Abstract
Background:
Circadian disruption caused by exposure to light at night (LAN) has been proposed as a risk factor for breast cancer and a reason for secular increases in incidence. Studies to date have largely been ecological or case-control in design and findings have been mixed.
Methods:
We investigated the relationship between LAN and breast cancer risk in the UK Generations Study. Bedroom light levels and sleeping patterns at age 20 and at study recruitment were obtained by questionnaire. Analyses were conducted on 105 866 participants with no prior history of breast cancer. During an average of 6.1 years of follow-up, 1775 cases of breast cancer were diagnosed. Cox proportional hazard models were used to calculate hazard ratios (HRs), adjusting for potential confounding factors.
Results:
There was no association between LAN level and breast cancer risk overall (highest compared with lowest LAN level at recruitment: HR=1.01, 95% confidence interval (CI): 0.88–1.15), or for invasive (HR=0.98, 95% CI: 0.85–1.13) or in situ (HR=0.96, 95% CI: 0.83–1.11) breast cancer, or oestrogen-receptor (ER) positive (HR=0.98, 95% CI: 0.84–1.14); or negative (HR=1.16, 95% CI: 0.82–1.65) tumours separately. The findings did not differ by menopausal status. Adjusting for sleep duration, sleeping at unusual times (non-peak sleep) and history of night work did not affect the results. Night waking with exposure to light, occurring around age 20, was associated with a reduced risk of premenopausal breast cancer (HR for breast cancer overall=0.74, 95% CI: 0.55–0.99; HR for ER-positive breast cancer=0.69, 95% CI: 0.49–0.97).
Conclusions:
In this prospective cohort analysis of LAN, there was no evidence that LAN exposure increased the risk of subsequent breast cancer, although the suggestion of a lower breast cancer risk in pre-menopausal women with a history of night waking in their twenties may warrant further investigation.
Similar content being viewed by others
Main
Breast cancer is the most common cancer diagnosed in women worldwide and incidence continues to rise. Internationally, the highest rates are seen in economically developed countries (DeSantis et al, 2015). This pattern of incidence, coupled with observations from migration studies (Ziegler et al, 1993; Deapen et al, 2002), is consistent with a strong role for lifestyle and environmental factors influencing breast cancer risk.
In 1978 Cohen et al (1978) suggested that disruption to circadian rhythm could result in higher circulating oestrogen levels and thereby increase the risk of breast cancer, and in 1987 Stevens (Stevens, 1987) proposed that secular trends in breast cancer incidence might be explained by increasing exposure to artificial light. The hypothesised mechanism is via melatonin, a hormone secreted by the pineal gland in response to decreases in ambient light (Huether, 1993; Brainard et al, 2001).
This ‘light at night’ (LAN) theory has stimulated epidemiological investigations. To date, most studies have been either ecological in design, correlating cancer incidence rates in populations with estimates of outdoor ambient LAN (Kloog et al, 2008, 2010; Kim et al, 2016), or case-control studies, examining risks associated with self-reported measures of indoor LAN (Davis et al, 2001; O'Leary et al, 2006; Bauer et al, 2013). These have disadvantages in that the former do not analyse on an individual basis and the latter have potential for recall and selection biases. Only one cohort study has been published, which found an increased risk in relation to outdoor LAN, measured by satellite, but not indoor LAN, measured by questionnaire (Hurley et al, 2014). Overall, epidemiological findings have been inconsistent, and the metrics analysed have varied and not been clearly comparable (O'Leary et al, 2006; Bauer et al, 2013; Hurley et al, 2014).
Here we report a cohort study of the relationship between LAN and subsequent breast cancer risk, based on data from women recruited to the UK Generations Study.
Methods
Study population
This analysis is based on the Generations Study (GS), a cohort study of >113 000 women from the UK, recruited at ages ⩾16 years since 2003. Recruitment involved a baseline postal questionnaire about established and potential breast cancer risk factors, and donation of a blood sample. Participants are followed up approximately every 3 years, by postal or online questionnaires, to obtain updated risk factor and outcome information (further detail in Swerdlow et al, 2011). The study was undertaken with informed consent and ethics approval from the South East Multi-Centre Research Ethics Committee.
