Abstract
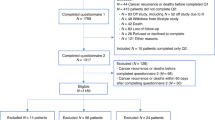
The present study examined changes in sleep quality following hematopoietic stem cell transplantation (HSCT) and investigated associations with biobehavioral factors. Individuals undergoing HSCT for hematologic malignancies (N=228) completed measures of sleep quality and psychological symptoms pre-transplant and 1, 3, 6 and 12 months post transplant. Circulating inflammatory cytokines (IL-6, TNF-α) were also assessed. Sleep quality was poorest at 1 month post transplant, improving and remaining relatively stable after 3 months post transplant. However, approximately half of participants continued to experience significant sleep disturbance at 6 and 12 months post transplant. Mixed-effects linear regression models indicated that depression and anxiety were associated with poorer sleep quality, while psychological well-being was associated with better sleep. Higher circulating levels of IL-6 were also linked with poorer sleep. Subject-level fixed effects models demonstrated that among individual participants, changes in depression, anxiety and psychological well-being were associated with corresponding changes in sleep after covarying for the effects of time since transplant. Sleep disturbance was most severe when depression and anxiety were greatest and psychological well-being was lowest. Findings indicate that sleep disturbance is a persistent problem during the year following HSCT. Patients experiencing depression or anxiety and those with elevated inflammation may be at particular risk for poor sleep.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Pidala J, Anasetti C, Jim H . Quality of life after allogeneic hematopoietic cell transplantation. Blood 2009; 114: 7–19.
Bush NE, Donaldson GW, Haberman MH, Dacanay R, Sullivan KM . Conditional and unconditional estimation of multidimensional quality of life after hematopoietic stem cell transplantation: a longitudinal follow-up of 415 patients. Biol Blood Marrow Transplant 2000; 6: 576–591.
Gruber U, Fegg M, Buchmann M, Kolb HJ, Hiddemann W . The long-term psychosocial effects of haematopoietic stem cell transplantation. Eur J Cancer Care (Engl) 2003; 12: 249–256.
Edman L, Larsen J, Hagglund H, Gardulf A . Health-related quality of life, symptom distress and sense of coherence in adult survivors of allogeneic stem-cell transplantation. Eur J Cancer Care (Engl) 2001; 10: 124–130.
Boonstra L, Harden K, Jarvis S, Palmer S, Kavanaugh-Carveth P, Barnett J et al. Sleep disturbance in hospitalized recipients of stem cell transplantation. Clin J Oncol Nurs 2011; 15: 271–276.
Bush NE, Haberman M, Donaldson G, Sullivan KM . Quality of life of 125 adults surviving 6-18 years after bone marrow transplantation. Soc Sci Med 1995; 40: 479–490.
Andrykowski MA, Carpenter JS, Greiner CB, Altmaier EM, Burish TG, Antin JH et al. Energy level and sleep quality following bone marrow transplantation. Bone Marrow Transplant 1997; 20: 669–679.
Rischer J, Scherwath A, Zander AR, Koch U, Schulz-Kindermann F . Sleep disturbances and emotional distress in the acute course of hematopoietic stem cell transplantation. Bone Marrow Transplant 2009; 44: 121–128.
Andrykowski MA, Bishop MM, Hahn EA, Cella DF, Beaumont JL, Brady MJ et al. Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. J Clin Oncol 2005; 23: 599–608.
Illescas-Rico R, Amaya-Ayala F, Jimenez-Lopez JL, Caballero-Mendez ME, Gonzalez-Llaven J . Increased incidence of anxiety and depression during bone marrow transplantation. Arch Med Res 2002; 33: 144–147.
Syrjala KL, Chapko MK, Vitaliano PP, Cummings C, Sullivan KM . Recovery after allogeneic marrow transplantation: prospective study of predictors of long-term physical and psychosocial functioning. Bone Marrow Transplant 1993; 11: 319–327.
Flynn KE, Shelby RA, Mitchell SA, Fawzy MR, Hardy NC, Husain AM et al. Sleep-wake functioning along the cancer continuum: focus group results from the Patient-Reported Outcomes Measurement Information System (PROMIS). Psychooncology 2009; 19: 1086–1093.
