Abstract
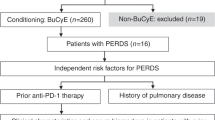
Cryptogenic organizing pneumonia (COP), previously known as bronchiolitis obliterans organizing pneumonia (BOOP), is a significant complication after allogeneic hematopoietic SCT (HCT). However, the pathogenesis of this complication has not yet been elucidated. Therefore, we identified the pre-transplant risk factors for the development of COP/BOOP using the Japan transplant registry database between 2005 and 2009. Among 9550 eligible recipients, 193 experienced COP/BOOP (2%). HLA disparity (odds ratio (OR) 1.51, P=0.05), female-to-male HCT (OR 1.53, P=0.023), and PBSC transplant (OR 1.84, P=0.0076) were significantly associated with an increased risk of COP/BOOP. On the other hand, BU-based myeloablative conditioning (OR 0.52, P=0.033), or fludarabine-based reduced-intensity conditioning (OR 0.50, P=0.0011) in comparison with a TBI-based regimen and in vivo T-cell depletion (OR 0.46, P=0.055) were associated with a lower risk. Of the 193 patients with COP/BOOP, 77 died, including non-relapse death in 46 (59%). Pulmonary failure and fatal infection accounted for 41% (n=19) and 26% (n=12) of the non-relapse death. Allogeneic immunity and conditioning toxicity could be associated with COP/BOOP. Prospective studies are required to elucidate the true risk factors for COP/BOOP and to develop a prophylactic approach.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Change history
09 October 2013
This article has been corrected since Advance Online Publication and a Corrigendum is also printed in this issue
References
Demedts M, Costabel U . ATS/ERS international multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Eur Respir J 2002; 19: 794–796.
Afessa B, Litzow MR, Tefferi A . Bronchiolitis obliterans and other late onset non-infectious pulmonary complications in hematopoietic stem cell transplantation. Bone Marrow Transplant 2001; 28: 425–434.
Yoshihara S, Yanik G, Cooke KR, Mineishi S . Bronchiolitis obliterans syndrome (BOS), bronchiolitis obliterans organizing pneumonia (BOOP), and other late-onset noninfectious pulmonary complications following allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2007; 13: 749–759.
Watkins TR, Chien JW, Crawford SW . Graft versus host-associated pulmonary disease and other idiopathic pulmonary complications after hematopoietic stem cell transplant. Semin Respir Crit Care Med 2005; 26: 482–489.
Cordier JF . Organising pneumonia. Thorax 2000; 55: 318–328.
Alasaly K, Muller N, Ostrow DN, Champion P, FitzGerald JM . Cryptogenic organizing pneumonia. A report of 25 cases and a review of the literature. Medicine 1995; 74: 201–211.
Yousem SA . The histological spectrum of pulmonary graft-versus-host disease in bone marrow transplant recipients. Hum Pathol 1995; 26: 668–675.
Freudenberger TD, Madtes DK, Curtis JR, Cummings P, Storer BE, Hackman RC . Association between acute and chronic graft-versus-host disease and bronchiolitis obliterans organizing pneumonia in recipients of hematopoietic stem cell transplants. Blood 2003; 102: 3822–3828.
Jinta M, Ohashi K, Ohta T, Ieki R, Abe K, Kamata N et al. Clinical features of allogeneic hematopoietic stem cell transplantation-associated organizing pneumonia. Bone Marrow Transplant 2007; 40: 465–472.
Kanda Y, Takahashi T, Imai Y, Miyagawa K, Ohishi N, Oka T et al. Bronchiolitis obliterans organizing pneumonia after syngeneic bone marrow transplantation for acute lymphoblastic leukemia. Bone Marrow Transplant 1997; 19: 1251–1253.
Kleinau I, Perez-Canto A, Schmid HJ, Grassot A, Staab D, Renz H et al. Bronchiolitis obliterans organizing pneumonia and chronic graft-versus-host disease in a child after allogeneic bone marrow transplantation. Bone Marrow Transplant 1997; 19: 841–844.
Palmas A, Tefferi A, Myers JL, Scott JP, Swensen SJ, Chen MG et al. Late-onset noninfectious pulmonary complications after allogeneic bone marrow transplantation. Br J Haematol 1998; 100: 680–687.
Sakai R, Kanamori H, Nakaseko C, Yoshiba F, Fujimaki K, Sakura T et al. Air-leak syndrome following allo-SCT in adult patients: report from the Kanto Study Group for Cell Therapy in Japan. Bone Marrow Transplant 2011; 46: 379–384.
Patriarca F, Skert C, Sperotto A, Damiani D, Cerno M, Geromin A et al. Incidence, outcome, and risk factors of late-onset noninfectious pulmonary complications after unrelated donor stem cell transplantation. Bone Marrow Transplant 2004; 33: 751–758.
Huisman C, van der Straaten HM, Canninga-van Dijk MR, Fijnheer R, Verdonck LF . Pulmonary complications after T-cell-depleted allogeneic stem cell transplantation: low incidence and strong association with acute graft-versus-host disease. Bone Marrow Transplant 2006; 38: 561–566.
