Abstract
Background:
First Spanish trial of Ewing sarcoma (ES) including adults and children with the aim to test the efficacy of Gemcitabine and Docetaxel (G/D) in newly diagnosed high-risk (HR) patients.
Methods:
This was a prospective, multicentric, non-randomised, open study for patients ⩽40 years with newly diagnosed ES. HR patients (metastatic, axial-pelvic primaries or bone marrow micrometastasis) received 2 window cycles of G/D. Patients with an objective response (OR) to G/D received 12 monthly cycles of G/D after completion of mP6. The primary end point was the OR rate to the G/D window phase and the event-free survival (EFS) and overall survival (OS) for all patients. The study is registered at ClinicalTrials.gov (identifier: NCT00006734).
Results:
Forty-three patients were enroled, median age 17 years (range, 3–40). After a median follow-up of 43.4 months, the 5-year OS rate is 55.0% (95% CI, 41–74%) with an EFS of 50.0% (95% CI, 36–68%). The 5-year OS and EFS rates for standard risk (SR) patients was 76.0% (95% CI, 57–100%) and 71.0% (CI, 54–94%); for HR 36.0% (CI, 20–65%) and 29.0% (CI, 15–56%). Twelve of 17 (70.6%) high-risk (HR) patients showed an OR (7 PR and 5 SD) to G/D window therapy. The 5-year OS rate for patients ⩽18 years of age was 74.0% (CI, 56–97%) and 31.0% for >18 years (95% CI, 15–66%), P<0.001. Grade 4 adverse events during mP6 occurred in 28/39 of patients (72%) and did not correlate with age. Multivariate survival analyses with <18 vs ⩾18 and risk groups significant differences, P<0.00001. Using a Cox model for OS, both age and risk group were statistically significant (P=0.0011 and P=0.0065, respectively).
Conclusions:
Age at diagnosis is an independent prognostic factor superior to the presence of metastases with 18 years as the strongest cut-off. The mP6 regimen provided survival curves that plateau at 3 years and G/D produced significant responses in HR-ES that is worth further exploring.
Similar content being viewed by others
Main
Ewing sarcoma (ES) is an exclusively human, aggressive and poorly differentiated tumour, typically arising from bone and soft tissues in children, adolescents and young adults (AYA). It is characterised by reciprocal translocations that result in the fusion of the EWS RNA binding protein 1 (EWSR1) to an ETS transcription factor, EWSR1–FLI1 being the most common chimera (Delattre et al, 1992; Sorensen et al, 1994). ES is reported to be the second most common bone malignancy in AYA (after osteosarcoma), with an average annual incidence rate of 2.9 per million (Hawkins et al, 2011). In Spain, according to the national Spanish paediatric tumour registry (RNTI), the annual incidence rate of ES is 5.2 per million between the ages of 0 and 14 years, almost twice as high as osteosarcoma (3.5 per million), the most common bone malignancy in the paediatric age range (Peris-Bonet et al, 2010).
Treatment of ES improved over the decades of the 1980s and 90s, with reported durable remissions in 50.0–70.0% of non-metastatic patients (Rodriguez-Galindo et al, 2006). In 1995, the MSKCC group published the P6 protocol showing a successful induction of remission in patients with non-metastatic disease (Kushner et al, 1995). An extended outcome data showed 4-year event-free survival (EFS) and overall survival (OS) of 82.0% and 89.0%, respectively. Patients with metastatic disease at diagnosis had a significantly worse prognosis, with 4-year EFS rate of 12.0% and OS of 17.8% (Kolb et al, 2003). In 2001, we modified the original P6 (hereby mP6) protocol (Mora et al, 2011) and the results of a single-institution study with 31 patients showed 4-year EFS rate for non-metastatic cases of 83.0% and OS of 92.0%. Patients with metastatic disease showed 3-year EFS rate of 28.0% and OS of 42.0% (Mora et al, 2011).
Hensley et al (2002) reported the combination of gemcitabine (G) followed by docetaxel (D) for patients with leiomyosarcoma. The regimen consisted of gemcitabine at a dose of 900 mg m−2 given over 90 min on days 1 and 8 followed by docetaxel at a dose of 100 mg m−2 on day 8 given over 1 h IV (herein called G/D protocol). A subsequent study (Leu et al, 2004) in a variety of histologic subtypes of adult sarcomas (including Ewing) using G/D but lower dosages of gemcitabine (675 mg m−2) showed an overall response rate of 43%. Navid et al (2008) reported their experience with G/D in relapsed sarcomas including 6 ES and in 2009 we reported our single-institution experience including 6 ES patients at relapse (Mora et al, 2009). Overall, the G/D regimen, as initially described, has demonstrated significant anti-tumour activity against advanced ES (Leu et al, 2004; Navid et al, 2008; Mora et al, 2009; Rapkin et al, 2012).