Cancers occurring in the cohort were identified from recruitment and follow-up questionnaires, spontaneous reports to the study centre, and ‘flagging’ at the National Health Service Central Registers, virtually complete registers of the population of the country, which notify cancer registrations, deaths and emigrations in study subjects to authorised medical researchers. Confirmation of self-reported cancer diagnoses was obtained from medical records.
Exposure assessment
Information on LAN and sleep patterns in GS participants was obtained at recruitment. Women were asked to report their level of exposure to LAN over the year prior to recruitment and at age 20 years, in the room in which they slept, in the categories; ‘light enough to read’; ‘light enough to see across the room, but not read’; ‘light enough to see your hand in front of you, but not to see across the room’; and ‘too dark to see your hand, or you wear a mask’.
Covariate information
Detailed information on established breast cancer risk factors was collected by the GS at recruitment and was updated, where applicable, at follow-up rounds (Swerdlow et al, 2011). Information on history of night shift work (defined as work between 2200 and 0700 hours) obtained at baseline was used to derive a dichotomous variable for ever/never night work during the 10 years before recruitment. The average number of times GS participants woke during the night and put on a light or entered a bright room over the year prior to recruitment and at age 20 years was collected at baseline. Non-peak sleep (Davis et al, 2001) was assessed as going to sleep at or after 0200 hours or rising for the day at or before 0100 hours. GS participants were also asked about average sleep duration, which was used to derive a dichotomous variable <7 h vs ⩾7 h sleep per night, based on median sleep in the GS cohort and thresholds used in other studies (Verkasalo et al, 2005; Pinheiro et al, 2006; Kakizaki et al, 2008).
Statistical analysis
The current analytic cohort is based on all women who were recruited to the study during June 2003 to June 2012 inclusive, and who had not previously been diagnosed with breast cancer. Follow-up for breast cancer started at the date of receipt of the recruitment questionnaire and ended on the earliest of: breast cancer, death, date of mailing for follow-up questionnaires, or if the follow-up questionnaire was not returned and the woman was covered by ‘flagging’, the earliest of the date the individual’s ‘flagging’ coverage ended (i.e., when she was removed from the NHS Central Register), or the date after which ‘flagging’ notification was not yet complete (taken to be 1 March 2014). If the follow-up questionnaire was not returned and the woman was not covered by ‘flagging’ (<1.2% of the cohort), the follow-up was truncated at the date of her last returned questionnaire.
Only a small proportion of women reported LAN in the lightest category (‘light enough to read’; 0.96% for the year before recruitment and 1.92% at age 20). This group was therefore combined with the adjacent group (‘light enough to see across the room, but not read’). Cox proportional hazards regression (Cox, 1972) using attained age as the implicit timescale was used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for breast cancer risk in relation to LAN exposure. To control for potential confounding by other breast cancer risk factors, we adjusted for year of birth, history of benign breast disease, history of breast cancer in a first-degree relative, socioeconomic score, age at menarche, age at first birth, parity, duration of breastfeeding, oral contraceptive (OC) use before menopause, hormone replacement therapy (HRT) use, menopausal status, age at menopause, pre-menopausal and post-menopausal body mass index, alcohol consumption, smoking and leisure time physical activity (in metabolic equivalents, METS, hours per week), with time-varying data incorporated for age at first birth, parity, menopausal status, age at menopause, OC use and HRT use. Socioeconomic score was based on place of residence (Acorn scores; Solutions CI, 2002).
Results are presented by oestrogen-receptor (ER) status of breast cancer and menopausal status during follow-up. Age at menopause was assumed to be 50 years for women whose menopausal status or age at menopause was not known. Analyses presented in the tables are for invasive plus in situ breast cancer combined, but we also conducted analyses separately for invasive and in situ disease and for broad morphological groups (ductal, lobular, other/not known), which are reported in the text. Analyses were also adjusted for ever night shift work, sleep duration, and non-peak sleep to investigate their potential impact.
