Abstract
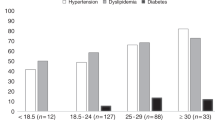
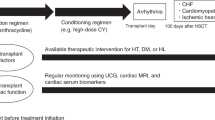
Increasing numbers of hematopoietic cell transplantations (HCTs) are being performed annually with a greater number of long-term survivors. There is increasing concern regarding the late complications and long-term effects that are secondary to treatment exposures before HCT as well as during the HCT conditioning therapy. In both the autologous as well as allogeneic transplant setting, transplant survivors experience mortality rates higher than the general population and the risk of premature cardiovascular (CV)-related death is increased 2.3-fold compared with the general population. The etiology of CV-related deaths in HCT survivors is multifactorial; however, increasing evidence suggests that HCT survivors are at higher risk of developing adverse CV risk factors leading to the development of the metabolic syndrome (a constellation high triglyceride levels, low high-density lipoprotein-cholesterol, hypertension, high fasting blood sugars and increased waist circumference), which then predisposes individuals to risk for early CV-related death. Resistance to insulin is the primary underlying pathophysiologic mechanism that contributes to the development of metabolic syndrome and HCT survivors have been shown to be more likely to develop hypertension, hyperlipidemia and to be insulin resistant. However, the relationship between HCT-related treatment exposures (total body irradiation, high dose chemotherapy, calcineurin inhibitors, steroids, etc) and transplant-related complications (such as GVHD) with the development of CV risk factors and insulin resistance is still in the early stages of investigation. Greater knowledge of the concern regarding CV risk in HCT survivors among both patients and care providers will provide the opportunity for appropriate screening as well as interventions for modifiable risk factors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Gooley TA, Chien JW, Pergam SA, Hingorani S, Sorror ML, Boeckh M et al. Reduced mortality after allogeneic hematopoietic-cell transplantation. N Engl J Med 2010; 363: 2091–2101.
Bhatia S, Francisco L, Carter A, Sun CL, Baker KS, Gurney JG et al. Late mortality after allogeneic hematopoietic cell transplantation and functional status of long-term survivors: report from the Bone Marrow Transplant Survivor Study. Blood 2007; 110: 3784–3792.
Bhatia S, Robison LL, Francisco L, Carter A, Liu Y, Grant M et al. Late mortality in survivors of autologous hematopoietic-cell transplantation: report from the Bone Marrow Transplant Survivor Study. Blood 2005; 105: 4215–4222.
Martin PJ, Counts Jr GW, Appelbaum FR, Lee SJ, Sanders JE, Deeg HJ et al. Life expectancy in patients surviving more than 5 years after hematopoietic cell transplantation. J Clin Oncol 2010; 28: 1011–1016.
Mertens AC, Liu Q, Neglia JP, Wasilewski K, Leisenring W, Armstrong GT et al. Cause-specific late mortality among 5-year survivors of childhood cancer: the Childhood Cancer Survivor Study. J Natl Cancer Inst 2008; 100: 1368–1379.
Baker KS, Ness KK, Weisdorf D, Francisco L, Sun CL, Forman S et al. Late effects in survivors of acute leukemia treated with hematopoietic cell transplantation: a report from the Bone Marrow Transplant Survivor Study. Leukemia 2010; 24: 2039–2047.
Baker KS, Gurney JG, Ness KK, Bhatia R, Forman SJ, Francisco L et al. Late effects in survivors of chronic myeloid leukemia treated with hematopoietic cell transplantation: results from the Bone Marrow Transplant Survivor Study. Blood 2004; 104: 1898–1906.
Reusch JE . Current concepts in insulin resistance, type 2 diabetes mellitus, and the metabolic syndrome. Am J Cardiol 2002; 90: 19G–26G.
Trevisan M, Liu J, Bahsas FB, Menotti A . Syndrome X and mortality: a population-based study. Risk Factor and Life Expectancy Research Group. Am J Epidemiol 1998; 148: 958–966.
Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 2002; 288: 2709–2716.
Reaven GM . Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 1988; 37: 1595–1607.
Despres JP, Lamarche B, Mauriege P, Cantin B, Dagenais GR, Moorjani S et al. Hyperinsulinemia as an independent risk factor for ischemic heart disease. N Engl J Med 1996; 334: 952–957.
Ruige JB, Assendelft WJ, Dekker JM, Kostense PJ, Heine RJ, Bouter LM . Insulin and risk of cardiovascular disease: a meta-analysis. Circulation 1998; 97: 996–1001.
Begum N, Song Y, Rienzie J, Ragolia L . Vascular smooth muscle cell growth and insulin regulation of mitogen-activated protein kinase in hypertension. Am J Physiol 1998; 275 (1 Part 1): C42–C49.
Nagai M, Kamide K, Rakugi H, Takiuchi S, Imai M, Kida I et al. Role of endothelin-1 induced by insulin in the regulation of vascular cell growth. Am J Hypertens 2003; 16: 223–228.
