Abstract
Background:
There remains uncertainty on the need for bone staging in men with intermediate-risk prostate cancer. Current guidelines do not use mpMRI-staging information and rely on historic pathology grading.
Methods:
We investigated the ability of mpMRI and the new Grade Group system to better predict bone metastasis status in a retrospective cohort study of 438 men with prostate cancer undergoing baseline mpMRI and isotope bone scintigraphy (BS).
Results:
Including mpMRI-staging information significantly increased the specificity of bone metastasis detection from 3.0% to 24.2% (P<0.01) and sensitivity from 89.2% to 97.3%. The new Grade Group score demonstrated progressive increase in bone metastasis rates (P<0.001). A novel risk-stratification model combining Grade Groups, PSA and mpMRI staging shows promise in predicting bone metastasis and could potentially reduce BS usage by 22.4%–34.7%.
Conclusions:
Incorporating the new Grade Group system and mpMRI staging more accurately identified bone metastatic risk and suggests men with Grade Group ⩽2 and/or without radiological T3 disease could safely avoid routine bone staging.
Similar content being viewed by others
Main
Assessment of bone metastasis status is key for the management of prostate cancer (PCa) (NICE, 2014a; Fizazi et al, 2015). Clear evidence exists for staging investigations such as isotope bone scintigraphy (BS) in patients with high-risk PCa while precluding its routine use in low-risk disease (NICE, 2014a). However, the utility of BS in intermediate-risk disease is unclear with EAU, AUA and NICE offering conflicting guidance (Heidenreich et al, 2014; NICE, 2014a).
The International Society of Uro-Pathology (ISUP) have recently approved a new PCa ‘Grade Group’ classification system to improve correlation of Gleason grade to biochemical recurrence (Epstein et al, 2016). Concurrently, multiparametric (mp)-MRI has emerged as a crucial tool in local staging of PCa, allowing improved discrimination between T2 and T3 disease compared with clinical nomograms (Turkbey et al, 2013; Lawrence et al, 2014). However, current guidelines on bone staging do not mandate use of mpMRI information or Grade Groups (NICE, 2014a). Therefore, we investigated the ability of mpMRI-staging information or the new Grade Group system to help predict bone metastatic status and refine the use of bone staging investigations.
Materials and methods
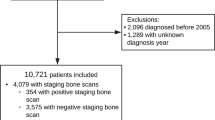
A radiology database was searched for all PCa patients undergoing baseline mpMRI prostate and BS from January 2010 to May 2015 in our tertiary centre (study registration CUH/3927). In cases of equivocal BS, the final status was recorded using a combination of clinical follow-up and/or any further radiological investigations. mpMRI was performed on a 3T Discovery MR750-HDx or 1.5T MR450 system (GE Healthcare, Waukesha, WI, USA) with a surface phased-array coil, including standard anatomical and functional diffusion-weighted imaging using multiple b-values, as previously described (Lawrence et al, 2014). All studies were reported by expert uro-radiologists and reviewed in a multi-disciplinary team (MDT) setting.
Gleason score was assessed according to the ISUP 2005 recommendations (Epstein et al, 2005) and recorded alongside the number of positive cores and percentage involvement of tissue. All cases were reported by a specialist uropathologist and reviewed a second time by another uro-patholigist prior to discussion at a specialist MDT. The core with the highest grade was used to devise the Grade Group.
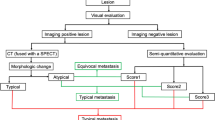
Patients were first categorised to low- (T1–T2a, Gleason ⩽6 and PSA<10 ng ml−1), intermediate- (T2b–c and/or Gleason=7 and/or PSA 10–20 ng ml−1) and high-risk (T3-T4, or Gleason 8–10 or PSA level >20 ng ml−1) according to NICE 2008 guidelines (NICE, 2014b). Patients were subsequently re-categorised according to the new Grade Group system (Epstein et al, 2016) and a novel five stratum Prognostic Risk Grouping system developed in our centre integrating PSA, Grade Group and mpMRI staging (Gnanapragasam et al, 2016; Table 1).
Contingency tables were constructed with expected frequency for bone metastasis and adjusted residuals calculated for each risk system (Supplementary Table S1). Pearson’s chi-squared test was used to examine the differences in observations. Comparison of sensitivities and specificities of bone metastasis between systems was made using McNemar’s test. To compare positive and negative predictive values, we used a generalised score statistic in R 3.1.2 (Leisenring et al, 2000; Stock and Hieschler, 2014). All other statistical analysis was performed in Stata14 (StataCorp LP, College Station, TX, USA).
Results
Four hundred and thirty-eight patients underwent mpMRI and BS. Mean age (±s.d.) was 67.1 years (±6.7) and mean PSA 21.3 ng ml−1 (±48.1). In this cohort, 37 patients had bone metastases (8.4%); Tables 2A and B. The specificity of BS was 86.5%. Fourteen out of 37 (37.8%) men with bone metastases also had evidence of pelvic metastasis on prostate MRI. Using NICE intermediate-risk as a threshold for performing BS, 426 BS would have been performed. Assessing this risk stratification as if it were a diagnostic test demonstrated a sensitivity of 100% but specificity of only 3.0%. Comparisons of other decision models were made against this standard (Table 3).