All statistical tests were performed using Stata/IC version 14.0 (StataCorp, 2015) and all reported P-values were two-sided.
Results
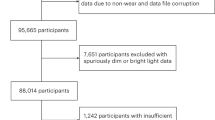
Of the 113 207 women recruited to the GS during June 2003 – June 2012, 6581 were excluded from analysis because of prior breast cancer, 14 due to prior bilateral mastectomy and 746 due to missing LAN information, leaving 105 866 women included in the analysis. Their mean age at recruitment was 46.5 years (range 16–102 years) and mean follow-up was 6.1 years (standard deviation=1.0). Follow-up by questionnaire (96.3%) or ‘flagging’ (1.7%) was complete for 98% of women, 0.8% (n=809) had died and 1.2% (n=1323) were lost to follow-up (e.g., by emigration). During follow-up, 1775 breast cancers (1503 invasive and 272 in situ) were diagnosed. ER status was ascertained for 99% of invasive and 58% of in situ cases; the latter was lower because hormone receptor assays are often not undertaken for in situ lesions in the UK. Histology was ascertained for 95% of cases. Further details of breast cancer cases are described in Supplementary Table 1.
Characteristics of the cohort are shown in Table 1. Women from earlier birth cohorts tended to report lower LAN levels, but overall, ‘medium’ levels of LAN were the most common, reported by 49% of participants for the year before recruitment and 47% of participants for age 20. Overall, 97% (n=102 972) of participants in this analysis reported LAN information at age 20. A greater proportion of women reported waking at night and turning on lights or going into a bright room during the year before recruitment than at age 20 (37% vs 10%, respectively, P<0.001). Seventeen percent of participants reported a history of night shift work during the 10 years before recruitment (we did not have consistent information on shift work before that).
There was no statistically significant association between breast cancer risk and LAN level in the year before recruitment or at age 20, when adjusted for age and year of birth. The HR for the highest LAN compared with the lowest LAN category at recruitment was 1.01 (95% CI: 0.88–1.15; Table 2) and for LAN at age 20 was 1.00 (95% CI: 0.88–1.15; Table 3). For pre-menopausal breast cancer, the adjusted HR for the highest vs lowest LAN level at recruitment was 1.00 (95% CI: 0.81–1.24) and at age 20 was 0.91 (95% CI: 0.73–1.13). Similarly, there was no significant association between LAN and breast cancer risk when the analysis was limited to post-menopausal follow-up (Table 2). Analyses in relation to ER sub-type showed no association: for LAN at recruitment, the HR for ER-positive breast cancer was 0.98 (95% CI: 0.84–1.14) and for ER-negative disease was 1.16 (95% CI: 0.82–1.65).
When analyses were repeated to investigate the risk of invasive and in situ breast cancer separately, results were very similar to those for breast cancer overall: HR=0.98 (95% CI: 0.85–1.13) for invasive and HR=0.96 (95% CI: 0.83–1.11) for in situ breast cancer for the highest vs lowest LAN level at recruitment (not in Table). Similarly, there was no association between LAN and the risk of different morphological subtypes of breast cancer: for the highest vs lowest level LAN at recruitment, ductal HR=1.00 (95% CI: 0.86–1.16), lobular HR=0.92 (95% CI: 0.66–1.28) and other types HR=1.41 (95% CI: 0.85–2.35) (not in Table).
There was no relationship between reported night waking with exposure to light in the year before recruitment and risk of breast cancer (HR=1.01, 95% CI: 0.92–1.12; Table 4). Similarly, there was no association between this exposure and breast cancer risk in pre- or post-menopausal women and results did not differ by ER status of breast cancer. For night waking with light exposure at age 20, however, there was a reduced risk of pre-menopausal breast cancer (HR=0.74, 95% CI: 0.55–0.99, P=0.04; Table 5), with a reduced risk of ER-positive (HR=0.69, 95% CI: 0.49–0.97, P=0.03), but not ER-negative (HR=0.91, 95% CI: 0.45–1.82) cancers and no effect for post-menopausal breast cancer.
