Abstract
Background:
Diabetes is a risk factor for pancreatic cancer but its association with survival from pancreatic cancer is poorly understood. Our objective was to investigate the association of diabetes with survival among pancreatic cancer patients in a prospective cohort-based study where diabetes history was ascertained before pancreatic cancer diagnosis.
Methods:
We evaluated survival by baseline (1993–2001) self-reported diabetes history (n=62) among 504 participants that developed exocrine pancreatic cancer within the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial. Hazard ratios (HRs) and 95% confidence intervals (CIs) for mortality were estimated using Cox proportional hazards model, adjusted for age, sex, body mass index, race, smoking, and tumour stage (local, locally advanced, and metastatic).
Results:
The multivariable-adjusted HR for mortality comparing participants with diabetes to those without was 1.52 (95% CI=1.14–2.04, P-value <0.01). After excluding those diagnosed with pancreatic cancer within 3 years of study enrolment, HR for mortality among those with diabetes was 1.45 (95% CI=1.06–2.00, P-value=0.02).
Conclusions:
Using prospectively collected data, our findings indicate that diabetes is associated with worse survival among patients with pancreatic cancer.
Similar content being viewed by others
Main
Pancreatic cancer is currently the fourth leading cause of cancer death but is projected to be the second leading cause before 2020 (Pancreatic Cancer Action Network, 2012). In 2013, 45 220 Americans will be diagnosed with pancreatic cancer and 85% (38 460) of them will die from the disease (Siegel et al, 2013). Thus, identifying factors that impact pancreatic cancer survival is of utmost priority.
The association of diabetes before pancreatic cancer diagnosis and survival among pancreatic cancer patients is poorly understood, probably, because few studies have investigated this association and most have been clinic-based studies that used retrospectively collected data or limited their analyses to pancreatic cancer patients who underwent surgical resection (McWilliams et al, 2010; Olson et al, 2010; Dandona et al, 2011; Hwang et al, 2013), although diabetes has been associated with an increased overall mortality (Seshasai et al, 2011). Another challenge is establishing the temporality of association between diabetes and pancreatic cancer in relation to survival because of the bidirectional relationship between diabetes and pancreatic cancer. To have a better understanding of whether diabetes impacts pancreatic cancer survival, the association of diabetes with pancreatic cancer survival should be evaluated in cohort studies where diabetes history is prospectively collected before pancreatic cancer diagnosis but these studies are lacking.
We investigated the association of diabetes with survival among pancreatic cancer patients in the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial, where history of diabetes was ascertained before pancreatic cancer diagnosis. This knowledge could be useful in the clinical management and risk stratification among pancreatic cancer patients. In addition, it could provide an insight into possible mechanistic pathways that might impact survival among patients with pancreatic cancer.
Materials and Methods
Design overview, study subjects, and endpoints
The PLCO Cancer Screening Trial is a randomized, two-armed, controlled trial designed to determine the effects of screening on disease-specific mortality for cancers of the prostate, lung, colorectal, and ovaries. The PLCO study design and characteristics of the participants have been described in detail elsewhere (Zhu et al, 2013). Briefly, the PLCO enroled 154 901 men and women aged 55–74 years from 10 centres in the United States between November 1993 and July 2001 (Zhu et al, 2013). Study participants filled a baseline questionnaire at study entry where they provided demographic, personal, and medical information, including history of diabetes.
Each eligible participant provided written informed consent. Pancreatic cancer diagnoses were determined from yearly questionnaires completed by participants or next of kin as well as state registries, death certificates, and physician reports and confirmed by PLCO staff (Oaks et al, 2010). At the time of last follow-up in December 2010, 627 primary newly diagnosed exocrine pancreas cancer cases had been identified. Pancreatic cancer stage was abstracted at the PLCO centres in categories of localised, locally advanced, and metastatic in 2010 from previously collected pathology reports and medical records used for cancer confirmation. As stage is an important prognostic factor, we decided a priori to include only those with information on tumour stage in our analyses. Tumour stage was classified as (i) local disease amenable to surgical resection; (ii) locally advanced disease with extra-pancreatic extension not amenable to surgical resection, but without distant metastases; and (iii) distant metastatic disease. The American Joint Committee on Cancer (AJCC)/International Union for Cancer Control (IUCC) tumour-lymph nodes-metastasis (TNM) staging was converted to the above categories. The AJCC/IUCC stages I and II corresponds to local disease, stage III corresponds to locally advanced disease, and stage IV corresponds to metastatic disease. We excluded participants with missing information on tumour stage (N=95) and diabetes (N=28). Therefore, our final analytic cohort for this study consisted of 504 exocrine pancreas cancer cases (437 were pancreatic ductal adenocarcinomas, PDAC). Baseline characteristics were similar for those who had information on tumour stage and those who did not. For instance, 14% of those with no information on stage had a positive history of diabetes compared with 12% of those with information on stage (P-value=0.30).
