Abstract
Respiratory syncytial virus (RSV) usually causes self-limiting upper respiratory tract infections, but can be associated with severe lower respiratory tract infection disease (LRTID) in infants and in patients with hematologic malignancies. We have analyzed the risk factors and the measures for containment within an outbreak of nosocomial RSV infections in a hematology and SCT unit. A total of 56 patients were affected (53 RSV-A and 3 RSV-B) including 32 transplant patients (16 allogeneic and 16 autologous). Forty (71%) of the 56 patients suffered from LRTID and 14 (35%) of the patients with LRTID subsequently died. However, because of concomitant infections with fungal and bacterial pathogens, the impact of RSV on the fatal outcome was difficult to assess. Multivariate analysis showed that low levels of IgG were significantly associated with fatal outcome (P=0.007), treatment with oral ribavirin represented a protective factor (P=0.02). An extremely protracted viral shedding was observed in this cohort of patients (median=30.5 days, range: 1–162 days), especially pronounced in patients after allogeneic transplantation (P=0.002). Implementation of rigorous isolation and barrier measures, although challenged by long-term viral carriers, was effective in containment of the outbreak.
Similar content being viewed by others
Introduction
Respiratory syncytial virus (RSV) is an enveloped single-stranded RNA virus of the family Paramyxoviridae. It is a common pathogen in children and might induce severe lower respiratory tract infection disease (LRTID), especially in infants. Nearly all children have been infected by the age of 2, yet no lasting immunity is acquired.1 RSV is rapidly transmitted by inhalation of droplets and can stay viable for up to 6 h outside of the patient.2 The diagnostic gold standard is viral culture, however, detection of viral RNA in respiratory specimens by reverse transcription PCR represents a faster and more sensitive approach.3
Although RSV is usually a self-limiting disease causing only mild symptoms of upper respiratory tract infection disease (URTID) or no symptoms at all,4 it may be associated with severe LRTID in elderly or immunocompromised adults.5, 6 Morbidity and mortality rates reported in the literature are heterogeneous, the relevance of RSV infections in terms of outcome for patients undergoing autologous or allogeneic SCT ranging from none7, 8 to a mortality rate of up to 78%.9, 10, 11, 12, 13, 14 The impact of RSV on fatal outcome in this often multi-morbid patient population might be difficult, if not impossible, to assess. Aerosolized ribavirin is the only Food and Drug Administration-approved drug for the treatment of severe RSV infection in children.15, 16 The use of aerosolized ribavirin to treat RSV infection in adults has remained controversial and clinical trials are lacking. Even fewer data are available regarding oral ribavirin. However, a recent pooled analysis suggests some efficacy.17
Several nosocomial outbreaks of RSV infections on pediatric wards18, 19, 20 as well as in adult hematology and transplantation units13, 21, 22, 23, 24, 25 have been described in the literature.
Here we report an outbreak of nosocomial RSV infections in an oncology and SCT unit from December 2011 to March 2012, which affected a total of 56 patients. The virological aspects of this outbreak have been recently published by Geis et al.26 We now present an analysis from a clinical point of view and aim to identify risk factors for LRTID and fatal outcome, to evaluate the contribution of RSV infection to the fatal cases observed and to define strategies for management as well as containment of RSV infections in immunocompromised patients.
Materials and methods
Study site, RSV diagnostics and treatment
The medical center of the University of Heidelberg is a tertiary care referral center. The Department of Hematology–Oncology consists of two inpatient wards where normal and high-dose chemotherapy including autologous blood SCT are performed, one intensive care ward for critically ill patients not requiring mechanical ventilation and an allogeneic transplant unit. In 2011, a total of 1825 cases were treated, 227 autologous and 114 allogeneic SCTs were performed.