There was no impact on our results when analyses comparing the highest LAN vs lowest LAN categories at recruitment were adjusted for history of night shift work in the 10 years before recruitment (HR=1.01, 95% CI: 0.88–1.15), duration of sleep (HR=1.01, 95% CI: 0.89–1.15) or non-peak sleep (HR=1.01, 95% CI: 0.88–1.15) (not in Table).
Discussion
It has been hypothesised that suppression of nocturnal pineal melatonin production in response to LAN might explain the rises in breast cancer rates that have accompanied industrialisation and electrification in westernised countries (Stevens, 1987). Exposure to artificial light during the night can disrupt the circadian rhythm and reduce the normal nocturnal rise in melatonin (Stevens, 1987; Stevens and Rea, 2001; Claustrat et al, 2005; Stevens et al, 2007; Straif et al, 2007), leading to an increase in circulating oestrogen levels (Cohen et al, 1978; Cos and Sanchez-Barcelo, 2000) and suppression of tumour anti-proliferative processes, which might increase breast cancer risk (Stevens, 1987; Stevens and Rea, 2001; Hill et al, 2015).
Clearly, if circadian disruption of melatonin plays a substantial role in the aetiology of breast cancer, it is of major public health importance. Following early epidemiologic studies (Davis et al, 2001; Hansen, 2001; Schernhammer et al, 2001; O'Leary et al, 2006), the World Health Organisation has designated night shift work involving LAN-induced circadian/melatonin disruption as a probable carcinogen (class 2a) and risk factor for the development of breast cancer (Straif et al, 2007). In Denmark this led to a change to occupational compensation law (Wise, 2009).
In our analysis of over 105 000 UK women, we found no evidence of a relationship between self-reported level of domestic exposure to LAN and subsequent raised risk of breast cancer. Published ecological studies using satellite data to derive LAN exposure in Israel, South Korea and worldwide have tended to show high light levels associated with a 30–70% increased risk of breast cancer (Kloog et al, 2008; 2010; Kim et al, 2016). Findings from case-control studies conducted in a number of countries have been more mixed. Using self-reported bedroom LAN data, several studies found statistically non-significant increased risks ranging from 10 to 50% (Davis et al, 2001; O'Leary et al, 2006; Li et al, 2010; Keshet-Sitton et al, 2016). Statistically significant increased risks of 10–20% have, however, been reported by case-control studies of LAN exposure in Israel (Kloog et al, 2011) and the US (Bauer et al, 2013). Ecological and case-control study designs have disadvantages, however: potential confounding by other factors affecting breast cancer risk, inability to link exposure directly to individual outcome in ecological studies, and potential selection and recall biases in case-control studies. Cohort studies provide a mechanism for avoiding these deficiencies. To the best of our knowledge, the only previously published cohort study was that by Hurley et al (2014) among teachers in California. That analysis of 106 731 female Californian teachers found an increased risk of breast cancer for women living in areas with the highest quintile of estimated outdoor LAN exposure as assessed from satellite data, but no effect of indoor LAN assessed from questionnaire responses incorporating duration of use.
When we examined LAN effects in pre- and post-menopausal women separately, we found no difference in breast cancer risk in relation to bedroom light level by menopausal status. A small number of published studies investigated risk by menopausal status. In the only cohort study (Hurley et al, 2014), there was a more pronounced risk of breast cancer associated with outdoor LAN in pre-menopausal than post-menopausal women, while in case-control studies, Li et al (2010) observed a non-significant increased risk in post-menopausal women only and O'Leary et al (2006) found similar LAN effects irrespective of menopausal status.