Goalstone ML, Natarajan R, Standley PR, Walsh MF, Leitner JW, Carel K et al. Insulin potentiates platelet-derived growth factor action in vascular smooth muscle cells. Endocrinology 1998; 139: 4067–4072.
Vicent D, Ilany J, Kondo T, Naruse K, Fisher SJ, Kisanuki YY et al. The role of endothelial insulin signaling in the regulation of vascular tone and insulin resistance. J Clin Invest 2003; 111: 1373–1380.
Reaven GM . Pathophysiology of insulin resistance in human disease. Physiol Rev 1995; 75: 473–486.
Cai D, Yuan M, Frantz DF, Melendez PA, Hansen L, Lee J et al. Local and systemic insulin resistance resulting from hepatic activation of IKK-beta and NF-kappaB. Nat Med 2005; 11: 183–190.
An J, Muoio DM, Shiota M, Fujimoto Y, Cline GW, Shulman GI et al. Hepatic expression of malonyl-CoA decarboxylase reverses muscle, liver and whole-animal insulin resistance. Nat Med 2004; 10: 268–274.
Biddinger SB, Hernandez-Ono A, Rask-Madsen C, Haas JT, Aleman JO, Suzuki R et al. Hepatic insulin resistance is sufficient to produce dyslipidemia and susceptibility to atherosclerosis. Cell Metab 2008; 7: 125–134.
Kim SP, Ellmerer M, Van Citters GW, Bergman RN . Primacy of hepatic insulin resistance in the development of the metabolic syndrome induced by an isocaloric moderate-fat diet in the dog. Diabetes 2003; 52: 2453–2460.
Cavaghan MK, Ehrmann DA, Polonsky KS . Interactions between insulin resistance and insulin secretion in the development of glucose intolerance. J Clin Invest 2000; 106: 329–333.
Mittelman SD, Van Citters GW, Kim SP, Davis DA, Dea MK, Hamilton-Wessler M et al. Longitudinal compensation for fat-induced insulin resistance includes reduced insulin clearance and enhanced beta-cell response. Diabetes 2000; 49: 2116–2125.
Sinha R, Fisch G, Teague B, Tamborlane WV, Banyas B, Allen K et al. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med 2002; 346: 802–810.
Taittonen L, Uhari M, Nuutinen M, Turtinen J, Pokka T, Akerblom HK . Insulin and blood pressure among healthy children. Cardiovascular risk in young Finns. Am J Hypertens 1996; 9: 194–199.
Odeleye OE, de Courten M, Pettitt DJ, Ravussin E . Fasting hyperinsulinemia is a predictor of increased body weight gain and obesity in Pima Indian children. Diabetes 1997; 46: 1341–1345.
Bao W, Srinivasan SR, Berenson GS . Persistent elevation of plasma insulin levels is associated with increased cardiovascular risk in children and young adults. The Bogalusa Heart Study. Circulation 1996; 93: 54–59.
Sinaiko AR, Steinberger J, Moran A, Prineas RJ, Vessby B, Basu S et al. Relation of body mass index and insulin resistance to cardiovascular risk factors, inflammatory factors, and oxidative stress during adolescence. Circulation 2005; 111: 1985–1991.
Taskinen M, Saarinen-Pihkala UM, Hovi L, Lipsanen-Nyman M . Impaired glucose tolerance and dyslipidaemia as late effects after bone- marrow transplantation in childhood. Lancet 2000; 356: 993–997.
Lorini R, Cortona L, Scaramuzza A, De Stefano P, Locatelli F, Bonetti F et al. Hyperinsulinemia in children and adolescents after bone marrow transplantation. Bone Marrow Transplant 1995; 15: 873–877.
Chow EJ, Simmons JH, Roth CL, Baker KS, Hoffmeister PA, Sanders JE et al. Increased cardiometabolic traits in pediatric survivors of acute lymphoblastic leukemia treated with total body irradiation. Biol Blood Marrow Transplant 2010; 16: 1674–1681.
Gurney JG, Ness KK, Sibley SD, O’Leary M, Dengel DR, Lee JM et al. Metabolic syndrome and growth hormone deficiency in adult survivors of childhood acute lymphoblastic leukemia. Cancer 2006; 107: 1303–1312.
Taskinen M, Lipsanen-Nyman M, Tiitinen A, Hovi L, Saarinen-Pihkala UM . Insufficient growth hormone secretion is associated with metabolic syndrome after allogeneic stem cell transplantation in childhood. J Pediatr Hematol Oncol 2007; 29: 529–534.
Baker KS, Ness KK, Steinberger J, Carter A, Francisco L, Burns LJ et al. Diabetes, hypertension, and cardiovascular events in survivors of hematopoietic cell transplantation: a report from the bone marrow transplantation survivor study. Blood 2007; 109: 1765–1772.
Chow E, Mueller B, Baker K, Cushing-Haugen K, Flowers M, Martin P et al. Cardiovascular hospitalizations and mortality among recipients of hematopoietic stem cell transplantation. Ann Intern Med 2011 (In press).