The GEIS-21 study was designed to test whether the mP6 results could be reproduced in the setting of a multi-institutional trial including adults and children within the GEIS consortium; and to formally evaluate the anti-tumour activity of the G/D regimen in newly diagnosed, previously untreated, high-risk (HR) ES patients.
Patients and methods
Patients
GEIS-21 was opened to 10 member institutions of the Spanish Sarcoma group (GEIS) between April 2010 and November 2014. Eligible patients were 40 years or younger at enrolment and had diagnosis of ES confirmed by EWSR1 rearrangement by FISH or qRT-PCR analysis. All patients were required to have 2–4 bone marrow (BM) aspirates for centralised study (CdT, Hospital Sant Joan de Déu) of (micro)metastasis according to the methods previously described (Mora et al, 2011). HR-ES was defined as patients presenting with metastasis, primary tumour in the pelvis or axial skeleton, and patients with BM (micro)metastasis. Patients not fulfilling any of the prior criteria were considered standard risk (SR). Eligibility requirements included normal liver, renal and cardiac function, and ECOG 0–1. All patients/guardians gave written informed consent according to institutional guidelines, and the protocol was approved by the institutional review boards at all participating centres.
Study design
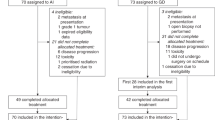
Patients were assigned to the treatment arm according to their risk group. In the SR group, assuming that the 3-year EFS may be increased by 20% (60–80%), with a confidence level of 0.1 and a statistical power of 80%, 22 patients were needed. Likewise, in the HR group, assuming that the 3-year EFS may be increased by 20% (10 to 30%), for the same confidence level and statistical power, 21 patients were needed.
A summary of chemotherapy details and road map is shown in Figure 1. Radiotherapy (RT) was scheduled after completion of all chemotherapy. SR patients with complete surgical resection, pathology-proven free margins (bone at least 1 cm; soft tissue at least 0.5 cm) and >90% tumour necrosis (TN), did not receive RT. Patients with unresectable tumours, inadequate margins or TN<90% received 40–45 Gy for microscopic margins and 50–56 Gy for gross residual disease. All radiation therapy was to be given in 1.8-Gy fractions.
Treatment details and road map. The mP6 regimen consisted of cycles 1, 2 and 4 with cyclophosphamide 4.2 g m−2, doxorubicin 75 mg m−2 and vincristine 2 mg m−2 (CDV); and cycles 3 and 5 with ifosfamide 9 g m−2 and etoposide 500 mg m−2 (IE). Doxorubicin was administered in 1 h infusion after administration of dexrazoxane (CardioxaneR) at 10 : 1 dose of doxorubicin. In April of 2012 an amendment to the protocol was approved after the EMA recommendation to contraindicate dexrazoxane in patients less than 18 years. Thereafter, patients less than 18 years received Doxorubicin in 4 h infusion with no prior Dexrazoxane. After each cycle of chemotherapy, granulocyte colony-stimulating factor was used to shorten the duration of neutropaenia. Whenever possible, surgical resection was performed after cycle 3 of chemotherapy. RT was given after mP6 chemotherapy. HR patients received gemcitabine 1000 mg m−2 iv over 90 min on day 1 and day 8, and docetaxel 100 mg m−2 over 2–4 h on day 8 of a 21-day cycle, 2 cycles (G+D regimen). The duration of docetaxel infusion was initially over 2 h and subsequently determined based upon the myelosuppression effect. If the patient recovered rapidly before the 21-day cycle, the infusion was prolonged up to 4 h. Prophylactic medications were provided on days 1 and 8 with IV ondansetron and on day 8 IV ranitidine, diphenhydramine and dexamethasone. All patients received filgrastim 5 μg kg−1 subcutaneously once a day from day 9 until haematological recovery.
Patients assigned to the HR group received a window phase of G/D as previously reported (Mora et al, 2009) prior to the mP6 regimen, with details of the regimen provided in Figure 1. Response to the G/D regimen was determined by imaging of the primary tumour using the RECIST 1.1 criteria as well as quantitative assessment of BM disease in at least 2 BM aspirates. BM studies were centralised to HSJD and independent radiological review was performed by one board certified musculoskeletal radiologist. At the end of mP6, the HR patients showing an objective response (OR: CR, PR or SD) to the G/D window phase, and received 12 monthly G/D cycles as maintenance. During maintenance patients were assessed every 3 months. SR patients were assessed every 3 months the first year and all patients were assessed every 6 months the second year and once a year after the third year.