In addition to LAN, a range of other exposure variables have been used to assess potential disruption to circadian rhythm, such as duration of sleep, non-peak sleep, night waking with exposure to light, and night shift work (Davis et al, 2001; Schernhammer et al, 2001; O'Leary et al, 2006; Straif et al, 2007; Li et al, 2010; Qian et al, 2015; Keshet-Sitton et al, 2016). There is a potential interplay between these variables and LAN. For example, people who have difficulty sleeping may spend more time awake with a light on during the night. Similarly, non-peak sleep may result in increased exposure to artificial light during the hours of natural darkness. In our study, there was still no association between LAN exposure and risk of breast cancer after adjustment for average sleep duration and nonpeak sleep. Likewise, after adjustment for history of night shift work in the 10 years before recruitment, we found no association between bedroom LAN and risk of breast cancer. Studies have shown that intermittent nocturnal light exposure of sufficient intensity lowers melatonin levels (Bojkowski et al, 1987; Brzezinski, 1997; Travlos et al, 2001). In our study, we found self-reported night waking with light exposure at age 20 was associated with a decreased risk of pre-menopausal breast cancer, particularly ER-positive cancer. Epidemiological investigations of night waking that leads to light exposure have had mixed findings: one study (Davis et al, 2001) found no relation, while another (O'Leary et al, 2006) found a significant 65% increase in breast cancer risk.
Major strengths of our study are its prospective design, large study population size, comprehensive assessment of breast cancer risk factors and very high follow-up rates. The detailed information on established breast cancer risk factors available within the GS allowed us to adjust for a wide range of potentially confounding factors in our analyses. The Californian Teachers cohort study and most case-control studies have adjusted for the major recognised breast cancer risk factors, but few ecological studies, with the exception of Kloog et al (2008) have been adjusted for potential confounders. Our study also has the advantage of having information on reported LAN at age 20.
LAN reflects the degree of exposure to internal lights left on at night, plus both the extent of external light (natural and artificial) and the extent of window covering blocking light entry. The LAN measure we used takes in all of these factors, whereas a residential address only gives potential information on external light. Thus a woman in a dark rural area with no street lighting might nevertheless leave her bedroom light on at night and sleep with high LAN, and a woman in a city centre might use shutters or blinds to keep out external light and hence sleep in total darkness. A potential limitation of our study is that it uses self-reported LAN exposure information. However, since this information was ascertained before breast cancer occurrence, it should not have biased the results. Misclassification would be likely to have diluted any true relation, but the lack of any sign of raised risk does not suggest a relationship.
In conclusion, we found no evidence of an association between LAN exposure and raised risk of breast cancer in this large UK-based cohort study. Although our findings raise the possibility of a protective effect in pre-menopausal women who reported night waking with exposure to light at age 20, this was a subset analysis with modest statistical significance, based on relatively few breast cancer cases, has not been reported elsewhere, and has no plausible mechanism, so cannot be taken as strong evidence unless confirmed independently.
References
Bauer SE, Wagner SE, Burch J, Bayakly R, Vena JE (2013) A case-referent study: light at night and breast cancer risk in Georgia. Int J Health Geogr 12: 23.
Bojkowski CJ, Aldhous ME, English J, Franey C, Poulton AL, Skene DJ, Arendt J (1987) Suppression of nocturnal plasma melatonin and 6-sulphatoxymelatonin by bright and dim light in man. Horm Metab Res 19 (9): 437–440.
Brainard GC, Hanifin JP, Greeson JM, Byrne B, Glickman G, Gerner E, Rollag MD (2001) Action spectrum for melatonin regulation in humans: evidence for a novel circadian photoreceptor. J Neurosci 21 (16): 6405–6412.
Brzezinski A (1997) Melatonin in humans. N Engl J Med 336 (3): 186–195.
Claustrat B, Brun J, Chazot G (2005) The basic physiology and pathophysiology of melatonin. Sleep Med Rev 9 (1): 11–24.
Cohen M, Lippman M, Chabner B (1978) Role of pineal gland in aetiology and treatment of breast cancer. Lancet 2 (8094): 814–816.