Ditschkowski M, Elmaagacli AH, Trenschel R, Peceny R, Koldehoff M, Schulte C et al. T-cell depletion prevents from bronchiolitis obliterans and bronchiolitis obliterans with organizing pneumonia after allogeneic hematopoietic stem cell transplantation with related donors. Haematologica 2007; 92: 558–561.
Yotsumoto S, Okada F, Ando Y, Matsumoto S, Wakisaka M, Mori H et al. Bronchiolitis obliterans organizing pneumonia after bone marrow transplantation: association with human leukocyte antigens. J Comput Assist Tomogr 2007; 31: 132–137.
Atsuta Y, Suzuki R, Yoshimi A, Gondo H, Tanaka J, Hiraoka A et al. Unification of hematopoietic stem cell transplantation registries in Japan and establishment of the TRUMP System. Int J Hematol 2007; 86: 269–274.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant 1995; 15: 825–828.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med 1980; 69: 204–217.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transplant 2009; 15: 367–369.
Kanda Y . Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant 2013; 48: 452–458.
Stem Cell Trialists' Collaborative Group. Allogeneic peripheral blood stem-cell compared with bone marrow transplantation in the management of hematologic malignancies: an individual patient data meta-analysis of nine randomized trials. J Clin Oncol 2005; 23: 5074–5087.
Gahrton G . Risk assessment in haematopoietic stem cell transplantation: impact of donor-recipient sex combination in allogeneic transplantation. Best Pract Res Clin Haematol 2007; 20: 219–229.
Santo Tomas LH, Loberiza FR Jr., Klein JP, Layde PM, Lipchik RJ, Rizzo JD et al. Risk factors for bronchiolitis obliterans in allogeneic hematopoietic stem-cell transplantation for leukemia. Chest 2005; 128: 153–161.
Nakasone H, Kanda J, Yano S, Atsuta Y, Ago H, Fukuda T et al. A case-control study of bronchiolitis obliterans syndrome following allogeneic hematopoietic stem cell transplantation. Transpl Int 2013; 26: 631–639.
Spiera RF, Gordon JK, Mersten JN, Magro CM, Mehta M, Wildman HF et al. Imatinib mesylate (Gleevec) in the treatment of diffuse cutaneous systemic sclerosis: results of a 1-year, phase IIa, single-arm, open-label clinical trial. Ann Rheum Dis 2011; 70: 1003–1009.
Weshler Z, Breuer R, Or R, Naparstek E, Pfeffer MR, Lowental E et al. Interstitial pneumonitis after total body irradiation: effect of partial lung shielding. Br J Haematol 1990; 74: 61–64.
Acknowledgements
We greatly appreciate the work of all of the physicians and data managers at the centers that contributed valuable data on transplantation to the Japan Society for Hematopoietic Cell Transplantation (JSHCT), the Japanese Society of Pediatric Hematology and Oncology (JSPHO) the Japan Marrow Donor Program (JMDP) and the Japan Cord Blood Bank Network (JCBBN). We also thank all of the members of the Transplant Registry Unified Management committees at JSHCT, JSPHO, JMDP and JCBBN for their dedication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflicts of interest.
Additional information
Author contributions
HN designed the study, analyzed data and wrote the manuscript. MO, NS and NF advised on methods, analyzed the data and wrote the manuscript. KK, TE, and KM collected the data. HS, HY, YM, and KK collected the data and were responsible for managing the data from JSHCT, JSPHO, JMDP and JCBBN, respectively. RS analyzed and managed the unified registry database, and wrote the manuscript. TF analyzed the data, wrote the manuscript and was responsible for the study and the Complications-Working Group of JSHCT.
Rights and permissions
About this article
Cite this article
Nakasone, H., Onizuka, M., Suzuki, N. et al. Pre-transplant risk factors for cryptogenic organizing pneumonia/bronchiolitis obliterans organizing pneumonia after hematopoietic cell transplantation. Bone Marrow Transplant 48, 1317–1323 (2013). https://doi.org/10.1038/bmt.2013.116
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2013.116
Keywords
This article is cited by
-
Association between early corticosteroid administration and long-term survival in non-infectious pulmonary complications after allogeneic hematopoietic stem cell transplantation
International Journal of Hematology (2023)
-
Clinical characteristics of late-onset interstitial pneumonia after allogeneic hematopoietic stem cell transplantation
International Journal of Hematology (2023)
-
Significance of alveolar nitric oxide concentration in the airway of patients with organizing pneumonia after allogeneic hematopoietic stem cell transplantation
Annals of Hematology (2022)
-
Risk factors and prognosis of non-infectious pulmonary complications after allogeneic hematopoietic stem cell transplantation
International Journal of Hematology (2022)
-
Characterization of localized macrophages in bronchiolitis obliterans after allogeneic hematopoietic cell transplantation
International Journal of Hematology (2021)