Statistical analysis
The final statistical analysis was planned for 6.1 years after the first enrolment, May 2016. The primary study end point was to determine the OR rate to the G/D window phase for HR and EFS, and OS for all patients. EFS was defined as the time from entry onto the study until the first occurrence of relapse, progression, diagnosis of a second malignancy, death or, if no events occurred, until the last contact. OS was defined as the time from entry onto the study until death or, if it did not happen during the follow-up, until last contact. Patients who had not experienced an event by the date of last follow-up were censored.
Survival was evaluated using the Kaplan–Meier estimator (Kaplan and Meier, 1958). The log-rank test was used to compare the risk of an adverse event or death between groups (Greenwood, 1926; Cox, 1972; Kalbfleisch and Prentice, 1980). Cox proportional hazards model was used to perform multivariate survival analyses. Hazard ratios and their corresponding confidence intervals were derived from that model (Cox, 1972). The Holm-Bonferroni method was used to adjust P-values when performing multiple comparisons (Holm, 1979). We used the Contal and O’Quigley method to determine a cut-off value of the continuous variable age (Contal and O'Quigley, 1999). Comparisons of continuous variables among groups were performed using the Mann–Whitney test.
All P-values lower than 0.05 were considered to be statistically significant. Statistical analyses were carried out using R software version 3.3.1 (R Core Team, 2016).
Results
Patient characteristics
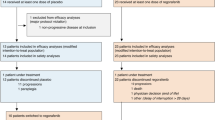
From April 2010 to November 2014, 43 patients with newly diagnosed ES and EWSR1 tumour rearrangement were enroled. Patient’s characteristics are summarised in Table 1. Thirty-two patients (74.4%) were male, and eleven (25.6%) female; a male to female ratio of 3 : 1, reflecting the well-described male predominance of ES (Hawkins et al, 2011). The median age at study entry was 17 years (range, 3–40 years); 12.5 years for SR and 18 years for HR, P=0.068. Screening for micrometastatic disease in the BM was performed in 41 of the 43 (95.3%) patients. Metastasis at diagnosis was present in 10 cases (23.0%); 6 (60.0%) in the lung; 3 (30.0%) in the bone or BM compartment; and 1 (10.0%) mixed. Among the four (40.0%) patients with metastasis in the bone/BM compartment, three were HR because of primary site, and one because of concomitant lung metastasis. One patient had a negative initial screen of BM disease by qualitative detection of EWSR1 rearrangement and because no other risk factors were present it was assigned to the SR group. This patient suffered an isolated skull relapse 10 months after completing mP6, once adequate fresh tissue to determine the breakpoint was obtained. Retrospective analysis of the BM sample by qRT-PCR at diagnosis showed micrometastatic disease confirming the misclassification of this patient.
Outcome
After a median follow-up of 43.4 months (range: 18.1–72.8 months), the 3 and 5-year OS rate for the whole cohort was 55.0% (95% CI, 41–74%) and the EFS was 50.0% (95% CI, 36–68%), Figure 2A. Statistically significant differences were detected for risk groups, Figure 2B. The OS rate for SR patients was 76.0% (95% CI, 57–100%) at 3 and 5 years and for HR patients 36.0% (CI, 20–65%), P=0.0051. The 3 and 5-year EFS rate was 71.0% (CI, 54–94%) for SR and 29.0% (CI, 15–56%) for HR, P=0.0031. It is relevant to note that 3 and 5-year survival rates are the same because the curves stabilise at 33.8 months from study entry, the time when the last events occurred.
The analysis of age revealed significant differences in outcome, Figure 2C, with an optimum cut-off at 18 years. The 5-year OS rate for patients younger than 18 years of age is 74.0% (CI, 56–97%) and 31.0% for those 18 years and older (95% CI, 15–66%), P<0.001. The 5-year EFS rate was 65.0% (95% CI, 48–88%) for younger than 18 years and 31.0% (95% CI, 15–61%) for older than 18 years, P=0.0047.
