Abstract
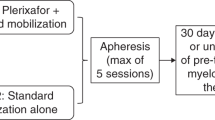
The CXCR4-inhibitor plerixafor mobilizes hematopoietic stem cells amplifying the effects of granulocyte-CSF (G-CSF). Before approval plerixafor was used in a compassionate use program (CUP) for patients who failed a previous mobilization. In the German CUP 60 patients from 23 centers (median age 56.5 years (2–75)) were given 240 μg/kg plerixafor SC 9–11 h before apheresis. A total of 78.3% (47/60) received G-CSF for 4 days before plerixafor administration; 76.6% of those (36/47) yielded at least 2.0 × 106 CD34+ cells/μL. The median cell yield was 3.35 × 106 CD34+ cells/kg (0–29.53). Nine patients received plerixafor alone or with G-CSF for less than 4 days mobilizing a median of 3.30 × 106 CD34+ cells/kg (1.6–5.6). There was no significant difference between G-CSF application for 4 days and for a shorter period of time (P=0.157). A total of 47 patients received plerixafor plus G-CSF combined with chemotherapy yielding a median of 3.28 × 106 CD34+ cells/kg (0–24.79). In all, 40 of 60 patients (66.7%) proceeded to transplantation, and achieved a timely and stable engraftment. Side effects were rare and manageable. In conclusion, mobilization with plerixafor in poor mobilizers is safe and results in a sufficient stem cell harvest in the majority of patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Demirer T, Bensinger WI, Buckner CD . Peripheral blood stem cell mobilization for high-dose chemotherapy. J Hematother 1999; 8: 103–113.
Bensinger W, Appelbaum F, Rowley S, Storb R, Sanders J, Lilleby K et al. Factors that influence collection and engraftment of autologous peripheral-blood stem cells. J Clin Oncol 1995; 13: 2547–2555.
Pusic I, Jiang SY, Landua S, Uy GL, Rettig MP, Cashen AF et al. Impact of mobilization and remobilization strategies on achieving sufficient stem cell yields for autologous transplantation. Biol Blood Marrow Transplant 2008; 14: 1045–1056.
Villalon L, Odriozola J, Larana JG, Zamora C, Perez de Oteyza J, Jodra MH et al. Autologous peripheral blood progenitor cell transplantation with <2 × 10 CD34(+)/kg: an analysis of variables concerning mobilisation and engraftment. Hematol J 2000; 1: 374–381.
Kessinger A, Sharp JG . The whys and hows of hematopoietic progenitor and stem cell mobilization. Bone Marrow Transplant 2003; 31: 319–329.
Koenigsmann M, Jentsch-Ullrich K, Mohren M, Becker E, Heim M, Franke A . The role of diagnosis in patients failing peripheral blood progenitor cell mobilization. Transfusion 2004; 44: 777–784.
Pastore D, Specchia G, Mestice A, Liso A, Pannunzio A, Carluccio P et al. Good and poor CD34+ cell mobilization in acute leukemia: analysis of factors affecting the yield of progenitor cells. Bone Marrow Transplant 2004; 33: 1083–1087.
Moog R . Management strategies for poor peripheral blood stem cell mobilization. Transfus Apher Sci 2008; 38: 229–236.
Mendrone Jr A, Arrais CA, Saboya R, Chamone Dde A, Dulley FL . Factors affecting hematopoietic progenitor cell mobilization: an analysis of 307 patients. Transfus Apher Sci 2008; 39: 187–192.
Pavone V, Gaudio F, Console G, Vitolo U, Iacopino P, Guarini A et al. Poor mobilization is an independent prognostic factor in patients with malignant lymphomas treated by peripheral blood stem cell transplantation. Bone Marrow Transplant 2006; 37: 719–724.
Kuittinen T, Nousiainen T, Halonen P, Mahlamaki E, Jantunen E . Prediction of mobilisation failure in patients with non-Hodgkin’lymphoma. Bone Marrow Transplant 2004; 33: 907–912.
Akhtar S, Weshi AE, Rahal M, Khafaga Y, Tbakhi A, Humaidan H et al. Factors affecting autologous peripheral blood stem cell collection in patients with relapsed or refractory diffuse large cell lymphoma and Hodgkin lymphoma: a single institution result of 168 patients. Leuk Lymphoma 2008; 49: 769–778.
