Abstract
Background:
Existing literature examining analgesic medication use and epithelial ovarian cancer (EOC) risk has been inconsistent, with the majority of studies reporting an inverse association. Race-specific effects of this relationship have not been adequately addressed.
Methods:
Utilising data from the largest population-based case–control study of EOC in African Americans, the African American Cancer Epidemiology Study, the relationship between analgesic use (aspirin, non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs), and acetaminophen) and risk of EOC was estimated by multivariate logistic regression. The association of frequency, duration, and indication of analgesic use on EOC risk was also assessed.
Results:
Aspirin use, overall, was associated with a 44% lower EOC risk (OR=0.56; 95% CI=0.35–0.92) and a 26% lower EOC risk was observed for non-aspirin NSAID use (OR=0.74; 95% CI=0.52–1.05). The inverse association was strongest for women taking aspirin to prevent cardiovascular disease and women taking non-aspirin NSAIDs for arthritis. Significantly decreased EOC risks were observed for low-dose aspirin use, daily aspirin use, aspirin use for <5 years, and occasional non-aspirin NSAID use for a duration of ⩾5 years. No association was observed for acetaminophen use.
Conclusions:
Collectively, these findings support previous evidence that any NSAID use is inversely associated with EOC risk.
Similar content being viewed by others
Main
Inflammation may play a role in ovarian cancer carcinogenesis through the production of toxic oxidants and bioactive substances, increasing the chances of DNA damage and mutagenesis (Ness and Cottreau, 1999). Analgesic drugs, such as aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs), have anti-inflammatory properties and have been associated with reduced risks of several malignancies (Schreinemachers and Everson, 1994; García-Rodríguez and Huerta-Alvarez, 2001; Bosetti et al, 2012; Rothwell et al, 2012; Neill et al, 2013). Another commonly used type of analgesic medication, acetaminophen, has weak anti-inflammatory activity, but may reduce cancer risk through antigonadotropic effects (Cramer et al, 1998) that may be particularly relevant to ovarian cancer.
The existing literature examining analgesic drug use and ovarian cancer risk is inconsistent, with the majority of studies reporting mild protective associations (Rosenberg et al, 2000; Schildkraut et al, 2006; Wernli et al, 2008; Pinheiro et al, 2009) or no association (Moysich et al, 2001; Lacey et al, 2004; Murphy et al, 2012), with few suggesting weak positive relationships (Hannibal et al, 2008; Wu et al, 2009). A meta-analysis of 17 studies concluded that the existing body of evidence does not clearly support the presence of an association between analgesic use and ovarian cancer risk (Ni et al, 2013). However, a recent, well-powered pooled analysis using data from 12 case–control studies participating in the Ovarian Cancer Association Consortium observed a statistically significant decrease in epithelial ovarian cancer (EOC) risk for aspirin use, a decrease in risk for high-dose non-aspirin NSAID use, and no association for acetaminophen use (Trabert et al, 2014).
The majority of published literature examining the relationship between analgesic use and ovarian cancer was conducted in study populations composed predominately of white women, with little representation of African American (AA) women. There are several indications that a differing risk profile may be evident by race; published studies have suggested that AA women have higher inflammatory marker levels (e.g., interleukin-6, C-reactive protein) than white women (Albert et al, 2004; Khera et al, 2005; Paalani et al, 2011) and that there are differences in patterns of analgesic use by race (Zhou et al, 2014). To our knowledge, only one study (Setiawan et al, 2012) has evaluated race-specific associations for analgesic use and risk of EOC. Using the Multiethnic Cohort Study, Setiawan et al (2012) reported a weak inverse association, although not significant, between analgesic drug use and EOC risk for AA women. Although this is a large prospective study of ∼60 000 women, the inferences were limited by the small number of AA ovarian cancer cases (n=41). Other studies including AA women had relatively small samples of AA women with inadequate power to assess race-specific associations (Schildkraut et al, 2006; Wu et al, 2009). To overcome these challenges, the present analysis utilised the largest study of EOC in AA women, to date, to examine EOC risk associated with analgesic medication use exclusively among AA women.