Adding mpMRI to current NICE risk groups
The distribution of patients by NICE classification is shown in Table 2A. By these categories, 33 out of 37 men with bone metastases were classified as high risk and 4 as intermediate risk. All 4 intermediate-risk patients had PSA<20.0 ng ml−1 but Gleason 4+3 disease. mpMRI staging re-categorised three of these patients to high risk (Supplementary Figures S1 and S2), improving the sensitivity of high risk for detecting bone metastases to 97.3% from 89.2% and specificity compared with intermediate risk to 24.2% from 3.0% (P<0.01). Using mpMRI-defined high-risk disease as a threshold for BS would have reduced the number of scintigrams performed by 98 (22.4%), with a single missed diagnosis.
Applying the new Grade Group scores to predict bone metastases
Using the new Grade Group scores in isolation, there was a progressive increase in bone metastases detection from 0 out of 43 (0%) for Grade Group 1 to 20 out of 121 (16.5%) for Grade Group 5 (Gleason 9–10); P<0.001, Table 2B. Using BS only for patients with Grade Group scores ⩾3 significantly improved sensitivity to 97.3% and significantly improved specificity to 37.7% (P<0.01); Table 3. Using this cutoff would have reduced the number of BS by 152 (34.7%), with a single missed diagnosis.
Combining mpMRI and Grade Group scores in a novel risk-stratification system
This model defines five prognostic risk strata for prostate cancer (Table 1; Gnanapragasam et al, 2016). Within this model, no men in Risk Groups 1 or 2 had bone metastasis. Bone metastasis rate increased progressively in Risk Groups 3 (2.13%), 4 (5.8%) and 5 (13.7%); P=0.004. Using Risk Group 4 as a threshold for bone staging demonstrated improvement in specificity to 23.9% (P<0.01) and 97.3% sensitivity, with a 22.1% reduction in the need for BS.
Discussion
Detection of bone metastasis confers a significantly worse prognosis in men with PCa and is thus an important part of the staging work-up (Fizazi et al, 2015). In our study, we showed that only 8.4% of men had bone metastasis out of the 438 men scanned, emphasising the need to refine use of this resource-intensive investigation. Of note, we did not find that a high PSA alone was a good discriminator; in our cohort, we identified 4 men with bone metastases and a PSA<20 ng ml−1, which is at odds with other reports (McArthur et al, 2012).
In this study, we have demonstrated evidence that mpMRI staging provides a useful adjunct in appropriately identifying men who will benefit most from BS. The integration of mpMRI alongside traditional biochemical and pathological markers, to re-categorise patients as high-risk disease, would have led to a 99.0% NPV for bone metastases at this threshold, alongside a significant increase in specificity to 24.2% and reduction in BS use. We also provide early validation of the new histological Grade Group system, with BS yield being higher in Grade Group 3 (bone metastasis rate of 5.8%) compared with Grade Group 2 (0.6%). Setting a threshold for BS of Grade Group ⩾3 would have reduced the number of BS performed by 152 (34.7%), with a single false negative. This correlates with data used to inform the 2015 update to EAU guidelines (Heidenreich et al, 2014) and should encourage adoption of these proposed grading groups (Epstein et al, 2016).
It should be noted that grade and stage data are not used in isolation in clinical management. We therefore tested the proof-of-principle of a new prognostic risk model incorporating the new Grade Group system, mpMRI and biochemical information. This refinement demonstrated promising results with an NPV of 100% for Risk Groups 1 and 2. Taken together, our data demonstrate that the combined use of more accurate mpMRI staging and histological grade stratification better defines men who benefit most from bone staging investigations. These promising results show potential for reductions in the use of BS by up to a third while maintaining sensitivity and NPV above 97% and 99%, respectively.
The main limitation of our study is its retrospective nature and a selected population only including men undergoing both mpMRI and BS. The relatively small absolute numbers of men with intermediate-risk disease or men with bone metastases in this cohort should lead to caution when interpreting sensitivity or specificity values in isolation. Additionally, bone scintigraphy can be questioned as an ideal standard for diagnosing bone metastases; however, our data reflects current clinical practice and should be useful in guiding clinical management. PET-CT using fluorine or choline tracers has been shown to be a superior, albeit more expensive option for assessing metastatic bone involvement (Fuccio et al, 2012). Our results would require further validation in external cohorts in a prospective study and preferably using these modalities.
Conclusion
We demonstrate for the first time that the new histological Grade Group system and mpMRI staging more accurately identified men at risk of harbouring bone metastases. Importantly, our data strongly suggest that men without histology in Grade Group ⩾3 and/or radiological T3 disease could safely avoid routine bone staging.