Cos S, Sanchez-Barcelo EJ (2000) Melatonin and mammary pathological growth. Front Neuroendocrinol 21 (2): 133–170.
Cox DR (1972) Regression models and life-tables. J R Stat Soc B 34 (2): 187–220.
Davis S, Mirick DK, Stevens RG (2001) Night shift work, light at night, and risk of breast cancer. J Natl Cancer Inst 93 (20): 1557–1562.
Deapen D, Liu L, Perkins C, Bernstein L, Ross RK (2002) Rapidly rising breast cancer incidence rates among Asian-American women. Int J Cancer 99 (5): 747–750.
DeSantis CE, Bray F, Ferlay J, Lortet-Tieulent J, Anderson BO, Jemal A (2015) International variation in female breast cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev 24 (10): 1495–1506.
Hansen J (2001) Increased breast cancer risk among women who work predominantly at night. Epidemiology 12 (1): 74–77.
Hill SM, Belancio VP, Dauchy RT, Xiang S, Brimer S, Mao L, Hauch A, Lundberg PW, Summers W, Yuan L, Frasch T, Blask DE (2015) Melatonin: an inhibitor of breast cancer. Endocr Relat Cancer 22 (3): R183–R204.
Huether G (1993) The contribution of extrapineal sites of melatonin synthesis to circulating melatonin levels in higher vertebrates. Experientia 49 (8): 665–670.
Hurley S, Goldberg D, Nelson D, Hertz A, Horn-Ross PL, Bernstein L, Reynolds P (2014) Light at night and breast cancer risk among California teachers. Epidemiology 25 (5): 697–706.
Kakizaki M, Kuriyama S, Sone T, Ohmori-Matsuda K, Hozawa A, Nakaya N, Fukudo S, Tsuji I (2008) Sleep duration and the risk of breast cancer: the Ohsaki Cohort Study. Br J Cancer 99 (9): 1502–1505.
Keshet-Sitton A, Or-Chen K, Yitzhak S, Tzabary I, Haim A (2016) Light and the city: breast cancer risk factors differ between urban and rural women in Israel. Integr Cancer Ther 16 (2): 176–187.
Kim YJ, Park MS, Lee E, Choi JW (2016) High incidence of breast cancer in light-polluted areas with spatial effects in Korea. Asian Pac J Cancer Prev 17 (1): 361–367.
Kloog I, Haim A, Stevens RG, Barchana M, Portnov BA (2008) Light at night co-distributes with incident breast but not lung cancer in the female population of Israel. Chronobiol Int 25 (1): 65–81.
Kloog I, Portnov BA, Rennert HS, Haim A (2011) Does the modern urbanized sleeping habitat pose a breast cancer risk? Chronobiol Int 28 (1): 76–80.
Kloog I, Stevens RG, Haim A, Portnov BA (2010) Nighttime light level co-distributes with breast cancer incidence worldwide. Cancer Causes Control 21 (12): 2059–2068.
Li Q, Zheng T, Holford TR, Boyle P, Zhang Y, Dai M (2010) Light at night and breast cancer risk: results from a population-based case-control study in Connecticut, USA. Cancer Causes Control 21 (12): 2281–2285.
O'Leary ES, Schoenfeld ER, Stevens RG, Kabat GC, Henderson K, Grimson R, Gammon MD, Leske MC (2006) Shift work, light at night, and breast cancer on Long Island, New York. Am J Epidemiol 164 (4): 358–366.
Pinheiro SP, Schernhammer ES, Tworoger SS, Michels KB (2006) A prospective study on habitual duration of sleep and incidence of breast cancer in a large cohort of women. Cancer Res 66 (10): 5521–5525.
Qian X, Brinton LA, Schairer C, Matthews CE (2015) Sleep duration and breast cancer risk in the Breast Cancer Detection Demonstration Project follow-up cohort. Br J Cancer 112 (3): 567–571.