We performed multivariate survival analyses, with age at study entry (<18 vs ⩾18) and risk group as variables. The first approach consisted of a Kaplan–Meier analysis considering the four groups obtained when combining the categorical variables age and risk group: HR and <18, HR and ⩾18, SR and <18, and SR and ⩾18. This analysis showed statistically significant differences in OS between the four groups, P<0.00001 (Figure 3A). Furthermore, pairwise comparisons showed statistically significant differences in OS between the HR and ⩾18 group and the remaining 3 groups. A second approach consisted in adjusting a Cox model for OS with the same variables (Figure 3B). Both age and risk group were statistically significant (P=0.0011 and P=0.0065, respectively), showing an association of both factors with the risk of death. According to these results we can conclude that (a) for each given risk group, the chances of dying because of disease for a patient aged 18 years or older is 6 times higher than that of a patient younger than 18 years; (b) for the same age group, the risk of dying for a HR patient is 4.8 times higher than that of a SR patient; (c) the risk of dying for a HR patient aged 18 years or older is 29 times higher than that of a patient younger than 18 years with SR disease; and (d) the risk of dying for a HR patient aged under 18 years is not significantly different than that of a SR patient aged 18 years or older.
To determine how the risk of dying changes with age, another Cox model using continuous age and risk group variables was performed. The hazard ratio corresponding to age was 1.1 (95% CI, 1.0–1.2), P<0.001. This finding points that for every year of age increase, the risk of dying increases 1.1 times. Therefore, for any two patients in the same risk group the risk of dying increases by 10.0% for each year of age difference at diagnosis.
The G/D regimen
Twenty out of 21 (95.2%) HR patients received two experimental window cycles of G/D. Response was assessed by BM MRD analysis and RECIST criteria. Overall, 12 out of 17 (70.6%) fully evaluable patients had an OR (7 PR and 5 SD) to the G/D window cycles. Of the 3 non-evaluable patients, one had surgery upfront and was not eligible for imaging evaluation (the patient is alive and in continued CR). The second patient had SD by RECIST but BM analysis was not performed adequately since the primary was in the pelvis and the sites sampled could not be adequately distinguished from the primary tumour. This patient continued on protocol and entered the maintenance phase in CR, however during maintenance an isolated lung relapse developed and currently is alive receiving third-line treatment. The third patient showed SD by RECIST criteria but BM analysis was not performed in time. This patient progressed through mP6 induction chemotherapy and died of disease progression 4 months from study entry.
Eleven of 21 (52.4%) HR patients received monthly G/D cycles. Five (45.5%) completed the 12 cycles uneventfully and four remain in durable complete remission with median follow-up of 56.3 months. Six patients did not complete maintenance therapy as planned: 2 because of toxicity and 4 because of disease progression. One (9.1%) patient developed treatment induced acute myeloblastic leukaemia (t-AML) after nine G/D cycles and died of progressive leukaemia 13 months later with no evidence of ES in autopsy. One patient developed grade-3 skin toxicity after the fourth G/D cycle in a previously irradiated area. The toxicity resolved without long-term sequels and the patient remains disease free, 64.1 months from study entry.
Out of four patients that progressed during G/D, two (50.0%) were not in CR at the end of mP6 evaluation, one showing PR and one SD. Two patients entered maintenance phase in CR and had a systemic progression after the sixth cycle. Overall, the disease progression rate for HR-ES patients during the G/D maintenance treatment after mP6 therapy is 36.4%.
The mP6 regimen
At the end of mP6 regimen, 32 out of 43 (74.4%) patients were fully evaluated for response. By RECIST criteria CR was achieved in 27 (75.0%); PR in 4 (11.1%); and SD in 2 (5.6%). Three (8.3%) patients progressed through the mP6 phase, two already showing progression after the G/D window cycles. BM analysis was performed in 30 patients at the end of mP6 and all (100.0%) were negative. Evaluation of response showed CR in 25/32 (78.1%), PR in 3/32 (9.4%), SD in 1/32 (3.1%) and PD in 3/32 (9.4%); an OR of 90.6%.
The three patients with PR in the primary site by RECIST showed no progression during follow-up. FDG PET-CT was performed in all showing no metabolic active disease. Four of five (80.0%) PD patients during the G/D window cycles showed OR after the mP6 regimen suggesting independent mechanisms of resistance.
Local control measures
Surgery was performed in 33 (76.7%) patients. Fourteen of 33 (42.4%) had positive surgical margins and 19 (57.6%) had non-affected margins, according to the protocol guidelines. All patients with affected margins had axial, chest wall or pelvic primary tumours. Four (9.3%) early local progressions occurred, all in axial sites, before local control measures were taken. Two (4.7%) patients relapsed locally after local control was performed.