Information on deaths and causes of death were obtained by linking the study population to the National Death Index (Miller et al, 2000). The institutional review boards of the National Cancer Institute and each of the centres that participated approved the study.
Statistical analysis
We compared baseline characteristics of participants who developed pancreatic cancer by diabetes history using χ2-test for categorical variables and Wilcoxon Rank test for continuous variables. Survival was calculated from the day of pancreatic cancer diagnosis to the day of death or December 2010, whichever came first. We used Cox proportional hazards model to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs) of pancreatic cancer mortality by diabetes status. We first adjusted the model for age and tumour stage. In multivariable adjusted model, we adjusted for age, sex, body mass index (BMI), smoking status, race, and tumour stage. We conducted analyses stratified by sex and stage. Sex and stage were excluded from multivariable models stratified on these variables. Furthermore, because pancreatic cancer-induced diabetes could start 2 years before a diagnosis of pancreatic cancer is made, we conducted sensitivity analysis excluding participants who developed pancreatic cancer within 3 years of enrolment.
Survival curves were generated using Kaplan–Meier method. The proportional hazard assumption was tested and satisfied through the use of time-dependent covariate method. Statistical analyses were performed using SAS 9.3 statistical package (SAS Institute, Cary, NC, USA). Statistical significance was set at P<0.05 and all P-values are two-sided.
Results
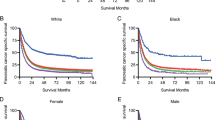
Median age at baseline examination was 64 years. Baseline characteristics, by diabetes history, are listed in Table 1. Of the 504 participants with incident exocrine pancreatic cancer, 62 (12%) reported a history of diabetes before pancreatic cancer diagnosis. Participants with diabetes were comparable with those without diabetes for most characteristics except BMI. At the end of the follow-up period, 91% of the participants (N=460) had died. Median survival was shorter for those with diabetes (92 days) than for those without diabetes (139 days, P-value 0.05). Death fractions for diabetic/non-diabetic patients were 92% vs 91%. Most of the deaths among people with diabetes occurred during the first 500 days of follow-up (Figure 1).
The majority (93%) of participants had pancreatic cancer listed as the cause of death on their death certificates (95% among those with diabetes and 93% among those without diabetes). Some other causes of death listed include ischaemic heart disease (four among those without diabetes and one among those with diabetes), cerebrovascular disease (four among those without diabetes and one among those with diabetes).
A history of diabetes was associated with reduced survival (Figure 1). In multivariable adjusted Cox regression model, the HR for mortality comparing those with diabetes to those without diabetes was 1.52 (95% CI=1.14–2.04, P-value<0.01) (Table 2). In analyses stratified by tumour stage, diabetes was associated with a 2.3-fold (95%CI=1.16–4.58) and 1.5-fold (95% CI=1.04–2.24) greater mortality among those with localised and metastatic diseases, respectively, but not among those with locally advanced disease (HR=1.17, 95% CI=0.62–2.20). In sensitivity analysis excluding participants who developed pancreatic cancer within 3 years of enrolment, diabetes was associated with increased hazard of mortality (HR=1.45, 95% CI=1.06–2.00, P-value=0.02).
The results were identical in analysis limited to participants with PDAC (n=437) (Supplementary Table 1).
Discussion
In this prospective cohort-based study, we observed that participants who reported having diabetes before being diagnosed with pancreatic cancer had worse survival compared with those who did not have diabetes.
Previous studies have evaluated the associations of diabetes with survival among pancreatic cancer patients using retrospectively collected data and among patients who underwent surgical resection, with conflicting results (Chu et al, 2010; McWilliams et al, 2010; Olson et al, 2010; Dandona et al, 2011; Hwang et al, 2013). In a large study conducted within the United Kingdom, there was no survival difference between those with diabetes and those without (Hwang et al, 2013). However, the authors reported increased pancreatic cancer mortality among those who had long-term diabetes (>5 years). Diabetes was not associated with survival from pancreatic cancer in three clinical studies (McWilliams et al, 2010; Olson et al, 2010; Dandona et al, 2011). Our study underscores the need for prospective studies to evaluate the associations of diabetes with survival among pancreatic cancer patients. In the Cancer Prevention Study II (CPS II), a history of diabetes was associated with higher death rates (Calle et al, 1998) but the analyses did not take into account tumour stage.