Change history
22 November 2016
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Epstein JI, Zelefsky MJ, Sjoberg DD, Nelson JB, Egevad L, Magi-Galluzzi C, Vickers AJ, Parwani AV, Reuter VE, Fine SW, Eastham JA, Wiklund P, Han M, Reddy CA, Ciezki JP, Nyberg T, Klein EA (2016) A contemporary prostate cancer grading system: a validated alternative to the gleason score. Eur Urol 69 (3): 428–435.
Epstein JI, Allsbrook WC, Amin MB, Egevad LI Committee IG (2005) The 2005 International Society of Urological Pathology (ISUP) consensus conference on gleason grading of prostatic carcinoma. Am J Surg Pathol 29: 1228–1242.
Fizazi K, Massard C, Smith M, Rader M, Brown J, Milecki P, Shore N, Oudard S, Karsh L, Carducci M, Damião R, Wang H, Ying W, Goessl C (2015) Bone-related parameters are the main prognostic factors for overall survival in men with bone metastases from castration-resistant prostate cancer. Eur Urol 68 (1): 42–50.
Fuccio C, Castellucci P, Schiavina R, Guidalotti PL, Gavaruzzi G, Montini GC, Nanni C, Marzola MC, Rubello D, Fanti S (2012) Role of 11C-choline PET/CT in the re-staging of prostate cancer patients with biochemical relapse and negative results at bone scintigraphy. Eur J Radiol 81 (8): e893–e896.
Gnanapragasam VJ, Lophatananon A, Wright KA, Muir KR, Gavin A, Greenberg DC (2016) Improving clinical risk stratification at diagnosis in primary prostate cancer: a prognostic modelling study. PLoS Med 13 (8): e1002063.
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, Mason M, Matveev V, Wiegel T, Zattoni F, Mottet N European Association of Urology (2014) EAU guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol 65 (1): 124–137.
Lawrence EM, Gallagher FA, Barrett T, Warren AY, Priest AN, Goldman DA, Goldman D, Sala E, Gnanapragasam VJ (2014) Preoperative 3-T diffusion-weighted MRI for the qualitative and quantitative assessment of extracapsular extension in patients with intermediate- or high-risk prostate cancer. AJR Am J Roentgenol 203 (3): W280–W286.
Lawrence EM, Tang SY, Barrett T, Koo B, Goldman DA, Warren AY, Axell RG, Doble A, Gallagher FA, Gnanapragasam VJ, Kastner C, Sala E (2014) Prostate cancer: performance characteristics of combined T-W and DW-MRI scoring in the setting of template transperineal re-biopsy using MR-TRUS fusion. Eur Radiol 24 (7): 1497–1505.
Leisenring W, Alonzo T, Pepe MS (2000) Comparisons of predictive values of binary medical diagnostic tests for paired designs. Biometrics 56 (2): 345–351.
McArthur C, McLaughlin G, Meddings RN (2012) Changing the referral criteria for bone scan in newly diagnosed prostate cancer patients. Br J Radiol 85 (1012): 390–394.
NICE National Institute for Health and Care Excellence (2014a) NICE Guidelines [CG175] Prostate cancer: diagnosis and treatment. Available at: https://www.nice.org.uk/guidance/cg175.
NICE National Institute for Health and Care Excellence (2014b) Prostate cancer: diagnosis and treatment. Update of clinical guideline 58. Appendices J-L., p 31. Available at: https://www.nice.org.uk/guidance/cg175/evidence/appendices-jl-191710766.
Stock C, Hieschler T (2014) DTComPair: comparison of binary diagnostic tests for paired designs. R Package. Version 1.0.3.
Turkbey B, Mani H, Aras O, Ho J, Hoang A, Rastinehad AR, Agarwal H, Shah V, Bernardo M, Pang Y, Daar D, McKinney YL, Linehan WM, Kaushal A, Merino MJ, Wood BJ, Pinto PA, Choyke PL (2013) Prostate cancer: can multiparametric MR imaging help identify patients who are candidates for active surveillance? Radiology 268 (1): 144–152.
Acknowledgements
We thank research support from the National Institute of Health Research, Cambridge Biomedical Research Centre, Cancer Research UK, Cancer Research UK and the Engineering and Physical Sciences Research Council Imaging Centre in Cambridge and Manchester and the Cambridge Experimental Cancer Medicine Centre.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Thurtle, D., Hsu, R., Chetan, M. et al. Incorporating multiparametric MRI staging and the new histological Grade Group system improves risk-stratified detection of bone metastasis in prostate cancer. Br J Cancer 115, 1285–1288 (2016). https://doi.org/10.1038/bjc.2016.353
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2016.353
Keywords
This article is cited by
-
Evaluation of selective bone scan staging in prostate cancer – external validation of current strategies and decision-curve analysis
Prostate Cancer and Prostatic Diseases (2022)
-
The Cambridge Prognostic Groups for improved prediction of disease mortality at diagnosis in primary non-metastatic prostate cancer: a validation study
BMC Medicine (2018)
-
Prostate cancer grading: a decade after the 2005 modified system
Modern Pathology (2018)
-
Novel three-dimensional bone ‘mapping’ software can help assess progression of osseous metastases from routine CT
Radiation Oncology (2017)