Abstract
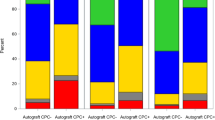
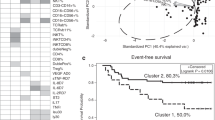
Relapsed disease remains a major obstacle following autologous haematopoietic SCT (HSCT) for non-Hodgkin's lymphoma (NHL) and multiple myeloma (MM). Studies regarding the importance of detectable tumour cells in PBSC collections have been inconclusive. Patients undergoing autologous HSCT for NHL and MM between 2001 and 2006 were enrolled (n=158). PBSC grafts were assessed for clonal IgH CDR3 gene rearrangements using qualitative semi-nested PCR. In comparison to patients with PCR-positive PBSC grafts, patients negative for detectable disease had no improvement in overall survival (OS) or PFS for MM (P=0.91 and 0.91) or NHL (P=0.82 and 0.85). Further, no significant difference in OS was observed between patients with PCR-positive compared with PCR-negative PBSC grafts with aggressive NHL histology (P=0.74) or indolent disease (P=0.29). Patients with contaminating tumour cells in autologous PBSCs do not have worsened OS or PFS in MM or NHL. Tumour cells detected by sensitive molecular methods in PBSC collections may be distinct from cells contaminating marrow and appear to have limited utility in identifying patients with MM and B-cell NHL who would benefit from purging strategies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Attal M, Harrousseau JL, Stoppa AM, Sotto JJ, Fuzibet JG, Rossi JF et al. A prospective randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma. N Engl J Med 1996; 335: 91–97.
Child JA, Morgan GJ, Davies FE, Owen RG, Bell SE, Hawkins K et al. High-dose chemotherapy with hematopoietic stem cell rescue for multiple myeloma. N Engl J Med 2003; 348: 1875–1883.
Philip T, Guglielmi C, Hagenbeek A, Somers R, van der Lelie H, Bron D et al. Autologous bone marrow transplantation as compared with salvage chemotherapy in relapses of chemotherapy-sensitive non-Hodgkin's lymphoma. N Engl J Med 1995; 333: 1540–1545.
Sharp JG, Kessinger A, Mann S, Crouse DA, Armitage JO, Bierman P et al. Outcome of high-dose therapy and autologous transplantation in non-Hodgkin's lymphoma based on the presence of tumor in the marrow or infused hematopoietic harvest. J Clin Oncol 1996; 14: 214–219.
Vose JM, Sharp G, Chan WC, Nichols C, Loh K, Inwards D et al. Autologous transplantation for aggressive non-Hodgkin's lymphoma: results of a randomized trial evaluating graft source and minimal residual disease. J Clin Oncol 2002; 20: 2344–2352.
Brown JR, Feng Y, Gribben JG, Neuberg D, Fisher DC, Mauch P et al. Long-term survival after autologous bone marrow transplantation for follicular lymphoma in first remission. Biol Blood Marrow Transplant 2007; 13: 1057–1065.
Ladetto M, Corradini P, Vallet S, Benedetti F, Vitolo U, Martelli M et al. High rate of clinical and molecular remissions in follicular lymphoma patients receiving high-dose sequential chemotherapy and autografting at diagnosis: a multicenter, prospective study by the Gruppo Italiano Trapianto Midollo Osseo (GITMO). Blood 2002; 100: 1559–1565.
Lopez-Perez R, Garcia-Sanz R, Gonzalez D, Balanzategui A, Chillon MC, Alaejos I et al. The detection of contaminating clonal cells in apheresis products is related to response and outcome in multiple myeloma undergoing autologous peripheral blood stem cell transplantation. Leukemia 2000; 14: 1493–1499.
Vogel W, Kopp HG, Kanz L, Einsele H . Myeloma cell contamination of peripheral blood stem-cell grafts can predict the outcome in multiple myeloma patients after high-dose chemotherapy and autologous stem-cell transplantation. J Cancer Res Clin Oncol 2005; 131: 214–218.
Demirkazik A, Kessinger A, Armitage JO, Bierman PJ, Lynch J, Vose J et al. Progenitor and lymphoma cells in blood stem cell harvests: impact on survival following transplantation. Bone Marrow Transplant 2001; 28: 207–212.
Stewart AK, Vescio R, Schiller G, Ballester O, Noga S, Rugo H et al. Purging of autologous peripheral-blood stem cells using CD34 selection does not improve overall or progression-free survival after high-dose chemotherapy for multiple myeloma: results of a multicenter randomized controlled trial. J Clin Oncol 2001; 19: 3771–3779.
Bourhis JH, Bouko Y, Koscielny S, Bakkus M, Greinix H, Derigs G et al. Relapse risk after autologous transplantation in patients with newly diagnosed myeloma is not related with infused tumor cell load and the outcome is not improved by CD34+ cell selection: long term follow-up of an EBMT phase III randomized study. Haematologica 2007; 92: 1083–1090.
Gribben JG, Freedman AS, Neuberg D, Roy DC, Blake KW, Woo SD et al. Immunologic purging of marrow assessed by PCR before autologous bone marrow transplantation for B-cell lymphoma. N Engl J Med 1991; 325: 1525–1533.
Freedman AS, Neuberg D, Mauch P, Soiffer RJ, Anderson KC, Fisher DC et al. Long-term follow-up of autologous bone marrow transplantation in patients with relapsed follicular lymphoma. Blood 1999; 94: 3325–3333.