Association AP. Diagnostic and statistical manual of mental disorders. Washington, DC 46: 2095–2098.
Ohayon MM . Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev 2002; 6: 97–111.
Mystakidou K, Parpa E, Tsilika E, Gennatas C, Galanos A, Vlahos L . How is sleep quality affected by the psychological and symptom distress of advanced cancer patients? Palliat Med 2009; 23: 46–53.
Bourdet C, Goldenberg F . Insomnia in anxiety: sleep EEG changes. J Psychosom Res 1994; 38 (Suppl 1): 93–104.
Spira AP, Friedman L, Aulakh JS, Lee T, Sheikh JI, Yesavage JA . Subclinical anxiety symptoms, sleep, and daytime dysfunction in older adults with primary insomnia. J Geriatr Psychiatry Neurol 2008; 21: 149–153.
Delgado-Guay M, Yennurajalingam S, Parsons H, Palmer JL, Bruera E . Association between self-reported sleep disturbance and other symptoms in patients with advanced cancer. J Pain Symptom Manage 2011; 41: 819–827.
Miller AH, Ancoli-Israel S, Bower JE, Capuron L, Irwin MR . Neuroendocrine-immune mechanisms of behavioral comorbidities in patients with cancer. J Clin Oncol 2008; 26: 971–982.
Opp MR . Cytokines and sleep. Sleep Med Rev 2005; 9: 355–364.
Liu L, Mills PJ, Rissling M, Fiorentino L, Natarajan L, Dimsdale JE et al. Fatigue and sleep quality are associated with changes in inflammatory markers in breast cancer patients undergoing chemotherapy. Brain Behav Immun 2012; 26: 706–713.
Sprod LK, Palesh OG, Janelsins MC, Peppone LJ, Heckler CE, Adams MJ et al. Exercise, sleep quality, and mediators of sleep in breast and prostate cancer patients receiving radiation therapy. Community Oncol 2010; 7: 463–471.
Wang XS, Shi Q, Williams LA, Cleeland CS, Mobley GM, Reuben JM et al. Serum interleukin-6 predicts the development of multiple symptoms at nadir of allogeneic hematopoietic stem cell transplantation. Cancer 2008; 113: 2102–2109.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ . The Pittsburgh Sleep Quality Index: A new instrument for psychiatric research and practice. Psychiatry Res 1989; 28: 193–213.
Carpenter JS, Andrykowski MA . Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res 1998; 45 (1 Spec No): 5–13.
Watson D, O'Hara MW, Simms LJ, Kotov R, Chmielewski M, McDade-Montez EA et al. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS). Psychol Assess 2007; 19: 253–268.
McDade-Montez EA, Watson D . Examining the potential influence of diabetes on depression and anxiety symptoms via multiple sample confirmatory factor analysis. Ann Behav Med 2011; 42: 341–351.
Nylen KJ, Williamson JA, O'Hara MW, Watson D, Engeldinger J . Validity of somatic symptoms as indicators of depression in pregnancy. Arch Womens Ment Health 2013; 16: 203–210.
Collado-Hidalgo A, Bower JE, Ganz PA, Cole SW, Irwin MR . Inflammatory biomarkers for persistent fatigue in breast cancer survivors. Clin Cancer Res 2006; 12: 2759–2766.
Musselman DL, Miller AH, Porter MR, Manatunga A, Gao F, Penna S et al. Higher than normal plasma interleukin-6 concentrations in cancer patients with depression: preliminary findings. Am J Psychiatry 2001; 158: 1252–1257.
Meyers CA, Albitar M, Estey E . Cognitive impairment, fatigue, and cytokine levels in patients with acute myelogenous leukemia or myelodysplastic syndrome. Cancer 2005; 104: 788–793.
Coe CL, Love GD, Karasawa M, Kawakami N, Kitayama S, Markus HR et al. Population differences in proinflammatory biology: Japanese have healthier profiles than Americans. Brain Behav Immun 2011; 25: 494–502.