Chemotherapy response was assessed by TN and was used to determine the need for RT. Twenty-six (78.8%) of the 33 tumour samples resected were assessable for response after 3 cycles of mP6 chemotherapy. Thirteen had more than 90% TN and 13 had <90%. TN did not correlate with outcome. Twenty-two (66.7%) of the 33 patients who underwent surgery received RT. One of the 9 (11.1%) patients treated with only surgery experienced local relapse and eventually died of disease progression.
Toxicity
Overall treatment with G/D was well tolerated. It was discontinued because of grade 3–4 toxicity in 2 (4.6%) patients. The main toxicity of the mP6 regimen was haematologic, as described (9–11). Two patients (4.6%) developed t-AML likely related to the mP6 alkylator and topoisomerase-II inhibitor components. Table 2 summarises all toxicities reported in the trial.
Discussion
GEIS-21, a multi-institutional study including children and adults, reproduced similar survival rates than original mP6 and P6 reports for patients with SR disease. Patients with HR disease showed significantly worse outcome although the results are slightly superior to the original MSKCC P6 report for patients with metastases (Kolb et al, 2003). This improvement affects mainly patients younger than 18 years and is likely related to the anti-tumour activity of the G/D regimen. Importantly, the OS and EFS curves stabilised at 33.8 months. A similar experience was described with MSKCC reports, although they were quite distinct from many ES trials whereby relapses have been reported as late as 15 years post treatment (Rodriguez-Galindo et al, 2006).
Patients with pelvic primaries are at a particularly high risk of an event according to many previous studies (Nesbit et al, 1990; Cotterill et al, 2000; Grier et al, 2003; Argon et al, 2004; Rodríguez-Galindo et al, 2007; Granowetter et al, 2009). Age has also been consistently identified as predicting higher event rates (Bacci et al, 2000; Cotterill et al, 2000; Jenkin et al, 2002), although the age cut-off has varied among studies. We were able to confirm the importance of age as an independent predictor of worse outcome, superior to the detection of metastasis in multivariate analysis. In the most recent report from the Children’s Oncology group (COG), trial of localised ES and the retrospective analysis of all COG trials indicate that age ⩾18 years is an important predictor of worse outcome (Womer et al, 2012; Marina et al, 2015). According to our results, and those of others, patients older than 18 years with metastasis or pelvic primaries should be prioritised to treatments using new agents since conventional cytotoxic drugs are unlikely to provide much benefit at a high toxicity cost.
In 2009, our group reported the use of G/D as an effective therapy to rescue relapsed paediatric ES patients (Mora et al, 2009). Other studies exploring G/D in various bone sarcomas for AYA (Navid et al, 2008; Fox et al, 2012; Rapkin et al, 2012) showed inferior anti-tumour activity. Of note, doses of G/D in those studies were 25–33% lower and the drugs often administered over shorter infusion times. Most recently, the G/D combination has been combined with bevacizumab, a regimen called ‘TAG’. To date 5 studies have been reported using TAG (Hingorani et al, 2012; Verschraegen et al, 2012; Dickson et al, 2015; Hensley et al, 2015; Kuo et al, 2017) showing activity in very HR AYA sarcomas. To the best of our knowledge, this is the first study to report the use of G/D in newly diagnosed ES patients. We show an objective response of 70.6% in keeping with most recent reports. In our experience, the G/D regimen was compatible with normal age-appropriate activities and outpatient treatment was possible because of the ease and rapidity of administration and the moderate side effects observed.
Metastatic status at diagnosis is the strongest prognostic factor for sarcomas. According to a French study, disseminated tumour cells in BM and blood were detected at diagnosis by RT-PCR in 20% of patients with localised ES (Schleiermacher et al, 2003). The prognostic value of molecularly detectable minimal residual disease however, remains controversial in the field mainly because of technical issues. In our study only 9.0% of cases showed BM infiltrate being 60.0% of the samples studied by qRT-PCR and 40.0% by conventional RT-PCR. In our study, all patients with BM metastasis at diagnosis presented HR features according to our risk definition. Hence, performing BM micrometastasis screening did not change the treatment arm. Our findings also suggest, as already reported in the literature (van der Woude et al, 1998), that current imaging techniques may not accurately evaluate response in ES.
In conclusion, we show that the G/D regimen provides clinical benefit to newly diagnosed HR-ES patients. The G/D schema provides a backbone regimen for managing minimal residual ES disease that is worth further exploring.