Before the described outbreak, screening for RSV infections was not standard and RSV was only tested for if specifically requested by the physician. Diagnosis of RSV infection was performed via reverse transcription PCR amplification of specific viral RNA in respiratory specimens, that is, nasal or throat swabs, tracheal secretions or broncho-alveolar lavage, and was characterized as either RSV-A or RSV-B. In the majority of patients, the RSV strain was further characterized by sequencing of the second variable region of the G gene. Details on reverse transcription PCR and sequencing are provided by Geis et al.26 During the outbreak, throat swabs were established as standard diagnostic material for screening purposes, being readily obtainable and practicable.
No standard treatment existed for RSV infections in adults. At the peak of the outbreak, a 2 week course of oral ribavirin in a weight adapted dosage (<65 kg body weight: 800 mg daily; 65–80 kg body weight: 1000 mg daily; >80 kg body weight: 1200 mg daily; total daily dose administered in two divided doses) was recommended for all patients, independently of the presence of LRTID. Aerosolized ribavirin was not used for safety reasons because of its suspected teratogenicity for the surroundings.27 During ribavirin therapy, patients were checked twice weekly for signs of hemolytic anemia as the major reported side-effect.28 In cases of significant hypogammaglobulinemia, patients might additionally receive polyvalent Ig preparations (0.2–0.4 g/kg body weight) at the discretion of the attending physician.
Outbreak management
RSV-infected patients were isolated in single rooms or cohort isolated. They were considered infectious until three consecutive throat swabs were tested negative covering a period of 2 weeks. Contact patients were isolated in single rooms until they tested negative at the end of the 2–8 days incubation period.29 RSV-negative inpatients were regularly screened for RSV infections. Infected patients were repeatedly retested in order to monitor viral shedding. Barrier measures were severely reinforced. Disposable gowns, gloves and filtering facepieces (FFP2) were to be worn when entering patient rooms. Health-care staff with respiratory symptoms were suspended from work until a negative RSV test was obtained.
Retrospective analysis
Charts of all RSV-infected hematologic inpatients from 1 September 2011 to 30 March 2012 were thoroughly reviewed. Patients were categorized as either asymptomatic/URTID or LRTID according to the adapted criteria by the European Centre for Disease Prevention and Control applied in the recent guidelines by the 4th European Conference on Infections in Leukaemia (ECIL-4).30 Aplasia was defined as total leukocyte count <1000/μL, hypogammaglobulinemia as polyclonal IgG <6 g/L. Time to RSV clearance was calculated from first to last positive RSV test, patients who were only tested once were excluded for analysis of this end point. Patient movements and bed occupancies were analyzed to identify a possible chain of infection.
Statistical analysis of potential risk and protective factors in regard to respiratory disease, fatal outcome and duration of RSV positivity was performed. Single risk/protective factors (delineated in Table 3) for development of LRTID as well as for fatal outcome were analyzed using univariate χ2 tests for binary variables and univariate Wilcoxon tests for continuous variables. Possible influence factors regarding duration of RSV positivity were analyzed by Kruskal–Wallis tests in the case of binary variables and by Spearman’s ρ statistics in the case of continuous variables. For multivariate analysis, a reduced set of potential influence factors was considered: age (⩾65 years versus<65 years), allogeneic versus autologous transplantation, pre-existing respiratory disease, duration of aplasia (> versus ⩽10 days), hypogammaglobulinemia and treatment with ribavirin. Penalized logistic regression models31 were adapted for the outcomes LRTID, fatal disease and RSV positivity. The outcome RSV positivity was dichotomized in > or ⩽ 1 week in the multivariate model. In all tests, P-values<0.05 were regarded as significant.
Results
Outbreak and monitoring of RSV
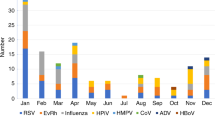
From 30 December 2011 to 22 March 2012 an outbreak of nosocomial RSV infections occurred at the Department of Hematology–Oncology of the University of Heidelberg. RSV-A RNA was detected in bronchial specimens of two patients with LRTID on two different wards on 30 December. During the first 2 weeks of January, systematic RSV screening of all inpatients and personnel was performed revealing further 16 RSV-infected patients, 14 of them with signs of LRTID and 1 infected physician out of 209 employees. Barrier measures were reinforced and elective admissions were suspended. Over the following weeks, the number of newly diagnosed RSV infections decreased with the last infection occurring on 22 March.