Wuchter P, Ran D, Bruckner T, Schmitt T, Witzens-Harig M, Neben K et al. Poor mobilization of hematopoietic stem cells-definitions, incidence, risk factors, and impact on outcome of autologous transplantation. Biol Blood Marrow Transplant 2010; 16: 490–499.
Nagasawa T . A chemokine, SDF-1/PBSF, and its receptor, CXC chemokine receptor 4, as mediators of hematopoiesis. Int J Hematol 2000; 72: 408–411.
Lee Y, Gotoh A, Kwon HJ, You M, Kohli L, Mantel C et al. Enhancement of intracellular signaling associated with hematopoietic progenitor cell survival in response to SDF-1/CXCL12 in synergy with other cytokines. Blood 2002; 99: 4307–4317.
Mohle R, Bautz F, Rafii S, Moore MA, Brugger W, Kanz L . The chemokine receptor CXCR-4 is expressed on CD34+ hematopoietic progenitors and leukemic cells and mediates transendothelial migration induced by stromal cell-derived factor-1. Blood 1998; 91: 4523–4530.
Gerlach LO, Skerlj RT, Bridger GJ, Schwartz TW . Molecular interactions of cyclam and bicyclam non-peptide antagonists with the CXCR4 chemokine receptor. J Biol Chem 2001; 276: 14153–14160.
Hubel K, Liles WC, Broxmeyer HE, Rodger E, Wood B, Cooper S et al. Leukocytosis and mobilization of CD34+ hematopoietic progenitor cells by AMD3100, a CXCR4 antagonist. Support Cancer Ther 2004; 1: 165–172.
Hendrix CW, Collier AC, Lederman MM, Schols D, Pollard RB, Brown S et al. Safety, pharmacokinetics, and antiviral activity of AMD3100, a selective CXCR4 receptor inhibitor, in HIV-1 infection. J Acquir Immune Defic Syndr 2004; 37: 1253–1262.
Liles WC, Rodger E, Broxmeyer HE, Dehner C, Badel K, Calandra G et al. Augmented mobilization and collection of CD34+ hematopoietic cells from normal human volunteers stimulated with granulocyte-colony-stimulating factor by single-dose administration of AMD3100, a CXCR4 antagonist. Transfusion 2005; 45: 295–300.
Flomenberg N, Devine SM, Dipersio JF, Liesveld JL, McCarty JM, Rowley SD et al. The use of AMD3100 plus G-CSF for autologous hematopoietic progenitor cell mobilization is superior to G-CSF alone. Blood 2005; 106: 1867–1874.
Tricot G, Cottler-Fox MH, Calandra G . Safety and efficacy assessment of plerixafor in patients with multiple myeloma proven or predicted to be poor mobilizers, including assessment of tumor cell mobilization. Bone Marrow Transplant 2010; 45: 63–68.
Duarte RF, Shaw BE, Marin P, Kottaridis P, Ortiz M, Morante C et al. Plerixafor plus granulocyte CSF can mobilize hematopoietic stem cells from multiple myeloma and lymphoma patients failing previous mobilization attempts: EU compassionate use data. Bone Marrow Transplant (e-pub ahead of print 22 March 2010; doi:10.1038/bmt.2010.54).
Calandra G, McCarty J, McGuirk J, Tricot G, Crocker SA, Badel K et al. AMD3100 plus G-CSF can successfully mobilize CD34+ cells from non-Hodgkin's lymphoma, Hodgkin's disease and multiple myeloma patients previously failing mobilization with chemotherapy and/or cytokine treatment: compassionate use data. Bone Marrow Transplant 2008; 41: 331–338.
Tricot G, Cottler-Fox MH, Calandra G . Safety and efficacy assessment of plerixafor in patients with multiple myeloma proven or predicted to be poor mobilizers, including assessment of tumor cell mobilization. Bone Marrow Transplant 2010; 45: 63–68.
Micallef IN, Stiff PJ, DiPersio JF, Maziarz RT, McCarty JM, Bridger G et al. Successful stem cell remobilization using plerixafor (mozobil) plus granulocyte colony-stimulating factor in patients with non-hodgkin lymphoma: results from the plerixafor NHL phase 3 study rescue protocol. Biol Blood Marrow Transplant 2009; 15: 1578–1586.
Fowler CJ, Dunn A, Hayes-Lattin B, Hansen K, Hansen L, Lanier K et al. Rescue from failed growth factor and/or chemotherapy HSC mobilization with G-CSF and plerixafor (AMD3100): an institutional experience. Bone Marrow Transplant 2009; 43: 909–917.