Change history
05 September 2017
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Argon A, Basaran M, Yaman F, Dizdar Y, Sakar B, Camlica H, Bavbek SE, Ozger H, Darendeliler E, Onat H (2004) Ewing’s sarcoma of the axial system in patients older than 15 years: dismal prognosis despite intensive multiagent chemotherapy and aggressive local treatment. Jpn J Clin Oncol 34 (11): 667–672.
Bacci G, Ferrari S, Bertoni F, Rimondini S, Longhi A, Bacchini P, Forni C, Manfrini M, Donati D, Picci P (2000) Prognostic factors in nonmetastatic Ewing’s sarcoma of bone treated with adjuvant chemotherapy: analysis of 359 patients at the Istituto Ortopedico Rizzoli. J Clin Oncol 18 (1): 4–11.
Contal C, O'Quigley J (1999) An application of changepoint methods in studying the effect of age on survival in breast cancer. Comput Stat Data Anal 30: 253–270.
Cotterill SJ, Ahrens S, Paulussen M, Jürgens HF, Voûte PA, Gadner H, Craft AW (2000) Prognostic factors in Ewing’s tumor of bone: analysis of 975 patients from the European Intergroup Cooperative Ewing’s Sarcoma Study Group. J Clin Oncol 18 (17): 3108–3114.
Cox DR (1972) Regression models and life-tables. J R Stat Soc B 34: 187–220.
Delattre O, Zucman J, Plougastel B, Desmaze C, Melot T, Peter M, Kovar H, Joubert I, de Jong P, Rouleau G, Aurias A, Thomas G (1992) Gene fusion with an ETS DNA-binding domain caused by chromosome translocation in human tumours. Nature 359 (6391): 162–165.
Dickson MA, D'Adamo DR, Keohan ML, D'Angelo SP, Carvajal RD, Gounder MM, Maki RG, Qin LX, Lefkowitz RA, McKennon OR, Hirst CM, Schwartz GK, Tap WD (2015) Phase II trial of gemcitabine and docetaxel with bevacizumab in soft tissue sarcoma. Sarcoma 2015: 1–7.
Fox E, Patel S, Wathen JK, Schuetze S, Chawla S, Harmon D, Reinke D, Chugh R, Benjamin RS, Helman LJ (2012) Phase II Study of sequential gemcitabine followed by docetaxel for recurrent Ewing sarcoma, osteosarcoma, or unresectable or locally recurrent chondrosarcoma: results of sarcoma alliance for research through collaboration study 003. Oncologist 17 (3): 321–329.
Granowetter L, Womer R, Devidas M, Krailo M, Wang C, Bernstein M, Marina N, Leavey P, Gebhardt M, Healey J, Shamberger RC, Goorin A, Miser J, Meyer J, Arndt CA, Sailer S, Marcus K, Perlman E, Dickman P, Grier HE (2009) Dose-intensified compared with standard chemotherapy for nonmetastatic Ewing sarcoma family of tumors: a children’s oncology group study. J Clin Oncol 27 (15): 2536–2541.
Greenwood M (1926) The natural duration of cancer. Rep Public Health Med Subj 33: 1–26.
Grier HE, Krailo MD, Tarbell NJ, Link MP, Fryer CJ, Pritchard DJ, Gebhardt MC, Dickman PS, Perlman EJ, Meyers PA, Donaldson SS, Moore S, Rausen AR, Vietti TJ, Miser JS (2003) Addition of ifosfamide and etoposide to standard chemotherapy for Ewing’s sarcoma and primitive neuroectodermal tumor of bone. N Engl J Med 348 (8): 694–701.
Hawkins DS, Bölling T, Dubois S, Hogendoorn PCW, Jurgens H, Paulussen M, Randall RL, Lessnick SL (2011) Ewing sarcoma. In Principles and practice of pediatric oncology PA Pizzo, DG Poplack, (eds) pp 987–1014. Lippincott-Raven: Philadelphia, PA, USA.
Hensley ML, Maki R, Venkatraman E, Geller G, Lovegren M, Aghajanian C, Sabbatini P, Tong W, Barakat R, Spriggs DR (2002) Gemcitabine and docetaxel in patients with unresectable leiomyosarcoma: results of a phase II trial. J Clin Oncol 20 (12): 2824–2831.
Hensley ML, Miller A, O'Malley DM, Mannel RS, Behbakht K, Bakkum-Gamez JN, Michael H (2015) Randomized phase III trial of gemcitabine plus docetaxel plus bevacizumab or placebo as first-line treatment for metastatic uterine leiomyosarcoma: an NRG Oncology/Gynecologic Oncology Group study. J Clin Oncol 33 (10): 1180–1185.