Systematic review of virological test results as well as retrospective tests of stored respiratory specimens identified 10 patients with RSV infection before the recognition of the outbreak (2 in November and 8 in December), 1 of them was infected as early as 12 November. Retrospectively, this might represent the actual index case. In summary, 56 inpatients were diagnosed with RSV infection from November 2011 to March 2012, 53 with RSV-A and 3 with RSV-B.
The strict criteria of a nosocomial case, that is, diagnosis of RSV infection ⩾3 days after hospital admission taking into account the 2–8 days incubation period,29 were met by 40 patients. However, a further eight patients had a prior stay on one of the hematologic wards or were treated at the chemotherapy day care unit within 4 weeks of the recent admission. A timeline of new cases is given in Figure 1.
Morbidity and mortality
A total of 16 of the 56 RSV-infected patients were asymptomatic or showed only minor signs of URTID. Forty patients developed a LRTID, 13 of them had progressed from prior URTID, whereas 27 had already symptoms of LRTID at the time of RSV diagnosis. The patients’ characteristics are summarized in Table 1. Oral ribavirin was administered to 36 patients. Treatment with oral ribavirin was generally well tolerated and no side effects requiring medical intervention or dose reduction were observed. At the discretion of the attending physician, 14 patients received i.v. Ig preparations in addition.
Of all RSV-infected patients, 32 underwent SCT (16 allogeneic and 16 autologous). RSV infection was diagnosed in 24 patients after engraftment, 8 patients were infected during aplasia. The median time to leukocyte recovery (that is, leukocytes >1000/μL) was 13.5 days (range 0–27) and 14.5 days (range 10–47) for post- and pre-engraftment infected patients, respectively.
Among the 40 patients with LRTID, 14 patients died 1 to 134 days (median 15 days) after diagnosis of RSV. Six underwent SCT (three allogeneic and three autologous), two of them were infected before engraftment. Concomitant infections with fungal, bacterial and other viral pathogens were present in 11 patients. In addition, a high proportion of these patients suffered from advanced, resistant disease or from severe comorbidities such as steroid-refractory GVHD. The details are delineated in Table 2. At the time of death, one patient had already cleared the virus (that is, tested repeatedly negative) but still required mechanical ventilation and two tested negative once.
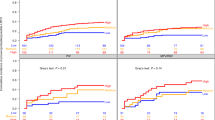
We have performed a retrospective analysis to determine if the development of LRTID as well as fatal outcome was associated with any of an extensive list of possible influence factors. Univariate analysis showed that duration of aplasia was significantly associated with development of LRTID (P=0.0001). Hypogammaglobulinemia was a significant risk factor for fatal outcome (P=0.03), whereas therapy with ribavirin was a protective factor (P=0.02). Details of univariate analysis are given in Table 3.
Multivariate analysis confirmed hypogammaglobulinemia to be a risk factor (P=0.007) and treatment with ribavirin a protective factor against fatal outcome (P=0.02). In addition, a negative trend for fatal outcome was seen for pre-existing respiratory disease (P=0.08). Age and transplant status remained without significant influence. In regard to development of LRTID, no factor reached statistical significance, but a trend was seen for aplasia >10 days (P=0.08). For details on multivariate analysis refer to Table 4.
An extensively protracted viral shedding was noted in this group of patients. The median duration of positive RSV detection using PCR was 30.5 days (range: 1–162 days) in 51 patients who were tested at least twice. The risk factors that were significantly associated with duration of RSV positivity in univariate analysis were hypogammaglobulinemia (P=0.01) and allogeneic transplantation (P=0.04). In multivariate analysis, allogeneic transplantation correlated significantly (P=0.002) with duration of RSV positivity by >1 week. Interestingly, therapy with ribavirin was also associated with prolonged viral shedding (P=0.01). Details of multivariate analysis are given in Table 5.