Materials and methods
Study population
The African American Cancer Epidemiology Study (AACES) is a population-based case–control study examining risk factors for EOC exclusively among AA women. The AACES is a collaborative effort between 11 sites, including Alabama, Georgia, Illinois, Louisiana, Michigan, New Jersey, North Carolina, Ohio, South Carolina, Tennessee, and Texas. A detailed description of methods for AACES has been published elsewhere (Schildkraut et al, 2014). Briefly, cases were identified through rapid case ascertainment at SEER and state cancer registries, gynaecologic oncology departments, or hospitals. Eligibility criteria for the cases included: self-identification of AA race, aged 20–79 years, and newly diagnosed with invasive EOC after December 2010. The AA controls were identified through random digit dialing, and were frequency matched to cases by 5-year age category and state of residence. Women were excluded if previously diagnosed with EOC or if they had a bilateral oophorectomy. The AACES participants completed a telephone interview, including questions on demographic characteristics, reproductive history, oral contraceptive use, hormone therapy, family history of cancers, medication use, and a variety of lifestyle characteristics (e.g., smoking, physical activity). A short form of the questionnaire could also be completed in an effort to increase participation for women who would have otherwise refused. The study protocol was approved by the Institutional Review Board at each site, and informed consent was obtained for all participants.
As of August 2015, AACES has enrolled a total of 593 cases and 750 controls (N=1343). Of these, 71 women completed the short questionnaire, 52 cases and 19 controls. As the short form of the questionnaire did not inquire about analgesic medication use, the data set was restricted to include only those women completing the long form of the questionnaire (N=1272; 541 cases and 731 controls).
Analgesic drug use
In the questionnaire, participants were asked to recall any medications for pain or inflammation that were taken regularly, defined as at least once a week or at least 5 days out of the month, at any point in their lifetime. Examples of analgesic drugs and indications of use were provided to aid in recollection. Women who responded affirmatively to ever using pain or inflammation medications were then asked the name of the drug (including dosing information, if available), the reason for using the drug, how many days per month taken, age of first and last use, and the duration of use in months or years. This series of questions was repeated if the participant reported using more than one drug in her lifetime, with no participant reporting use of more than 10 analgesic drugs. The names of each drug were reviewed and categorised into the following groups: aspirin, non-aspirin NSAIDs, and acetaminophen. Some medications contained a combination of these analgesic types (e.g., aspirin and acetaminophen) and women who reported taking them were categorised as having used both types of analgesics. Any reported medication that did not fit into one of these categories (e.g., muscle relaxants, opioids, anti-epileptics) was considered as nonuse. To successfully model a time period of analgesic use that was not influenced by potential symptoms of an undiagnosed EOC, women who reported initiation of analgesic drug use within the year before the reference date (cases: diagnosis of EOC; controls: time of interview) were categorised as nonusers. In addition, a women who reported a duration of use of <6 months or any case who reported initiation of analgesic drug use after her EOC diagnosis was categorised as a nonuser.
Statistical analyses
Multivariate unconditional logistic regression was used to estimate odds ratios (ORs) and 95% confidence intervals (95% CIs) for the relationship between use of analgesic medications and risk of EOC. Each medication type was examined in a separate model with women who never used any analgesic medication serving as the referent group. In addition, the association of any type of NSAID (aspirin and non-aspirin NSAIDs, but not acetaminophen) with EOC risk was also examined. Use of aspirin, non-aspirin NSAIDs, and acetaminophen was further examined by frequency of use (<30 times per month, daily), duration of use (<5 years, ⩾5 years), combined frequency and duration of use (<30 times per month for <5 years, daily for <5 years, <30 times per month for ⩾5 years, daily for ⩾5 years), and indication of use (arthritis, menstrual cramps, injury/pain, headache, and heart disease). Because of insufficient data on dose for non-aspirin NSAIDs and acetaminophen, the effect of dose on EOC risk was assessed for aspirin only (low dose: <100 mg; high dose: ⩾100 mg).