Experimental studies suggest that diabetes can impact pancreatic cancer survival through its effect on glucose metabolism and insulin resistance-related metabolic markers. There is emerging evidence that diabetes alters, and reprograms the intracellular metabolic environment to a metabolism more favourable to proliferation (Regel et al, 2012; Sah et al, 2013). Kras, p53, and c-Myc pathways impact pancreatic cancer proliferation and studies have shown that these pathways also affect energy metabolism by influencing glucose and glutamine utilisation (Regel et al, 2012). In addition, hyperinsulinaemia enhances pancreatic cell proliferation and invasiveness either directly or indirectly through its effects on insulin-like growth factor (IGF) pathway. Metformin, an anti-diabetic drug, has been shown to improve survival among pancreatic cancer patients (Sadeghi et al, 2012), possibly via its impact on insulin/IGF-I signalling (Rozengurt et al, 2010). Median overall survival was 15.2 months among pancreatic cancer patients treated with metformin compared with 11.1 months among the non-metformin group (Sadeghi et al, 2012). A better understanding of the biological mechanisms driving the association between diabetes and pancreatic cancer survival could provide insights into the development of targeted therapies for some pancreatic cancer patients.
Another possible explanation for the worse survival may be because diabetics have more comorbidities, especially cardiovascular comorbidities, than those without diabetes. These comorbidities might put those with diabetes at a survival disadvantage directly or indirectly as physicians may be less likely to use aggressive chemotherapy on patients with diabetes because of the comorbidities. Hence, diabetes status may be driving aggressiveness of treatment decisions. Nevertheless, in our study cohort, pancreatic cancer was reported as the cause of death in 95% of participants with diabetes and 93% of participants without diabetes and there appears to be no difference in death due to ischaemic heart disease and cerebrovascular accident between the two groups. Further, we had no information available on the history of chronic pancreatitis. The worse survival among those with diabetes could also be related to later stage at diagnosis, although information on tumour staging in our data does not support this.
The major strength of our study is its prospective nature. Information on diabetes was collected before pancreatic cancer diagnosis. In addition, we adjusted for stage, which is an important determinant of pancreatic cancer survival. Our study has the following limitations. A sizeable proportion of diabetes may be undiagnosed. Using haemoglobin A1C concentrations as a diagnostic test, up to 19% of people with diabetes in the United States are undiagnosed (Cowie et al, 2010). Because history of diabetes was based on self-report, prevalence of diabetes in our study population would have been underestimated; hence some participants with diabetes would have been misclassified as not having diabetes. Any misclassification, though, would have been non-differential. Finally, because PLCO is a multicenter study, patients diagnosed with pancreatic cancer were treated at different hospitals in different geographical locations; hence, treatment programs which were likely to vary among patients could have contributed to differences in survival but we had no information on the treatment programs, particularly surgery, received by the patients.
In conclusion, this survival analysis using incident cases ascertained from the PLCO prospective cohort, a history of diabetes before pancreatic cancer diagnosis was associated with higher mortality among pancreatic cancer patients. Studies characterising the molecular mechanisms driving this association are needed as these can provide insights into relevant pathways that could be targeted for possible therapeutic interventions.
Change history
01 July 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Calle EE, Murphy TK, Rodriguez C, Thun MJ, Heath CW Jr (1998) Diabetes mellitus and pancreatic cancer mortality in a prospective cohort of United States adults. Cancer Causes Control 9 (4): 403–410.
Chu CK, Mazo AE, Goodman M, Egnatashvili V, Sarmiento JM, Staley CA, Galloway JR, Adsay NV, Jacobs S, Kooby DA (2010) Preoperative diabetes mellitus and long-term survival after resection of pancreatic adenocarcinoma. Ann Surg Oncol 17 (2): 502–513.
Cowie C, Rust K, Byrd-Holt D, Gregg E, Ford E, Geiss L, Bainbridge K, Fradkin J (2010) Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988-2006. Diabetes Care 33 (3): 562–568.
Dandona M, Linehan D, Hawkins W, Strasberg S, Gao F, Wang-Gillam A (2011) Influence of obesity and other risk factors on survival outcomes in patients undergoing pancreaticoduodenectomy for pancreatic cancer. Pancreas 40 (6): 931–937.
