residual disease. Leukemia 2012; 26: 1410–1413.
Kim YJ, Cho SG, Lee S, Kim MS, Kim EK, Cho BS et al. Potential role of adoptively transferred allogeneic WT1-specific CD4+ and CD8+ T lymphocytes for the sustained remission of refractory AML. Bone Marrow Transplant 2010; 45: 597–599.
Brandwein JM, Hedley DW, Chow S, Schimmer AD, Yee KW, Schuh AC et al. A phase I/II study of imatinib plus reinduction therapy for c-kit-positive relapsed/refractory acute myeloid leukemia: inhibition of Akt activation correlates with complete response. Leukemia 2011; 25: 945–952.
Advani AS, Tiu R, Saunthararajah Y, Maciejewski J, Copelan EA, Sobecks R et al. A Phase 1 study of imatinib mesylate in combination with cytarabine and daunorubicin for c-kit positive relapsed acute myeloid leukemia. Leuk Res 2010; 34: 1622–1626.
Nanri T, Matsuno N, Kawakita T, Mitsuya H, Asou N Imatinib mesylate for refractory acute myeloblastic leukemia harboring inv(16) and a C-KIT exon 8 mutation. Leukemia 2005; 19: 1673–1675.
Fischer T, Stone RM, Deangelo DJ, Galinsky I, Estey E, Lanza C et al. Phase IIB trial of oral Midostaurin (PKC412), the FMS-like tyrosine kinase 3 receptor (FLT3) and multi-targeted kinase inhibitor, in patients with acute myeloid leukemia and high-risk myelodysplastic syndrome with either wild-type or mutated FLT3. J Clin Oncol 2010; 28: 4339–4345.
Growney JD, Clark JJ, Adelsperger J, Stone R, Fabbro D, Griffin JD et al. Activation mutations of human c-KIT resistant to imatinib mesylate are sensitive to the tyrosine kinase inhibitor PKC412. Blood 2005; 106: 721–724.
Gotlib J, Berube C, Growney JD, Chen CC, George TI, Williams C et al. Activity of the tyrosine kinase inhibitor PKC412 in a patient with mast cell leukemia with the D816V KIT mutation. Blood 2005; 106: 2865–2870.
Kosmider O, Denis N, Dubreuil P, Moreau-Gachelin F Semaxinib (SU5416) as a therapeutic agent targeting oncogenic Kit mutants resistant to imatinib mesylate. Oncogene 2007; 26: 3904–3908.
Fiedler W, Mesters R, Tinnefeld H, Loges S, Staib P, Duhrsen U et al. A phase 2 clinical study of SU5416 in patients with refractory acute myeloid leukemia. Blood 2003; 102: 2763–2767.
Giles FJ, Stopeck AT, Silverman LR, Lancet JE, Cooper MA, Hannah AL et al. SU5416, a small molecule tyrosine kinase receptor inhibitor, has biologic activity in patients with refractory acute myeloid leukemia or myelodysplastic syndromes. Blood 2003; 102: 795–801.
Smolich BD, Yuen HA, West KA, Giles FJ, Albitar M, Cherrington JM The antiangiogenic protein kinase inhibitors SU5416 and SU6668 inhibit the SCF receptor (c-kit) in a human myeloid leukemia cell line and in acute myeloid leukemia blasts. Blood 2001; 97: 1413–1421.
Acknowledgements
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry for Health and Welfare, Republic of Korea (1020370).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Bone Marrow Transplantation website
Supplementary information
Rights and permissions
About this article
Cite this article
Yoon, JH., Kim, HJ., Kim, JW. et al. Identification of molecular and cytogenetic risk factors for unfavorable core-binding factor-positive adult AML with post-remission treatment outcome analysis including transplantation. Bone Marrow Transplant 49, 1466–1474 (2014). https://doi.org/10.1038/bmt.2014.180
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2014.180
This article is cited by
-
Autologous hematopoietic cell transplantation following high-dose cytarabine consolidation for core-binding factor-acute myeloid leukemia in first complete remission: a phase 2 prospective trial
International Journal of Hematology (2021)
-
Prognostic values of D816V KIT mutation and peri-transplant CBFB-MYH11 MRD monitoring on acute myeloid leukemia with CBFB-MYH11
Bone Marrow Transplantation (2021)
-
Different prognostic effects of core-binding factor positive AML with Korean AML registry data
Annals of Hematology (2019)
-
The dynamics of RUNX1-RUNX1T1 transcript levels after allogeneic hematopoietic stem cell transplantation predict relapse in patients with t(8;21) acute myeloid leukemia
Journal of Hematology & Oncology (2017)
-
Significance of KIT exon 17 mutation depends on mutant level rather than positivity in core-binding factor acute myeloid leukemia
Blood Cancer Journal (2016)