Flomenberg N, Comenzo RL, Badel K, Calandra G . Plerixafor (Mozobil) alone to mobilize hematopoietic stem cells from multiple myeloma patients for autologous transplantation. Biol Blood Marrow Transplant 2010; 16: 695–700.
DiPersio JF, Stadtmauer EA, Nademanee A, Micallef IN, Stiff PJ, Kaufman JL et al. Plerixafor and G-CSF versus placebo and G-CSF to mobilize hematopoietic stem cells for autologous stem cell transplantation in patients with multiple myeloma. Blood 2009; 113: 5720–5726.
DiPersio JF, Micallef IN, Stiff PJ, Bolwell BJ, Maziarz RT, Jacobsen E et al. Phase III prospective randomized double-blind placebo-controlled trial of plerixafor plus granulocyte colony-stimulating factor compared with placebo plus granulocyte colony-stimulating factor for autologous stem-cell mobilization and transplantation for patients with non-Hodgkin's lymphoma. J Clin Oncol 2009; 27: 4767–4773.
Flomenberg N, DiPersio J, Calandra G . Role of CXCR4 chemokine receptor blockade using AMD3100 for mobilization of autologous hematopoietic progenitor cells. Acta Haematol 2005; 114: 198–205.
Cashen A, Lopez S, Gao F, Calandra G, MacFarland R, Badel K et al. A phase II study of plerixafor (AMD3100) plus G-CSF for autologous hematopoietic progenitor cell mobilization in patients with Hodgkin lymphoma. Biol Blood Marrow Transplant 2008; 14: 1253–1261.
Hendrix CW, Flexner C, MacFarland RT, Giandomenico C, Fuchs EJ, Redpath E et al. Pharmacokinetics and safety of AMD-3100, a novel antagonist of the CXCR-4 chemokine receptor, in human volunteers. Antimicrob Agents Chemother 2000; 44: 1667–1673.
Liles WC, Broxmeyer HE, Rodger E, Wood B, Hubel K, Cooper S et al. Mobilization of hematopoietic progenitor cells in healthy volunteers by AMD3100, a CXCR4 antagonist. Blood 2003; 102: 2728–2730.
Cashen AF, Lazarus HM, Devine SM . Mobilizing stem cells from normal donors: is it possible to improve upon G-CSF? Bone Marrow Transplant 2007; 39: 577–588.
Stewart DA, Smith C, MacFarland R, Calandra G . Pharmacokinetics and pharmacodynamics of plerixafor in patients with non-Hodgkin lymphoma and multiple myeloma. Biol Blood Marrow Transplant 2009; 15: 39–46.
Hicks ML, Lonial S, Langston A, Flowers C, Roback JD, Smith KJ et al. Optimizing the timing of chemotherapy for mobilizing autologous blood hematopoietic progenitor cells. Transfusion 2007; 47: 629–635.
Toledano H, Yahel A, Cohen IJ, Yaniv I, Stein J . Successful mobilization, harvest and transplant of peripheral blood stem cells using AMD3100 and G-CSF following high dose craniospinal irradiation for medulloblastoma in a young child. Pediatr Blood Cancer 2010; 54: 613–615.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Hübel, K., Fresen, M., Salwender, H. et al. Plerixafor with and without chemotherapy in poor mobilizers: results from the German compassionate use program. Bone Marrow Transplant 46, 1045–1052 (2011). https://doi.org/10.1038/bmt.2010.249
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2010.249
Keywords
This article is cited by
-
The timing of plerixafor addition to G-Csf and chemotherapy affects immunological recovery after autologous stem cell transplant in multiple myeloma
Bone Marrow Transplantation (2020)
-
Dynamic cellular phenotyping defines specific mobilization mechanisms of human hematopoietic stem and progenitor cells induced by SDF1α versus synthetic agents
Scientific Reports (2018)
-
Prognostic factors for re-mobilization using plerixafor and granulocyte colony-stimulating factor (G-CSF) in patients with malignant lymphoma or multiple myeloma previously failing mobilization with G-CSF with or without chemotherapy: the Korean multicenter retrospective study
Annals of Hematology (2016)
-
A plerixafor-based strategy allows adequate hematopoietic stem cell collection in poor mobilizers: results from the Canadian Special Access Program
Bone Marrow Transplantation (2014)
-
An effective mobilization strategy for lymphoma patients after failed upfront mobilization with plerixafor
Bone Marrow Transplantation (2014)