The following a priori confounders were adjusted for in all models: age (age at diagnosis for cases and age at the time of interview for controls); study site (Alabama, Georgia and Tennessee combined (because of small sample sizes and geographic similarities), Illinois and Michigan combined (because of small sample sizes and geographic similarities), Louisiana, New Jersey, North Carolina, Ohio, South Carolina, and Texas); education (high school graduate or less, some post-high school training, and college or graduate degree); income (<$25 000, $25 000–$49 999, $50 000–$74 999, and ⩾$75 000); parity (nulliparous, 1, 2, 3, or more live births); family history of a first-degree relative with breast or ovarian cancer (yes, no); tubal ligation (yes, no); body mass index (<25 kg m−2: underweight and normal weight; 25–29.9 kg m−2: overweight; ⩾30 kg m−2: obese); oral contraceptive use (ever, never); menopausal status (pre-, peri-, and post-menopause); endometriosis (yes, no); pelvic inflammatory disease (yes, no); mild physical activity (yes, no); and moderate or strenuous physical activity (yes, no). Several comorbid conditions (e.g., heart disease, osteoporosis, and arthritis) were also evaluated as potential confounders, but no appreciable change in the effect estimates was observed and these conditions were not included in the final models. As women commonly reported use of more than one type of analgesic (e.g., of the women reporting acetaminophen use, 40% also reported using non-aspirin NSAIDs), use of (frequency of, duration of, indication of) the other analgesic types were simultaneously adjusted for in regression models. Therefore, the estimated associations in the present study reflect the independent effect of that type of analgesic without confounding by use of other analgesic types.
Finally, potential effect modification by two pro-inflammatory factors, BMI and smoking, was evaluated to determine whether analgesic medication use may be particularly beneficial for specific subgroups with higher inflammation. All analyses were conducted using SAS, Version 9.3 (SAS, Cary, NC, USA).
Results
A total of 1272 subjects, 541 cases and 731 controls, were included in the analysis. Table 1 describes demographic, reproductive, and lifestyle characteristics of cases and controls. Compared with controls, cases were more likely to be older (because of collapsing of 5-year age categories that were used for frequency matching), to have a high school education or less, to be nulliparous, to have a family history of a first-degree relative with breast or ovarian cancer, to have had endometriosis, and to have had pelvic inflammatory disease, and cases were less likely to have had tubal ligation, to use oral contraceptives, and to engage in mild intensity physical activity. The majority of cases were diagnosed with serous EOC (72.8%). Overall, 467 women reported use of any analgesic medication (36.7%). Of those, non-aspirin NSAIDs were the most commonly reported analgesic medication (62.7%), followed by aspirin and acetaminophen, 35.1% and 27.4% respectively (percentages do not equal 100% because of women taking more than one type of analgesic drug).
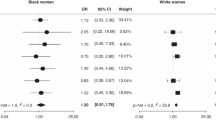
The associations between analgesic medication use and EOC risk are shown in Table 2. In comparison with never users of any analgesic medications, women who used any type of NSAIDs, including aspirin and non-aspirin NSAIDs but not acetaminophen, had a 27% lower risk of EOC (OR=0.73, 95% CI=0.54–0.98). No association with EOC risk was observed for women who used a combination of all analgesic drug types (OR=1.03, 95% CI=0.58–1.84). When evaluating use of each analgesic medication in separate models, a statistically significant 44% lower EOC risk was observed for women who reported use of aspirin (OR=0.56, 95% CI=0.35–0.92), and a 26% lower EOC risk (OR=0.74, 95% CI= 0.52–1.05) was observed for non-aspirin NSAID use. Acetaminophen was inversely associated with risk of EOC, although not statistically significant (OR=0.89, 95% CI=0.49–1.62).