Discussion
This is the largest outbreak of RSV infections documented in the literature, affecting a total of 56 patients. Several smaller outbreaks have been reported from adult hematology or transplant units13, 21, 22, 23, 24, 25 as well as from pediatric wards and neonatal intensive care units.18, 19, 20 A unique aspect of this retrospective analysis was the fact that all inpatients were repeatedly screened for the presence of RSV infection. In addition, retrospective analysis of stored respiratory specimens covering a time period of over 6 months was performed enabling us to provide a detailed and comprehensive review of the outbreak. Systematic analysis of risk factors in this special cohort of patients revealed hypogammaglobulinemia to be a significant risk factor for RSV-associated morbidity and mortality, whereas treatment with oral ribavirin might provide a protective effect. Protracted viral shedding was frequently observed, especially affecting patients after allogeneic transplantation.
We have shown that RSV is highly contagious—especially among immunocompromised patients and direct patient-to-patient contact was revealed as the most likely chain of infection. In all, 95% of cases were infected with RSV-A. Sequence analysis of the RSV G-protein was performed in some patients infected with RSV-A and showed by the majority an identical virus strain type GA2.26
Univariate and multivariate analysis showed that hypogammaglobulinemia was a significant risk factor for fatal outcome. However, treatment with polyvalent Ig preparations was not able to reverse this association. In contrast, treatment with ribavirin had a significant impact on mortality. Pre-existing pulmonary conditions might also have an influence but the difference was statistically not significant.
In a retrospective analysis, Khanna et al.32 reported that severe immunosuppression was associated with mortality. This is consistent with our observation that hypogammaglobulinemia was associated with fatal outcome. Other risk factors, such as age33 or RSV infection pre-engraftment,32, 34, 35 were not statistically significant in our univariate or multivariate analysis. We also did not find any significant difference in median time to leukocyte recovery in patients infected before versus after engraftment, as found by others.11, 22 However, the numbers of patients in these subgroups in our study were relatively small.
The impact of RSV on morbidity and mortality for transplant and oncology patients has been controversial. Although RSV has been associated with fatal pneumonia without evidence of super-infections by other pathogens,10 other groups have provided evidence that RSV positivity in immunocompromised patients was not associated with any adverse outcome.7, 8 It is indeed difficult to assess to what extent the fatal outcome could be attributed to the RSV infection in our cohort, because this particular population typically suffers from several comorbidities and co-infections. The fatal cases in the outbreak described here showed that the majority (11/14 patients) had co-infections with other viral (BK virus, CMV, EBV, Herpes simplex virus—in one case acyclovir resistant), bacterial (for example, multi-drug resistant Pseudomonas aeruginosa) or fungal (Aspergillus fumigatus) pathogens. A significant contribution of RSV to the fatal outcome was clinically suspected in several patients; in addition, RSV might have contributed to susceptibility for other pathogens by damage to the mucous lining of the bronchial system.
Controversies prevail over the management of symptomatic RSV infections among adult immunocompromised patients. Although some authors have reported a mild and self-limiting course of infection without any specific treatment, even in transplant patients,7, 8 a recent pooled analysis by Shah and Chemaly17 comparing different treatment regimens for RSV infection in SCT patients showed a significantly improved outcome in patients treated with ribavirin, regardless of modality of administration. The recent ECIL-4 guidelines recommended aerosolized or systemic ribavirin therapy for RSV-infected patients undergoing allogeneic transplantation.30 A joint report of several societies for BMT, including the American Society and the European Group for Blood and Marrow Transplantation, also proposed aggressive therapy of RSV infection in allogeneic transplant recipients, however, without opting for any specific treatment strategy.36 For patients with other hematologic–oncologic conditions, there is even less evidence on the role of antiviral therapy.