Hingorani P, Eshun F, White-Collins A, Watanabe M (2012) Gemcitabine, docetaxel, and bevacizumab in relapsed and refractory pediatric sarcomas. J Pediatr Hematol Oncol 34 (7): 524–527.
Holm S (1979) A simple sequentially rejective multiple test procedure. Scan J Stat 6: 65–70.
Jenkin RD, Al-Fawaz I, Al-Shabanah M, Allam A, Ayas M, Khafaga Y, Memon M, Rifai S, Schultz H, Younge D (2002) Localised Ewing sarcoma/PNET of bone—prognostic factors and international data comparison. Med Pediatr Oncol 39 (6): 586–593.
Kalbfleisch JD, Prentice RL (1980) The Statistical Analysis Of Failure Time Data. John Wiley and Sons: New York, NY, USA.
Kaplan EL, Meier P (1958) Non parametric estimation from incomplete observations. J Am Stat Assoc 53: 457–481.
Kolb EA, Kushner BH, Gorlick R, Laverdiere C, Healey JH, LaQuaglia MP, Huvos AG, Qin J, Vu HT, Wexler L, Wolden S, Meyers PA (2003) Long-term event-free survival after intensive chemotherapy for Ewing’s family of tumors in children and young adults. J Clin Oncol 21 (18): 3423–3430.
Kuo C, Kent PM, Logan AD, Tamulonis KB, Dalton KL, Batus M, Fernandez K, Mcfall RE (2017) Docetaxel, bevacizumab, and gemcitabine for very high risk sarcomas in adolescents and young adults: a single-center experience. Pediatr Blood Cancer e-pub ahead of print 5 November 2016;; doi:10.1002/pbc.26265.
Kushner BH, Meyers PA, Gerald WL, Healey JH, La Quaglia MP, Boland P, Wollner N, Casper ES, Aledo A, Heller G, Schwartz GK, Bonilla MA, Lindsley KL, Merchant TE, Rosenfield NS, Abramson SJ, Cheung NKV (1995) Very-high-dose short term chemotherapy for poor-risk peripheral primitive neuroectodermal tumors, including Ewing’s sarcoma, in children and young adults. J Clin Oncol 13 (11): 2796–2804.
Leu KM, Ostruszka LJ, Shewach D, Zalupski M, Sondak V, Biermann JS, Lee JS, Couwlier C, Palazzolo K, Baker LH (2004) Laboratory and clinical evidence of synergistic cytotoxicity of sequential treatment with gemcitabine followed by docetaxel in the treatment of sarcoma. J Clin Oncol 22 (9): 1706–1712.
Marina N, Granowetter L, Grier HE, Womer RB, Randall RL, Marcus KJ, McIlvaine E, Krailo M (2015) Age, tumor characteristics, and treatment regimen as event predictors in ewing: A Children’s Oncology Group Report. Sarcoma 2015: 927123.
Mora J, Cruz CO, Parareda A, de Torres C (2009) Treatment of pediatric relapsed/refractory pediatric sarcomas with gemcitabine and docetaxel. J Pediatr Hematol Oncol 31 (10): 723–729.
Mora J, de Torres C, Parareda A, Torner F, Galván P, Rodríguez E, Cardesa T, Salvador H, Suñol M, Huguet R, Cruz O (2011) Treatment of Ewing sarcoma family of tumors with a modified P6 protocol in children and adolescents. Pediatr Blood Cancer 57 (1): 69–75.
Navid F, Willert JR, McCarville MB, Furman W, Watkins A, Roberts W, Daw NC (2008) Combination of gemcitabine and docetaxel in the treatment of children and young adults with refractory bone sarcoma. Cancer 113 (2): 419–425.
Nesbit ME, Gehan EA, Burgert EO, Vietti TJ, Cangir A, Tefft M, Evans R, Thomas P, Askin FB, Kissane JM, Pritchard DJ, Herrmann J, Neff J, Makley JT, Gilula L (1990) Multimodal therapy for the management of primary, nonmetastatic Ewing’s Sarcoma of bone: a long-term follow-up of the first intergroup study. J Clin Oncol 8 (10): 1664–1674.
Peris-Bonet R, Salmerón D, Martínez-Beneito MA, Galceran J, Marcos-Gragera R, Felipe S, González V, Sánchez de Toledo Codina J (2010) Childhood cancer incidence and survival in Spain. Ann Oncol 21 (Suppl 3): S103–S110.
R Core Team (2016) R: A language and environment for statistical computing. R Foundation for Statistical Computing: Vienna, Austria http://www.R-project.org/.