Table 3 shows the associations for frequency and duration of use for each analgesic drug and risk of EOC. Irrespective of frequency and duration of aspirin use, inverse associations with risk of EOC were observed. Statistically significant lower risks of EOC were observed for daily aspirin use (OR=0.56, 95% CI=0.34–0.94) and aspirin use for a duration of <5 years (OR=0.52, 95% CI=0.28–0.98). A significant inverse association with risk of EOC was observed for AA women who occasionally used non-aspirin NSAIDs (<30 days per month), OR=0.54 (95% CI=0.35–0.83). An inverse association was observed for women who used non-aspirin NSAIDs for a duration of ⩾5 years, although not statistically significant (OR=0.71, 95% CI=0.47–1.07). In combined analyses of frequency and duration of use, inverse associations with EOC risk, although not statistically significant, were observed for all categories of aspirin use. However, a statistically significant lower risk of EOC was present among women who used non-aspirin NSAIDs for <30 days per month for a duration of ⩾5 years (OR=0.47, 95% CI=0.28–0.79). Although inversely associated, no statistically significant associations were observed for frequency or duration of acetaminophen use.
The most common indication of aspirin use was heart disease prevention (75.3%), whereas arthritis (45.5%) was the most common reason for non-aspirin NSAID use. Significant inverse associations were observed for the most prevalent indication of use for aspirin and non-aspirin NSAIDs, where a 50% lower EOC risk was observed for women using aspirin to prevent heart disease (OR=0.50, 95% CI=0.29–0.85) and a 48% lower EOC risk for women using non-aspirin NSAIDs for arthritis (OR=0.52, 95% CI=0.31–0.88) (data not shown).
The influence of dose for analgesic medications on EOC risk was also examined; however, sufficient data on dose were only present for aspirin use. Of the aspirin users with dosing information (n=127), 77.2% reported low-dose aspirin use. Low-dose aspirin users had a more pronounced, statistically significant inverse association with EOC risk, OR=0.54 (95% CI=0.31–0.97), in comparison with high-dose aspirin users, OR=0.78 (95% CI=0.30–2.06) (data not shown).
Presence of effect modification by BMI and smoking on the relationship between analgesic medications and EOC risk was not observed, P<0.05 (data not shown).
Discussion
This is the first study to examine the association between analgesic drug use and EOC risk in a large population of AA women. A statistically significant 44% lower EOC risk and a borderline significant 26% lower EOC risk was observed among aspirin and non-aspirin NSAID users, respectively. Although inversely related, no significant associations for acetaminophen use and EOC risk were observed in this population. The inverse association between analgesic use and EOC was consistent with previous findings from several studies (Schildkraut et al, 2006; Wernli et al, 2008; Pinheiro et al, 2009), and especially parallel the findings in the recent pooled analysis (Trabert et al, 2014). As with the pooled analysis, a similar inverse association for aspirin use and EOC risk, overall, was observed and especially for low-dose aspirin use, daily aspirin use, and shorter duration of aspirin use (<5 years). The present study also observed a decreased EOC risk for non-aspirin NSAID use overall and specifically for occasional monthly use (<30 days per month) for ⩾5 years. The previously published pooled analysis only observed a significant inverse association for high-dose non-aspirin NSAID use (Trabert et al, 2014); however, the non-aspirin NSAID use results of the present study were similar to many published studies (Fairfield et al, 2002; Schildkraut et al, 2006; Merritt et al, 2008; Wernli et al, 2008; Pinheiro et al, 2009).
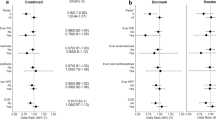
Interestingly, the inverse relationship between analgesic use and EOC risk observed in the present study was more pronounced than those observed in predominately white populations. In the only other study to conduct race-specific analyses for analgesic use and EOC risk, AA women had the strongest inverse association between aspirin and non-aspirin NSAID use and EOC risk, although not significant (Setiawan et al, 2012). Similar differences in the magnitude of effect by race have been reported for breast cancer, where use of analgesic medications was associated with a stronger inverse relationship for risk of breast cancer among AA women compared with all other races (Gill et al, 2007). As AA women have higher levels of inflammation, in general, compared with white women (Albert et al, 2004; Khera et al, 2005; Paalani et al, 2011), the potential benefit of taking anti-inflammatory drugs may be greater among AA women. The observed racial differences may also be because of a variety of factors that could vary by race, including genetic variants (e.g., prevalence of polymorphisms affecting cyclooxygenase activity), cultural attitudes toward analgesic use, or patterns of analgesic use. Further research needs to be conducted among racially diverse populations to confirm the observed racial differences in effect.