Univariate and multivariate analysis in our cohort showed that treatment with oral ribavirin might be a significant protective factor against fatal outcome. The mortality rate among patients with RSV LRTID was 69% for untreated and 23% for treated patients. Although the former almost exactly matches the mortality rate of 70% for untreated HSCT patients with RSV-associated LRTID as reported by Shah and Chemaly17, the mortality rate was estimated to be 54% for patients who received systemic ribavirin treatment in this pooled analysis. The lower mortality rate of 23% in our cohort might be due to improved supportive care, taking into account the fact that some of the studies covered in the meta-analysis went back as far as 1993.
An important observation in this outbreak was the protracted viral shedding and hence the RSV carrier status of the patients affected. Although this finding has been discussed in detail from a virological point of view by Geis et al.,26 we tried to identify clinical risk factors for prolonged RSV positivity. In multivariate analysis, allogeneic transplantation was significantly associated with viral shedding for >1 week. In all, 6 of the 10 patients with viral shedding for >50 days were allogeneic transplant recipients, 5 of whom were transplanted within the previous 3 months. Thus, intensive immunosuppression following allogeneic transplantation might represent a significant risk factor for protracted RSV infection. Interestingly, treatment with ribavirin showed also a trend toward longer viral shedding, maybe attributable to the lower mortality rate in the treated cohort.
As this study is a retrospective analysis, it is associated with a number of limitations. The major limitation may be the relatively small number of patients limiting the statistical power. Furthermore, the study population does not constitute a completely homogenous group in regard to various aspects: before or early during the outbreak patients were tested for RSV because of clinically manifest respiratory symptoms or only identified retrospectively, whereas later on many patients were diagnosed with RSV infection during the systematic screenings; a treatment recommendation to administer oral ribavirin was first established at the height of the outbreak; optional therapies such as Ig preparations were given mainly at the discretion of the attending physician; finally both transplant and non-transplant patients were included. However, we think that the data presented in this retrospective analysis, being one of the largest of its kind and one of the few reporting on oral ribavirin to treat RSV infection,17 might prove helpful to the clinician, especially considering the lack of randomized controlled trials in adults.
In conclusion, this report shows that RSV is highly contagious in immunocompromised patients. Patients with severe hypogammaglobulinemia as a consequence of underlying disease and of immunosuppressive treatment have a significantly higher propensity to suffer fatal complications. Treatment with oral ribavirin might positively influence the outcome of RSV infections. Prolonged viral shedding, in particular after allogeneic transplantation, poses a major challenge among immunocompromised patients. Awareness of RSV, early recognition of infected patients and rigorous isolation of RSV-infected patients are the only effective measures in the containment of an RSV outbreak.
References
Hall CB, Walsh EE, Long CE, Schnabel KC . Immunity to and frequency of reinfection with respiratory syncytial virus. J Infect Dis 1991; 163: 693–698.
Hall CB, Douglas RG Jr., Geiman JM . Possible transmission by fomites of respiratory syncytial virus. J Infect Dis 1980; 141: 98–102.
Kuypers J, Campbell AP, Cent A, Corey L, Boeckh M . Comparison of conventional and molecular detection of respiratory viruses in hematopoietic cell transplant recipients. Transplant Infect Dis 2009; 11: 298–303.
Hall CB, Long CE, Schnabel KC . Respiratory syncytial virus infections in previously healthy working adults. Clin Infect Dis 2001; 33: 792–796.
Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA 2003; 289: 179–186.
Couch RB, Englund JA, Whimbey E . Respiratory viral infections in immunocompetent and immunocompromised persons. Am J Med 1997; 102: 2–9 discussion 25-6..
Aslan T, Fassas AB, Desikan R, Siegel D, Munshi N, Mehta J et al. Patients with multiple myeloma may safely undergo autologous transplantation despite ongoing RSV infection and no ribavirin therapy. Bone Marrow Transplant 1999; 24: 505–509.
Anaissie EJ, Mahfouz TH, Aslan T, Pouli A, Desikan R, Fassas A et al. The natural history of respiratory syncytial virus infection in cancer and transplant patients: implications for management. Blood 2004; 103: 1611–1617.