Schouten HC, Qian W, Kvaloy S, Porcellini A, Haqberg H, Johnson HE et al. High-dose therapy improves progression-free survival and survival in relapsed follicular non-Hodgkin's lymphoma: results from the randomized European CUP trial. J Clin Oncol 2003; 21: 3918–3927.
Sukpanichnant S, Vnencak-Jones CL, McCurley TL . Determination of B-cell clonality in paraffin-embedded endoscopic biopsy specimens of abnormal lymphocytic infiltrates and gastrointestinal lymphoma by polymerase chain reaction. Am J Clin Pathol 1994; 102: 299–305.
Kaplan EL, Meier P . Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–481.
Durie BG, Harousseau JL, Miguel JS, Bladé J, Barlogie B, Anderson K et al. International uniform response criteria for multiple myeloma. Leukemia 2006; 20: 1467–1473.
Hamlin PA, Zelenetz PA, Kewalramani T, Qin J, Satogopan JM, Verbel D et al. Age-adjusted International Prognostic Index predicts autologous stem cell transplantation outcome for patients with relapsed or primary refractory diffuse large B-cell lymphoma. Blood 2003; 102: 1989–1996.
Vose JM, Bierman PJ, Loberiza FR, Lynch JC, Bociek GR, Weisenberger DD et al. Long-term outcomes of autologous stem cell transplantation for follicular non-Hodgkin lymphoma: effect of histological grade and Follicular International Prognostic Index. Biol Blood Marrow Transplant 2008; 14: 36–42.
Pennell N, Woods A, Reis M, Buckstein R, Spaner D, Imrie K et al. Association of clinical status of follicular lymphoma patients after autologous stem cell transplant and quantitative assessment of lymphoma in blood and bone marrow as measured by SYBR Green I polymerase chain reaction. J Mol Diagn 2006; 8: 40–50.
Narayamasami U, Kanteti R, Morelli J, Klekar K, Al-Olama A, Keating C et al. Randomized trial of filgrastim versus chemotherapy and filgrastim mobilization of hematopoietic progenitor cells for rescue in autologous transplantation. Blood 2001; 98: 2059–2064.
Sabloff M, Atkins HL, Bence-Bruckler I, Bredeson C, Fergusson D, Genest P et al. A 15-year analysis of early and late autologous hematopoietic stem cell transplant in relapsed, aggressive, transformed, and nontransformed follicular lymphoma. Biol Blood Marrow Transplant 2007; 13: 956–964.
Evans PA, Pott CH, Groenen PJ, Salles G, Davi F, Berger F et al. Significantly improved PCR-based clonality testing in B-cell malignancies by use of multiple immunoglobulin gene targets. Report of the BIOMED-2 Concerted Action BHM4-CT98-3936. Leukemia 2007; 21: 20–214.
van Dongen JJ, Langerak AW, Bruggemann M, Evans PA, Hummel M, Lavender FL et al. Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: report of the BIOMED-2 Concerted Action BMH4-CT98-3936. Leukaemia 2003; 17: 2257–2317.
Blystad AK, Delabie J, Kvaloy S, Holte H, Valerhaugen H, Ikonomou I et al. Infused CD34 cell dose, but not tumour cell content of peripheral blood progenitor cell grafts, predicts clinical outcome in patients with diffuse large B-cell lymphoma and follicular lymphoma grade 3 treated with high-dose therapy. Br J Haematol 2004; 105: 605–612.
Stewart AK, Sutherland DR, Nanji S, Zhao Y, Lutzko C, Nayar R et al. Engraftment of gene-marked hematopoietic progenitors in myeloma patients after transplant of autologous long-term marrow cultures. Hum Gene Ther 1999; 10: 1953–1964.
Dunbar CE, Cottler-Fox M, O'Shaugnessy JA, Doren S, Carter C, Berenson R et al. Retrovirally marked CD34-enriched peripheral blood and bone marrow cells contribute to long-term engraftment after autologous transplantation. Blood 1995; 85: 3048–3057.
Alici E, Bjorkstrand B, Treschow A, Aints I, Smith CI, Gharton G et al. Long-term follow-up of gene-marked CD34+ cells after autologous stem cell transplantation for multiple myeloma. Cancer Gene Ther 2007; 14: 227–232.
Acknowledgements
We acknowledge the support of Canadian Blood Services (CBS). DSA is an Adjunct Scientist at CBS. The database of the Blood and Marrow Transplant Program at The Ottawa Hospital received support from The Ottawa Hospital Foundation, BMT Research and Education Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ho, J., Yang, L., Banihashemi, B. et al. Contaminating tumour cells in autologous PBSC grafts do not influence survival or relapse following transplant for multiple myeloma or B-cell non-Hodgkin's lymphoma. Bone Marrow Transplant 43, 223–228 (2009). https://doi.org/10.1038/bmt.2008.318
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2008.318
Keywords
This article is cited by
-
Impact of residual tumor cells in the stem cell collection on multiple myeloma patients receiving autologous stem cell transplantation
Annals of Hematology (2023)
-
Stem cell mobilization in multiple myeloma: challenges, strategies, and current developments
Annals of Hematology (2023)
-
Secondary acute lymphoblastic leukemia is a distinct clinical entity with prognostic significance
Blood Cancer Journal (2017)
-
Reovirus as a successful ex vivo purging modality for multiple myeloma
Bone Marrow Transplantation (2014)
-
Autologous haematopoietic stem cell mobilisation in multiple myeloma and lymphoma patients: a position statement from the European Group for Blood and Marrow Transplantation
Bone Marrow Transplantation (2014)