Although our findings suggest a protective effect for aspirin taken daily, at low doses, and for heart disease prevention, these three characteristics of use are highly correlated. A daily, low dose of aspirin is typically recommended for women at high risk of a cardiovascular event. In the WaTCH study, of the women who took aspirin for heart disease prevention, >85% also reported low-dose aspirin use and a daily frequency of use. As the overwhelming majority of women taking aspirin for heart disease are the same women using aspirin daily and at low doses, it is difficult to determine whether indication, frequency, dose, or a combination of these characteristics of use is contributing to the reduction in risk. In addition, the observed association between aspirin use for heart disease prevention and EOC risk in the present study may be explained by the effects of other cardiovascular drugs (e.g., β-blockers, statins, angiotensin-converting enzyme inhibitors) taken concurrently with analgesic medications. To explore this possibility, the cardiovascular medication use of women taking aspirin for heart disease prevention (n=122) was examined; although a slightly higher prevalence of these cardiovascular medications was taken by the controls, a statistically significant difference in drug use was not observed (data not shown).
Although ovarian cancer is associated with a long latency period, our findings suggest that shorter durations of aspirin use (<5 years) confer a stronger protective effect. Previous literature evaluating this relationship is inconsistent; some studies (Akhmedkhanov et al, 2001; Wernli et al, 2008), including the large pooled analysis (Trabert et al, 2014), observed a stronger inverse association for shorter durations of aspirin use, whereas other studies reported a stronger protection for longer durations of use (Rosenberg et al, 2000; Lacey et al, 2004; Schildkraut et al, 2006). Although unclear, we speculate that the findings for shorter durations of use could be because of a few factors. A recall bias may be present, resulting in misclassification of duration. Women may have had difficulty accurately recalling their duration of use if it occurred for a longer period of time. In addition, as analgesic medications are routinely used for a variety of indications, women may not keep track of each use, leading to an underestimation of duration. The majority of women reporting a short duration of aspirin use began taking these medications within 2–5 years of their diagnosis (cases) or the time of interview (controls). It is possible that using aspirin during this time period may be more beneficial in protecting against ovarian cancer progression. In fact, cyclooxygenase inhibitors (i.e., aspirin) have been shown to decrease cell growth, increase apoptosis, and block angiogenesis (Dubois et al, 1998). Experimental studies are needed to explore a mechanistic explanation as to why a shorter duration of aspirin use may provide a greater protection against ovarian cancer.
The present study has several strengths. First, data from the largest study of EOC among AA women were utilised, resulting in a relatively large sample size to examine race-specific associations for analgesic use. Another strength is the detailed exposure assessment of analgesic use, allowing for effect estimates by frequency, duration, and indication of use. Despite these strengths, there were several limitations present in this study. Data on analgesic drug use were ascertained through self-report and may be subject to potential biases. In particular, if participants used several different types of these medications during their lifetime, it may be difficult to accurately report their use of each, especially with regard to the duration, frequency, and indication of use. However, the associations observed in the present study are consistent with those from the large pooled analysis of the Ovarian Cancer Association Consortium (Trabert et al, 2014) and other cohort studies (Setiawan et al, 2012), although not significant. In addition, women with cardiovascular disease may be more acutely aware of their aspirin use; however, the prevalence of heart disease is similar among cases and controls (∼11%) and any resulting misclassification would bias the effect estimates towards the null. The lack of information on dose for non-aspirin NSAIDs and acetaminophen use was another limitation in this study. Because of the case–control study design, a potential selection bias may be present (i.e., women using analgesic medications may be more healthy and more likely to participate in the study). To evaluate the potential for a selection bias, the prevalence of analgesic use among AACES controls was compared with the available estimates for the general US population (Zhou et al, 2014). Although a direct comparison group for the demographic of the AACES study was unavailable, the prevalence of aspirin use among Black adults, aged ⩾18 years, was similar to AACES controls, and although possible, a selection bias is unlikely. Finally, although AACES is the largest study of EOC in AA, the sample of AA women within certain categories of exposure (e.g., indication of aspirin use, combined frequency, and duration of use) was small, limiting the power and precision of the effect estimates.