Bevans MF, Mitchell SA, Marden S . The symptom experience in the first 100 days following allogeneic hematopoietic stem cell transplantation (HSCT). Support Care Cancer 2008; 16: 1243–1254.
Cohen MZ, Rozmus CL, Mendoza TR, Padhye NS, Neumann J, Gning I et al. Symptoms and quality of life in diverse patients undergoing hematopoietic stem cell transplantation. J Pain Symptom Manage 2012; 44: 168–180.
Syrjala KL, Langer S, Abrams J, Storer B, Martin P . Physical and mental recovery after hematopoietic stem cell transplantation. Discov Med 2004; 4: 263–269.
Chao NJ, Tierney DK, Bloom JR, Long GD, Barr TA, Stallbaum BA et al. Dynamic assessment of quality of life after autologous bone marrow transplantation. Blood 1992; 80: 825–830.
Peterson MJ, Benca RM . Sleep in mood disorders. Psychiatr Clin North Am 2006; 29: 1009–1032 abstract ix.
Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord 2011; 135: 10–19.
Vgontzas AN, Fernandez-Mendoza J . Insomnia with short sleep duration: nosological, diagnostic, and treatment implications. Sleep Med Clin 2013; 8: 309–322.
Laugsand LE, Strand LB, Platou C, Vatten LJ, Janszky I . Insomnia and the risk of incident heart failure: a population study. Eur Heart J 2013; 35: 1382–1393.
Jaffer U, Wade RG, Gourlay T . Cytokines in the systemic inflammatory response syndrome: a review. HSR Proc Intensive Care Cardiovasc Anesth 2010; 2: 161–175.
Slavich GM, Way BM, Eisenberger NI, Taylor SE . Neural sensitivity to social rejection is associated with inflammatory responses to social stress. Proc Natl Acad Sci USA 2010; 107: 14817–14822.
National Comprehensive Cancer N. Distress management. Clinical practice guidelines. J Natl Compr Canc Netw 2003; 1: 344–374.
Espie CA, Fleming L, Cassidy J, Samuel L, Taylor LM, White CA et al. Randomized controlled clinical effectiveness trial of cognitive behavior therapy compared with treatment as usual for persistent insomnia in patients with cancer. J Clin Oncol 2008; 26: 4651–4658.
Neikrug AB, Rissling M, Trofimenko V, Liu L, Natarajan L, Lawton S et al. Bright light therapy protects women from circadian rhythm desynchronization during chemotherapy for breast cancer. Behav Sleep Med 2012; 10: 202–216.
Acknowledgements
This work was supported by Grants R21 CA133343 and K07 CA136966 from the National Cancer Institute to ESC, KL2 RR0205012 from the National Center for Research Resources, P30 CA014520 from the UWCCC, and an award from the Forward Lymphoma Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflicts of intrest.
Rights and permissions
About this article
Cite this article
Nelson, A., Coe, C., Juckett, M. et al. Sleep quality following hematopoietic stem cell transplantation: longitudinal trajectories and biobehavioral correlates. Bone Marrow Transplant 49, 1405–1411 (2014). https://doi.org/10.1038/bmt.2014.179
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2014.179
This article is cited by
-
Relationship between circadian activity rhythms and fatigue in hospitalized children with CNS cancers receiving high-dose chemotherapy
Supportive Care in Cancer (2020)
-
Fluctuation in physical symptoms, coping, and mood in patients following hematopoietic stem cell transplantation: assessing mediation effects using a daily diary approach
Journal of Behavioral Medicine (2019)
-
Prevalence of self-reported sleep dysfunction before allogeneic hematopoietic cell transplantation
Bone Marrow Transplantation (2018)
-
Sleep disruption among cancer patients following autologous hematopoietic cell transplantation
Bone Marrow Transplantation (2018)
-
Severity, course, and predictors of sleep disruption following hematopoietic cell transplantation: a secondary data analysis from the BMT CTN 0902 trial
Bone Marrow Transplantation (2018)