Hwang A, Narayan V, Yang YX (2013) Type 2 diabetes mellitus and survival in pancreatic adenocarcinoma: a retrospective cohort study. Cancer 119 (2): 404–410.
McWilliams RR, Matsumoto ME, Burch PA, Kim GP, Halfdanarson TR, de Andrade M, Reid-Lombardo K, Bamlet WR (2010) Obesity adversely affects survival in pancreatic cancer patients. Cancer 116 (21): 5054–5062.
Miller AB, Yurgalevitch S, Weissfeld JL Prostate LC, Ovarian Cancer Screening Trial Project T (2000) Death review process in the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial. Control Clin Trials 21 (6 Suppl): 400S–406S.
Oaks BM, Dodd KW, Meinhold CL, Jiao L, Church TR, Stolzenberg-Solomon RZ (2010) Folate intake, post-folic acid grain fortification, and pancreatic cancer risk in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. Am J Clin Nutr 91 (2): 449–455.
Olson SH, Chou JF, Ludwig E, O'Reilly E, Allen PJ, Jarnagin WR, Bayuga S, Simon J, Gonen M, Reisacher WR, Kurtz RC (2010) Allergies, obesity, other risk factors and survival from pancreatic cancer. Int J Cancer 127 (10): 2412–2419.
Pancreatic Cancer Action Network (2012) The alarming rise of pancreatic cancer deaths in the United States: why we need to stem the tide.
Regel I, Kong B, Raulefs S, Erkan M, Michalski CW, Hartel M, Kleeff J (2012) Energy metabolism and proliferation in pancreatic carcinogenesis. Langenbecks Arch Surg 397 (4): 507–512.
Rozengurt E, Sinnett-Smith J, Kisfalvi K (2010) Crosstalk between insulin/insulin-like growth factor-1 receptors and G protein-coupled receptor signaling systems: a novel target for the antidiabetic drug metformin in pancreatic cancer. Clin Cancer Res 16 (9): 2505–2511.
Sadeghi N, Abbruzzese JL, Yeung SC, Hassan M, Li D (2012) Metformin use is associated with better survival of diabetic patients with pancreatic cancer. Clin Cancer Res 18 (10): 2905–2912.
Sah RP, Nagpal SJ, Mukhopadhyay D, Chari ST (2013) New insights into pancreatic cancer-induced paraneoplastic diabetes. Nat Rev Gastroenterol Hepatol 10 (7): 423–433.
Seshasai SR, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, Sarwar N, Whincup PH, Mukamal KJ, Gillum RF, Holme I, Njolstad I, Fletcher A, Nilsson P, Lewington S, Collins R, Gudnason V, Thompson SG, Sattar N, Selvin E, Hu FB, Danesh J (2011) Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 364 (9): 829–841.
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA: Cancer J Clin 63 (1): 11–30.
Zhu CS, Pinsky PF, Kramer BS, Prorok PC, Purdue MP, Berg CD, Gohagan JK (2013) The Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial and Its Associated Research Resource. J Natl Cancer Inst 105 (22): 1684–1693.
Acknowledgements
Adetunji T Toriola is supported by the Washington University School of Medicine, Barnes-Jewish Hospital Foundation, and Siteman Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Toriola, A., Stolzenberg-Solomon, R., Dalidowitz, L. et al. Diabetes and pancreatic cancer survival: a prospective cohort-based study. Br J Cancer 111, 181–185 (2014). https://doi.org/10.1038/bjc.2014.224
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2014.224
Keywords
This article is cited by
-
Diabetes Status and Pancreatic Cancer Survival in the Nationwide Veterans Affairs Healthcare System
Digestive Diseases and Sciences (2023)
-
Impact of diabetes and modifiable risk factors on pancreatic cancer survival in a population-based study after adjusting for clinical factors
Cancer Causes & Control (2022)
-
Predictive Value of Serum Carbohydrate Antigen 19-9 (CA19-9) for Early Mortality in Advanced Pancreatic Cancer
Journal of Gastrointestinal Cancer (2018)
-
Exploring the bi-directional relationship between pancreatic cancer and diabetes mellitus: a retrospective study
Journal of Diabetes & Metabolic Disorders (2018)
-
Worsened outcome in patients with pancreatic ductal carcinoma on long-term diabetes: association with E-cadherin1 (CDH1) promoter methylation
Scientific Reports (2017)