In conclusion, this study supports previous evidence that any NSAID use, but not acetaminophen, is inversely associated with EOC risk. The findings of the present study raise the intriguing possibility that the inverse association may be stronger in AA women compared with white women. This possibility emphasises the value of studying this question among racially diverse populations. Future research, specifically in large cohort studies, is needed in order to fully elucidate the impact of analgesic drug use on EOC risk in AA women, as well as other underrepresented racial groups.
Change history
29 March 2016
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Akhmedkhanov A, Toniolo P, Zeleniuch-Jacquotte A, Kato I, Koenig KL, Shore RE (2001) Aspirin and epithelial ovarian cancer. Prev Med 33: 682–687.
Albert MA, Glynn RJ, Buring J, Ridker PM (2004) C-Reactive protein levels among women of various ethnic groups living in the United States (from the Women’s Health Study). Am J Cardiol 93: 1238–1242.
Bosetti C, Rosato V, Gallus S, Cuzick J, La Vecchia C (2012) Aspirin and cancer risk: a quantitative review to 2011. Ann Oncol 23: 1403–1415.
Cramer DW, Harlow BL, Titus-Ernstoff L, Bohlke K, Welch WR, Greenberg ER (1998) Over-the-counter analgesics and risk of ovarian cancer. Lancet 351: 104–107.
Dubois RN, Abramson SB, Crofford L, Gupta RA, Simon LS, Van De Putte LB, Lipsky PE (1998) Cyclooxygenase in biology and disease. FASEB J 12: 1063–1073.
Fairfield KM, Hunter DJ, Fuchs CS, Colditz GA, Hankinson SE (2002) Aspirin, other NSAIDs, and ovarian cancer risk (United States). Cancer Causes Control 13: 535–542.
García-Rodríguez LA, Huerta-Alvarez C (2001) Reduced risk of colorectal cancer among long-term users of aspirin and nonaspirin nonsteroidal antiinflammatory drugs. Epidemiology 12: 88–93.
Gill JK, Maskarinec G, Wilkens LR, Pike MC, Henderson BE, Kolonel LN (2007) Nonsteroidal antiinflammatory drugs and breast cancer risk: the multiethnic cohort. Am J Epidemiol 166: 1150–1158.
Hannibal CG, Rossing MA, Wicklund KG, Cushing-Haugen KL (2008) Analgesic drug use and risk of epithelial ovarian cancer. Am J Epidemiol 167: 1430–1437.
Khera A, McGuire DK, Murphy SA, Stanek HG, Das SR, Vongpatanasin W, Wians FH, Grundy SM, de Lemos JA (2005) Race and gender differences in C-reactive protein levels. J Am Coll Cardiol 46: 464–469.
Lacey JV Jr, Sherman ME, Hartge P, Schatzkin A, Schairer C (2004) Medication use and risk of ovarian carcinoma: a prospective study. Int J Cancer 108: 281–286.
