Abstract
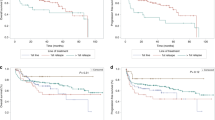
Conflicting conclusions can be drawn from the available data concerning antileukemic efficacy and risks of intrathecal (i.t.) chemoprophylaxis to children after hematopoietic SCT (HSCT). To address this, we enrolled six transplantation centers with similar treatment and patient material. Of the 397 children included, 136 patients had received post-HSCT i.t. treatment (i.t. group) and 261 had not (non-i.t. group). The two groups were, apart from the i.t. therapy given or not given, at equal risk of post-HSCT central nervous system (CNS) relapse, which was the primary endpoint studied. Isolated CNS relapses were observed in 2 (1.5%) patients from the i.t. group and 2 (1%) from the non-i.t. group. Combined relapses, including CNS, involved 4 (3%) patients from the i.t. group and 6 (2%) from the non-i.t. group. Overall survival and the occurrence of neurological side effects did not differ significantly between the groups. There was no statistically significant difference in the incidence of isolated or mixed CNS relapses between the two groups, suggesting little or no benefit from i.t. therapy post-HSCT in children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Thompson CB, Sanders JE, Flournoy N, Buckner CD, Thomas ED . The risks of central nervous system relapse and leukoencephalopathy in patients receiving marrow transplants for acute leukemia. Blood 1986; 67: 195–199.
Singhal S, Powles R, Treleaven J, Horton C, Tait D, Meller S et al. Central nervous system relapse after bone marrow transplantation for acute leukemia in first remission. Bone Marrow Transplant 1996; 17: 637–641.
Ganem G, Kuentz M, Bernaudin F, Gharbi A, Cordonnier C, Lemerle S et al. Central nervous system relapses after bone marrow transplantation for acute lymphoblastic leukemia in remission. Cancer 1989; 64: 1796–1804.
Pui CH . Central nervous system disease in acute lymphoblastic leukemia: prophylaxis and treatment. Hematology Am Soc Hematol Educ Program 2006, 142–146.
Oshima K, Kanda Y, Yamashita T, Takahashi S, Mori T, Nakaseko C et al. Central nervous system relapse of leukemia after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2008; 14: 1100–1107.
Ruutu T, Corradini P, Gratwohl A, Holler E, Apperley J, Dini G et al. Use of intrathecal prophylaxis in allogeneic haematopoietic stem cell transplantation for malignant blood diseases: a survey of the European Group for Blood and Marrow Transplantation (EBMT). Bone Marrow Transplant 2005; 35: 121–124.
Rubin J, Frost BM, Arvidson J, Wide K, Gustafsson-Jernberg A, Gustafsson B . Intrathecal chemoprophylaxis after HSCT in children. Pediatr Transplant 2008; 12: 889–895.
Thiebaut A, Thomas X, Belhabri A, Anglaret B, Archimbaud E . Impact of pre-induction therapy leukapheresis on treatment outcome in adult acute myelogenous leukemia presenting with hyperleukocytosis. Ann Hematol 2000; 79: 501–506.
Johnston DL, Alonzo TA, Gerbing RB, Lange BJ, Woods WG . Risk factors and therapy for isolated central nervous system relapse of pediatric acute myeloid leukemia. J Clin Oncol 2005; 23: 9172–9178.
De Angulo G, Yuen C, Palla SL, Anderson PM, Zweidler-McKay PA . Absolute lymphocyte count is a novel prognostic indicator in ALL and AML: implications for risk stratification and future studies. Cancer 2008; 112: 407–415.
Karnofsky DA, Patterson PA, Ridgway LP . Effect of folic acid, 4-amino folic acids and related substances on growth of chick embryo. Proc Soc Exp Biol Med 1949; 71: 447–452.
Lansky SB, List MA, Lansky LL, Ritter-Sterr C, Miller DR . The measurement of performance in childhood cancer patients. Cancer 1987; 60: 1651–1656.
Aytac S, Yetgin S, Tavil B . Acute and long-term neurologic complications in children with acute lymphoblastic leukemia. Turk J Pediatr 2006; 48: 1–7.
Hentschke P, Hagglund H, Mattsson J, Carlens S, Lonnqvist B, Ljungman P et al. Bilateral subdural haematomas following lumbar puncture in three haematopoietic stem cell transplant recipients. Bone Marrow Transplant 1999; 24: 1033–1035.
Weber C, Schaper J, Tibussek D, Adams O, Mackenzie CR, Dilloo D et al. Diagnostic and therapeutic implications of neurological complications following paediatric haematopoietic stem cell transplantation. Bone Marrow Transplant 2008; 41: 253–259.
Ferry C, Gemayel G, Rocha V, Labopin M, Esperou H, Robin M et al. Long-term outcomes after allogeneic stem cell transplantation for children with hematological malignancies. Bone Marrow Transplant 2007; 40: 219–224.
Flandin I, Hartmann O, Michon J, Pinkerton R, Coze C, Stephan JL et al. Impact of TBI on late effects in children treated by megatherapy for Stage IV neuroblastoma. A study of the French Society of Pediatric oncology. Int J Radiat Oncol Biol Phys 2006; 64: 1424–1431.
Acknowledgements
We thank Marianne Alverstrand for invaluable technical assistance and Jan Kowalski for excellent statistical assistance. This work was supported by Mary Béve Foundation for Pediatric Cancer Research, The Swedish Children Cancer Foundation, The Samariten Foundation and a Government Public Health Grant (ALF).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Rubin, J., Vettenranta, K., Vettenranta, J. et al. Use of intrathecal chemoprophylaxis in children after SCT and the risk of central nervous system relapse. Bone Marrow Transplant 46, 372–378 (2011). https://doi.org/10.1038/bmt.2010.121
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2010.121
Keywords
This article is cited by
-
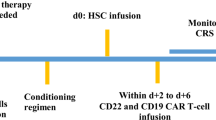
Intrathecal CAR-NK cells infusion for isolated CNS relapse after allogeneic stem cell transplantation: case report
Stem Cell Research & Therapy (2023)
-
Comparison of central nervous system relapse outcomes following haploidentical vs identical-sibling transplant for acute lymphoblastic leukemia
Annals of Hematology (2020)
-
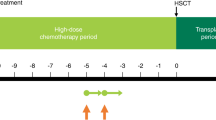
Safety of liposomal cytarabine CNS prophylaxis in children, adolescent and young adult hematopoietic stem cell transplant recipients with acute leukemia and non-Hodgkin lymphoma
Bone Marrow Transplantation (2016)