Rapkin L, Qayed M, Brill P, Martin M, Clark D, George BA, Olson TA, Wasilewski-Masker K, Alazraki A, Katzenstein HM (2012) Gemcitabine and docetaxel (GEMDOX) for the treatment of relapsed and refractory pediatric sarcomas. Pediatr Blood Cancer 59 (5): 854–858.
Rodriguez-Galindo C, Navid F, Khoury J, Krasin M (2006) Ewing sarcoma family of tumors. In Pediatric Bone And Soft Tissue Sarcomas A Pappo, (ed). pp 181–211. Springer-Verlag: Berlin.
Rodríguez-Galindo C, Liu T, Krasin MJ, Wu J, Billups CA, Daw NC, Spunt SL, Rao BN, Santana VM, Navid F (2007) Analysis of prognostic factors in Ewing sarcoma family of tumors: review of St Jude Children’s Research Hospital studies. Cancer 110 (2): 375–384.
Schleiermacher G, Peter M, Oberlin O, Philip T, Rubie H, Mechinaud F, Sommelet-Olive D, Landman-Parker J, Bours D, Michon J, Delattre O (2003) Increased risk of systemic relapses associated with bone marrow micrometastasis and circulating tumor cells in localized Ewing tumor. J Clin Oncol 21 (1): 85–91.
Sorensen PH, Lessnick SL, Lopez-Terrada D, Liu XF, Triche TJ, Denny CT (1994) A second Ewing's sarcoma translocation, t(21;22), fuses the EWS gene to another ETS-family transcription factor, ERG. Nat Genet 6 (2): 146–151.
van der Woude HJ, Bloem JL, Hogendoorn PC (1998) Preoperative evaluation and monitoring chemotherapy in patients with high grade osteogenic and Ewing’s sarcoma: Review of current imaging modalities. Skeletal Radiol 27: 57–71.
Verschraegen CF, Arias-Pulido H, Lee SJ, Movva S, Cerilli LA, Eberhardt S, Schmit B, Quinn R, Muller CY, Rabinowitz I, Purdy M, Snyder D, Bocklage T (2012) Phase IB study of the combination of docetaxel, gemcitabine, and bevacizumab in patients with advanced or recurrent soft tissue sarcoma: the Axtell regimen. Ann Oncol 23 (3): 785–790.
Womer RB, West DC, Krailo MD, Dickman PS, Pawel BR, Grier HE, Marcus K, Sailer S, Healey JH, Dormans JP, Weiss AR (2012) Randomized controlled trial of interval-compressed chemotherapy for the treatment of localized Ewing sarcoma: a report from the Children’s Oncology Group. J Clin Oncol 30 (33): 4148–4154.
Acknowledgements
This work was supported by Fundación FERO (primera beca de Oncología traslacional esponsorizada por la Fundació Josep Botet); Instituto de Salud Carlos III, Ministerio de sanidad y consumo; Fondo de investigación sanitaria (TRA-130 2009 to JM); Asociación Pablo Ugarte; Ministry of Economy and Competitiveness of Spain-FEDER grants (PT13/0010/0047, PT13/0010/0056, RD12/0036/0017, PI14/01466 to JM). We gratefully acknowledge the editorial contribution of Callum Fletcher.
Author contributions
Conception and design by JM and CdT. Analysis and interpretation of data by JM, AC, SPJ, ALP, EM, CV, JMB, XGM, OC, JC, JMT, JMa, MAV, EdA and CdT. Writing the article by JM. Final approval of the manuscript and agreement to be accountable for all aspects of the work by all authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This study was presented in part at the oral sarcoma session of the American Society of Clinical Oncology Annual Meeting, Chicago, IL, 5 June 2016.
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Mora, J., Castañeda, A., Perez-Jaume, S. et al. GEIS-21: a multicentric phase II study of intensive chemotherapy including gemcitabine and docetaxel for the treatment of Ewing sarcoma of children and adults: a report from the Spanish sarcoma group (GEIS). Br J Cancer 117, 767–774 (2017). https://doi.org/10.1038/bjc.2017.252
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2017.252
Keywords
This article is cited by
-
Ewing Sarcoma Drug Therapy: Current Standard of Care and Emerging Agents
Pediatric Drugs (2023)
-
Irinotecan plus temozolomide in relapsed Ewing sarcoma: an integrated analysis of retrospective studies
BMC Cancer (2022)
-
Outcome of multidisciplinary treatment of peripheral primitive neuroectodermal tumor
Scientific Reports (2020)