Schernhammer ES, Laden F, Speizer FE, Willett WC, Hunter DJ, Kawachi I, Colditz GA (2001) Rotating night shifts and risk of breast cancer in women participating in the nurses' health study. J Natl Cancer Inst 93 (20): 1563–1568.
Solutions CI (2002) ACORN; the complete consumer classification. Solutions CI: London.
StataCorp (2015) Stata Statistical Software: Release 14. StataCorp: College Station, TX.
Stevens RG (1987) Electric power use and breast cancer: a hypothesis. Am J Epidemiol 125 (4): 556–561.
Stevens RG, Blask DE, Brainard GC, Hansen J, Lockley SW, Provencio I, Rea MS, Reinlib L (2007) Meeting report: the role of environmental lighting and circadian disruption in cancer and other diseases. Environ Health Perspect 115 (9): 1357–1362.
Stevens RG, Rea MS (2001) Light in the built environment: potential role of circadian disruption in endocrine disruption and breast cancer. Cancer Causes Control 12 (3): 279–287.
Straif K, Baan R, Grosse Y, Secretan B, El GF, Bouvard V, Altieri A, Benbrahim-Tallaa L, Cogliano V (2007) Carcinogenicity of shift-work, painting, and fire-fighting. Lancet Oncol 8 (12): 1065–1066.
Swerdlow AJ, Jones ME, Schoemaker MJ, Hemming J, Thomas D, Williamson J, Ashworth A (2011) The Breakthrough Generations Study: design of a long-term UK cohort study to investigate breast cancer aetiology. Br J Cancer 105 (7): 911–917.
Travlos GS, Wilson RE, Murrell JA, Chignell CF, Boorman GA (2001) The effect of short intermittent light exposures on the melatonin circadian rhythm and NMU-induced breast cancer in female F344/N rats. Toxicol Pathol 29 (1): 126–136.
Verkasalo PK, Lillberg K, Stevens RG, Hublin C, Partinen M, Koskenvuo M, Kaprio J (2005) Sleep duration and breast cancer: a prospective cohort study. Cancer Res 65 (20): 9595–9600.
Wise J (2009) Danish night shift workers with breast cancer awarded compensation. BMJ 338: b1152.
Ziegler RG, Hoover RN, Pike MC, Hildesheim A, Nomura AM, West DW, Wu-Williams AH, Kolonel LN, Horn-Ross PL, Rosenthal JF, Hyer MB (1993) Migration patterns and breast cancer risk in Asian-American women. J Natl Cancer Inst 85 (22): 1819–1827.
Acknowledgements
We thank Breast Cancer Now and The Institute of Cancer Research for support and funding of the Generations Study, and the study participants, study staff, and the doctors, nurses, and other health-care providers and health information sources who have contributed to the study. The ICR acknowledges NHS funding to the Royal Marsden/ICR NIHR Biomedical Research Centre.
5Current address: Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford OX2 6GG, UK.
6Current address: UCSF Helen Diller Family Comprehensive Cancer Center, San Francisco, CA 94158, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
This work is licensed under the Creative Commons Attribution 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Johns, L., Jones, M., Schoemaker, M. et al. Domestic light at night and breast cancer risk: a prospective analysis of 105 000 UK women in the Generations Study. Br J Cancer 118, 600–606 (2018). https://doi.org/10.1038/bjc.2017.359
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2017.359
Keywords
This article is cited by
-
Light at night and risk of breast cancer: a systematic review and dose–response meta-analysis
International Journal of Health Geographics (2021)
-
Exposure to artificial light at night and risk of cancer: where do we go from here?
British Journal of Cancer (2021)
-
Night shift work and risk of breast cancer in women: the Generations Study cohort
British Journal of Cancer (2019)
-
Comment on ‘Domestic light at night and breast cancer risk: a prospective analysis of 105000 UK women in the Generations Study’
British Journal of Cancer (2019)
-
Response to ‘Comment on ‘Domestic light at night and breast cancer risk: a prospective analysis of 105 000 UK women in the Generations Study”
British Journal of Cancer (2019)