Narici MV, Maffulli N . Sarcopenia: characteristics, mechanisms and functional significance. Br Med Bull 2010; 95: 139–159.
Eaton SB, Cordain L, Sparling PB . Evolution, body composition, insulin receptor competition, and insulin resistance. Prev Med 2009; 49: 283–285.
Boirie Y . Physiopathological mechanism of sarcopenia. J Nutr Health Aging 2009; 13: 717–723.
Baker KS, Chow EJ, Koves I, Goodman P, Leisenring W, Hoffmeister PA et al. Adverse impact of hematopoietic cell transplantation (HCT) on body composition and insulin resistance is associated with increased cardiovascular risk. Biol Blood Marrow Transplant 2011; 17 (Suppl 2): S174.
Morris B, Partap S, Yeom K, Gibbs IC, Fisher PG, King AA . Cerebrovascular disease in childhood cancer survivors: a Children's Oncology Group Report. Neurology 2009; 73: 1906–1913.
Nandagopal R, Laverdiere C, Mulrooney D, Hudson MM, Meacham L . Endocrine late effects of childhood cancer therapy: a report from the Children's Oncology Group. Horm Res 2008; 69: 65–74.
Shankar SM, Marina N, Hudson MM, Hodgson DC, Adams MJ, Landier W et al. Monitoring for cardiovascular disease in survivors of childhood cancer: report from the Cardiovascular Disease Task Force of the Children's Oncology Group. Pediatrics 2008; 121: e387–e396.
Skinner R, Wallace WH, Levitt G . Therapy Based Long Term Follow Up, 2nd edn; 2006. United Kingdom Children's Cancer Study Group. http://www.cclg.org.uk/library/19/PracticeStatement/LTFU-full.pdf; accessed 1 December 2010.
Kavey RE, Allada V, Daniels SR, Hayman LL, McCrindle BW, Newburger JW et al. Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association Expert Panel on Population and Prevention Science; the Councils on Cardiovascular Disease in the Young, Epidemiology and Prevention, Nutrition, Physical Activity and Metabolism, High Blood Pressure Research, Cardiovascular Nursing, and the Kidney in Heart Disease; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics. Circulation 2006; 114: 2710–2738.
US Preventative Services Task Force. http://www.uspreventiveservicestaskforce.org/recommendations.htm; accessed 10 May 2010.
Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows AT et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med 2006; 355: 1572–1582.
Reulen RC, Winter DL, Frobisher C, Lancashire ER, Stiller CA, Jenney ME et al. Long-term cause-specific mortality among survivors of childhood cancer. JAMA 2010; 304: 172–179.
Rizzo JD, Wingard JR, Tichelli A, Lee SJ, Van Lint MT, Burns LJ et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation: joint recommendations of the European Group for Blood and Marrow Transplantation, the Center for International Blood and Marrow Transplant Research, and the American Society of Blood and Marrow Transplantation. Biol Blood Marrow Transplant 2006; 12: 138–151.
Rizzo JD, Wingard JR, Tichelli A, Lee SJ, Van Lint MT, Burns LJ et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation: joint recommendations of the European Group for Blood and Marrow Transplantation, Center for International Blood and Marrow Transplant Research, and the American Society for Blood and Marrow Transplantation (EBMT/CIBMTR/ASBMT). Bone Marrow Transplant 2006; 37: 249–261.
Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH . Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988–1994. Arch Pediatr Adolesc Med 2003; 157: 821–827.
Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 2003; 26: 3160–3167.
Grundy SM, Brewer Jr HB, Cleeman JI, Smith Jr SC, Lenfant C . Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004; 109: 433–438.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Baker, K., Chow, E. & Steinberger, J. Metabolic syndrome and cardiovascular risk in survivors after hematopoietic cell transplantation. Bone Marrow Transplant 47, 619–625 (2012). https://doi.org/10.1038/bmt.2011.118
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2011.118
Keywords
This article is cited by
-
Selection bias in follow-up studies of stem cell transplantation survivors: an experience within the Maastricht Observational study of late effects after Stem cell trAnsplantation (MOSA)
Annals of Hematology (2023)
-
Exercise training and NR supplementation to improve muscle mass and fitness in adolescent and young adult hematopoietic cell transplant survivors: a randomized controlled trial {1}
BMC Cancer (2022)
-
A non-interventional study of microcirculation dynamics in allogeneic hematopoietic cell transplantation survivors compared to controls: evidence of impaired microvascular response regardless of conventional cardiovascular risk factors
Bone Marrow Transplantation (2022)
-
Cardiovascular risk factors and subclinical organ damage after hematopoietic stem cell transplantation in pediatric age
Bone Marrow Transplantation (2018)
-
Prospective evaluation of metabolic syndrome and its features in a single-center series of hematopoietic stem cell transplantation recipients
Annals of Hematology (2018)