Merritt MA, Green AC, Nagle CM, Webb PM, Bowtell D, Chenevix-Trench G, Green A, Webb P, DeFazio A, Gertig D, Traficante N, Moore S, Hung J, Fereday S, Harrap K, Sadkowsky T, Mellon A, Robertson R, Vanden Bergh T, Maidens J, Nattress K, Chiew YE, Stenlake A, Sullivan H, Alexander B, Ashover P, Brown S, Corrish T, Green L, Jackman L, Martin K, Ranieri B, White J, Jayde V, Bowes L, Mamers P, Schmidt T, Shirley H, Viduka S, Tran H, Bilic S, Glavinas L, Proietto A, Braye S, Otton G, Bonaventura T, Stewart J, Friedlander M, Bell D, Baron-Hay S, Ferrier A, Gard G, Nevell D, Young B, Camaris C, Crouch R, Edwards L, Hacker N, Marsden D, Robertson G, Beale P, Beith J, Carter J, Dalrymple C, Hamilton A, Houghton R, Russell P, Brand A, Jaworski R, Harnett P, Wain G, Crandon A, Cummings M, Horwood K, Obermair A, Wyld D, Nicklin J, Perrin L, Ward B, Davy M, Hall C, Dodd T, Healy T, Pittman K, Henderson D, Hyde S, Miller J, Pierdes J, Blomfield P, Challis D, McIntosh R, Parker A, Brown B, Rome R, Allen D, Grant P, Hyde S, Laurie R, Robbie M, Healy D, Jobling T, Maniolitas T, McNealage J, Rogers P, Susil B, Veitch A, Constable J, Ping Tong S, Robinson I, Simpson I, Phillips K, Rischin D, Waring P, Loughrey M, O’Callaghan N, Murray B, Billson V, Galloway S, Pyman J, Quinn M, Hammond I, McCartney A, Leung Y, Haviv I, Zeps N, Green AC, Parsons PG, Hayward N, Webb P, Purdie D, Whiteman D (2008) Talcum powder, chronic pelvic inflammation and NSAIDs in relation to risk of epithelial ovarian cancer. Int J Cancer 122: 170–176.
Moysich KB, Mettlin C, Piver MS, Natarajan N, Menezes RJ, Swede H (2001) Regular use of analgesic drugs and ovarian cancer risk. Cancer Epidemiol Biomarkers Prev 10: 903–906.
Murphy MA, Trabert B, Yang HP, Park Y, Brinton LA, Hartge P, Sherman ME, Hollenbeck A, Wentzensen N (2012) Non-steroidal anti-inflammatory drug use and ovarian cancer risk: findings from the NIH-AARP Diet and Health Study and systematic review. Cancer Causes Control 23: 1839–1852.
Neill AS, Nagle CM, Protani MM, Obermair A, Spurdle AB, Webb PM (2013) Aspirin, nonsteroidal anti-inflammatory drugs, paracetamol and risk of endometrial cancer: a case-control study, systematic review and meta-analysis. Int J Cancer 132: 1146–1155.
Ness RB, Cottreau C (1999) Possible role of ovarian epithelial inflammation in ovarian cancer. J Natl Cancer Inst 91: 1459–1467.
Ni X, Ma J, Zhao Y, Wang Y, Wang S (2013) Meta-analysis on the association between non-steroidal anti-inflammatory drug use and ovarian cancer. Br J Clin Pharmacol 75: 26–35.
Paalani M, Lee JW, Haddad E, Tonstad S (2011) Determinants of inflammatory markers in bi-ethnic population. Ethn Dis 21: 142–149.
Pinheiro SP, Tworoger SS, Cramer DW, Rosner BA, Hankinson SE (2009) Use of nonsteroidal antiinflammatory agents and incidence of ovarian cancer in 2 large prospective cohorts. Am J Epidemiol 169: 1378–1387.
Rosenberg L, Palmer JR, Rao RS, Coogan PF, Strom BL, Zauber AG, Stolley PD, Shapiro S (2000) A case-control study of analgesic use and ovarian cancer. Cancer Epidemiol Biomarkers Prev 9: 933–937.
Rothwell PM, Price JF, Fowkes FGR, Zanchetti A, Roncaglioni MC, Tognoni G, Lee R, Belch JFF, Wilson M, Mehta Z, Meade TW (2012) Short-term effects of daily aspirin on cancer incidence, mortality, and non-vascular death: Analysis of the time course of risks and benefits in 51 randomised controlled trials. Lancet 379: 1602–1612.
Schildkraut JM, Alberg AJ, Bandera EV, Barnholtz-sloan J, Bondy M, Cote ML, Funkhouser E, Peters E, Schwartz AG, Terry P, Wallace K, Akushevich L, Wang F, Crankshaw S, Moorman PG (2014) A multi-center population-based case – control study of ovarian cancer in African-American women?: the African American Cancer Epidemiology Study (AACES). BMC Cancer 14: 688.