Avetisyan G, Mattsson J, Sparrelid E, Ljungman P . Respiratory syncytial virus infection in recipients of allogeneic stem-cell transplantation: a retrospective study of the incidence, clinical features, and outcome. Transplantation 2009; 88: 1222–1226.
Whimbey E, Champlin RE, Couch RB, Englund JA, Goodrich JM, Raad I et al. Community respiratory virus infections among hospitalized adult bone marrow transplant recipients. Clin Infect Dis 1996; 22: 778–782.
McCarthy AJ, Kingman HM, Kelly C, Taylor GS, Caul EO, Grier D et al. The outcome of 26 patients with respiratory syncytial virus infection following allogeneic stem cell transplantation. Bone Marrow Transplant 1999; 24: 1315–1322.
Machado CM, Boas LS, Mendes AV, Santos MF, da Rocha IF, Sturaro D et al. Low mortality rates related to respiratory virus infections after bone marrow transplantation. Bone Marrow Transplant 2003; 31: 695–700.
Harrington RD, Hooton TM, Hackman RC, Storch GA, Osborne B, Gleaves CA et al. An outbreak of respiratory syncytial virus in a bone marrow transplant center. J Infect Dis 1992; 165: 987–993.
Nichols WG, Gooley T, Boeckh M . Community-acquired respiratory syncytial virus and parainfluenza virus infections after hematopoietic stem cell transplantation: the Fred Hutchinson Cancer Research Center experience. Biol Blood Marrow Transplant 2001; 7 (Suppl): 11S–15S.
Food and Drug Administration. Ribavirin aerosol approved for severe cases of RSV in infants and young children. FDA Drug Bull 1986; 16: 7.
IMpact-RSV Study Group. Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. The IMpact-RSV Study Group. Pediatrics 1998; 102 (3 Pt 1): 531–537.
Shah JN, Chemaly RF . Management of RSV infections in adult recipients of hematopoietic stem cell transplantation. Blood 2011; 117: 2755–2763.
Dizdar EA, Aydemir C, Erdeve O, Sari FN, Oguz S, Uras N et al. Respiratory syncytial virus outbreak defined by rapid screening in a neonatal intensive care unit. J Hospital Infect 2010; 75: 292–294.
Abadesso C, Almeida HI, Virella D, Carreiro MH, Machado MC . Use of palivizumab to control an outbreak of syncytial respiratory virus in a neonatal intensive care unit. J Hospital Infect 2004; 58: 38–41.
Thorburn K, Kerr S, Taylor N, van Saene HK . RSV outbreak in a paediatric intensive care unit. J Hospital Infect 2004; 57: 194–201.
Jalal H, Bibby DF, Bennett J, Sampson RE, Brink NS, MacKinnon S et al. Molecular investigations of an outbreak of parainfluenza virus type 3 and respiratory syncytial virus infections in a hematology unit. J Clin Microbiol 2007; 45: 1690–1696.
Abdallah A, Rowland KE, Schepetiuk SK, To LB, Bardy P . An outbreak of respiratory syncytial virus infection in a bone marrow transplant unit: effect on engraftment and outcome of pneumonia without specific antiviral treatment. Bone Marrow Transplant 2003; 32: 195–203.
Taylor GS, Vipond IB, Caul EO . Molecular epidemiology of outbreak of respiratory syncytial virus within bone marrow transplantation unit. J Clin Microbiol 2001; 39: 801–803.
Mazzulli T, Peret TC, McGeer A, Cann D, MacDonald KS, Chua R et al. Molecular characterization of a nosocomial outbreak of human respiratory syncytial virus on an adult leukemia/lymphoma ward. J Infect Dis 1999; 180: 1686–1689.
Jones BL, Clark S, Curran ET, McNamee S, Horne G, Thakker B et al. Control of an outbreak of respiratory syncytial virus infection in immunocompromised adults. J Hospital Infect 2000; 44: 53–57.