Schildkraut JM, Moorman PG, Halabi S, Calingaert B, Marks JR, Berchuck A (2006) Analgesic drug use and risk of ovarian cancer. Epidemiology 17: 104–107.
Schreinemachers D, Everson R (1994) Aspirin use and lung, colon, and breast cancer incidence in a prospective study. Epidemiology 5: 138–146.
Setiawan VW, Matsuno RK, Lurie G, Wilkens LR, Carney ME, Henderson BE, Kolonel LN, Goodman MT (2012) Use of nonsteroidal anti-inflammatory drugs and risk of ovarian and endometrial cancer: the Multiethnic Cohort. Cancer Epidemiol Biomarkers Prev 21: 1441–1449.
Trabert B, Ness RB, Lo-Ciganic W-H, Murphy MA, Goode EL, Poole EM, Brinton LA, Webb PM, Nagle CM, Jordan SJ, Risch HA, Rossing MA, Doherty JA, Goodman MT, Lurie G, Kjær SK, Hogdall E, Jensen A, Cramer DW, Terry KL, Vitonis A, Bandera EV, Olson S, King MG, Chandran U, Anton-Culver H, Ziogas A, Menon U, Gayther SA, Ramus SJ, Gentry-Maharaj A, Wu AH, Pearce CL, Pike MC, Berchuck A, Schildkraut JM, Wentzensen N (2014) Aspirin, nonaspirin nonsteroidal anti-inflammatory drug, and acetaminophen use and risk of invasive epithelial ovarian cancer: a pooled analysis in the Ovarian Cancer Association Consortium. J Natl Cancer Inst 106: djt431.
Wernli KJ, Newcomb PA, Hampton JM, Trentham-Dietz A, Egan KM (2008) Inverse association of NSAID use and ovarian cancer in relation to oral contraceptive use and parity. Br J Cancer 98: 1781–1783.
Wu AH, Pearce CL, Tseng C-C, Templeman C, Pike MC (2009) Markers of inflammation and risk of ovarian cancer in Los Angeles county. Int J Cancer 124: 1409–1415.
Zhou Y, Boudreau DM, Freedman AN (2014) Trends in the use of aspirin and nonsteroidal anti-inflammatory drugs in the general U.S. population. Pharmacoepidemiol Drug Saf 23: 43–50.
Acknowledgements
This study was supported by the National Cancer Institute (Grant CA142081). Additional support was provided by the Metropolitan Detroit Cancer Surveillance System with funding from the National Cancer Institute, National Institute of Health, the Department of Health and Human Services (Contract HHSN261201000028C), and the Epidemiology Research Core, supported in part by the National Cancer Institute Center (Grant P30 CA22453) to the Karmanos Cancer Institute, Wayne State University School of Medicine). We are grateful to the AACES interviewers, Christine Bard, LaTonda Briggs, Whitney Franz (North Carolina), and Robin Gold (Detroit). We also acknowledge the individuals responsible for facilitating case ascertainment across all AACES sites.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Peres, L., Camacho, F., Abbott, S. et al. Analgesic medication use and risk of epithelial ovarian cancer in African American women. Br J Cancer 114, 819–825 (2016). https://doi.org/10.1038/bjc.2016.39
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2016.39
Keywords
This article is cited by
-
Low-dose aspirin use and risk of ovarian cancer: a combined analysis from two nationwide studies in Denmark and Sweden
British Journal of Cancer (2024)
-
Ovarian Cancer in Women of African Ancestry (OCWAA) consortium: a resource of harmonized data from eight epidemiologic studies of African American and white women
Cancer Causes & Control (2019)
-
Associations between aspirin use and the risk of cancers: a meta-analysis of observational studies
BMC Cancer (2018)
-
Racial health disparities in ovarian cancer: not just black and white
Journal of Ovarian Research (2017)
-
Lifetime number of ovulatory cycles and epithelial ovarian cancer risk in African American women
Cancer Causes & Control (2017)