Geis S, Prifert C, Weissbrich B, Lehners N, Egerer G, Eisenbach C et al. Molecular characterization of a respiratory syncytial virus (RSV) outbreak in a Hematology Unit, Heidelberg, Germany. J Clin Microbiol 2012; 51: 155–162.
Kilham L, Ferm VH . Congenital anomalies induced in hamster embryos with ribavirin. Science 1977; 195: 413–414.
De Franceschi L, Fattovich G, Turrini F, Ayi K, Brugnara C, Manzato F et al. Hemolytic anemia induced by ribavirin therapy in patients with chronic hepatitis C virus infection: role of membrane oxidative damage. Hepatology 2000; 31: 997–1004.
Black CP . Systematic review of the biology and medical management of respiratory syncytial virus infection. Respiratory Care 2003; 48: 209–231 discussion 231-3.
Hirsch HH, Martino R, Ward KN, Boeckh M, Einsele H, Ljungman P . Fourth European Conference on Infections in Leukaemia (ECIL-4): guidelines for diagnosis and treatment of human respiratory syncytial virus, parainfluenza virus, metapneumovirus, rhinovirus, and coronavirus. Clin Infect Dis 2013; 56: 258–266.
Heinze G, Schemper M . A solution to the problem of separation in logistic regression. Stat Med 2002; 21: 2409–2419.
Khanna N, Widmer AF, Decker M, Steffen I, J Halter, D Heim et al. Respiratory syncytial virus infection in patients with hematological diseases: single-center study and review of the literature. Clin Infect Dis 2008; 46: 402–412.
Chemaly RF, Ghosh S, Bodey GP, Rohatgi N, Safdar A, Keating MJ et al. Respiratory viral infections in adults with hematologic malignancies and human stem cell transplantation recipients: a retrospective study at a major cancer center. Medicine 2006; 85: 278–287.
Ghosh S, Champlin RE, Ueno NT, Anderlini P, Rolston K, Raad I et al. Respiratory syncytial virus infections in autologous blood and marrow transplant recipients with breast cancer: combination therapy with aerosolized ribavirin and parenteral immunoglobulins. Bone Marrow Transplant 2001; 28: 271–275.
Small TN, Casson A, Malak SF, Boulad F, Kiehn TE, Stiles J et al. Respiratory syncytial virus infection following hematopoietic stem cell transplantation. Bone Marrow Transplant 2002; 29: 321–327.
Tomblyn M, Chiller T, Einsele H, Gress R, Sepkowitz K, Storek J et al. Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: a global perspective. Biol Blood Marrow Transplant 2009; 15: 1143–1238.
Acknowledgements
We thank the nurses and physicians working at the Department of Hematology–Oncology at the University of Heidelberg for their commitment in containing this outbreak of RSV infections.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Lehners, N., Schnitzler, P., Geis, S. et al. Risk factors and containment of respiratory syncytial virus outbreak in a hematology and transplant unit. Bone Marrow Transplant 48, 1548–1553 (2013). https://doi.org/10.1038/bmt.2013.94
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2013.94
Keywords
This article is cited by
-
Target capture sequencing reveals a monoclonal outbreak of respiratory syncytial virus B infections among adult hematologic patients
Antimicrobial Resistance & Infection Control (2022)
-
Ribavirin for Treatment of Subjects with Respiratory Syncytial Virus-Related Infection: A Systematic Review and Meta-Analysis
Advances in Therapy (2022)
-
Evaluation of prognostic scores for respiratory syncytial virus infection in a French multicentre cohort of allogeneic haematopoietic stem cell transplantation recipients
Bone Marrow Transplantation (2021)
-
The effect of timing on community acquired respiratory virus infection mortality during the first year after allogeneic hematopoietic stem cell transplantation: a prospective epidemiological survey
Bone Marrow Transplantation (2020)
-
Are We Overlooking the Use of Oral Ribavirin for Respiratory Syncytial Virus Infection Following Hematopoietic Stem Cell Transplantation?
Current Treatment Options in Infectious Diseases (2019)