Abstract
Background:
Plasma circulating tumour-specific microRNAs (miRNAs) are promising biomarkers of tumour presence and recurrence, especially for diseases whose best chance of successful treatment requires early diagnosis and timely surgery of an already malignant but not yet invasive tumour, such as colorectal cancer (CRC).
Methods:
Expression levels of miRNAs previously found to be differently expressed in tumour vs normal colon tissues were investigated by quantitative real-time PCR in plasma from CRC patients and from healthy donors and confirmed in independent case control series. The validated miRNAs were also measured after surgery. Analyses were repeated on the subsets of haemolysis-free samples.
Results:
We identified four miRNAs differently expressed between the compared groups, two (miR-21 and miR-378) of which were validated. miR-378 expression decreased in non-relapsed patients 4–6 months after surgery and miR-378 ability to discriminate CRC patients from healthy individuals was not influenced by haemolysis levels of plasma samples.
Conclusion:
The miRNA analysis on plasma samples represents a useful non-invasive tool to assess CRC presence as well as tumour-free status at follow-up. Plasma levels of miR-378 could be used to discriminate CRC patients from healthy individuals, irrespective of the level of haemoglobin of plasma samples.
Similar content being viewed by others
Main
Colorectal cancer (CRC) remains the second main cause of cancer death in western countries (Jemal et al, 2011). Despite significant advances in the management of CRC, early diagnosis and timely surgery of an already malignant but not yet invasive tumour still represent the best- and only-cure options (Center et al, 2009; Ferlay et al, 2010; Gellad and Provenzale, 2010). Available methodologies for early detection are still based on traditional screening methods such as the Faecal Occult Blood Test (FOBT) in average-risk populations followed by colonoscopy in the case of positivity. However, FOBT is neither very sensitive nor particularly specific, and colonoscopy, though specific and sensitive, is not suitable for screening in the general population because of low compliance rate and high costs. Therefore, there is an increased need for new markers for earlier disease detection and a more efficient monitoring during the follow-up period (McLoughlin and O'Morain, 2006; Burch et al, 2007).
Plasma/serum circulating microRNAs (miRNAs) are promising novel minimally invasive biomarkers for diagnosing and monitoring human cancers (Calin and Croce, 2006; Chen et al, 2008; Filipowicz et al, 2008; Mitchell et al, 2008). They are small non-coding RNAs (18–25 nucleotides long) that can promote mRNA degradation or regulate the translation of specific protein-coding genes (Kosaka et al, 2010). microRNAs have an important regulatory role in a wide range of biological and pathological processes and are involved in tumorigenesis and in the development of various cancers, and miRNA signatures related to tumour classification, diagnosis, and disease progression have been identified (Calin and Croce, 2006). Tumour-derived miRNAs are resistant to endogenous ribonuclease activity, as well as extreme pH and temperature and can therefore be present in plasma/serum in a remarkably stable form (Mitchell et al, 2008). Initially, this was explained by the packaging of miRNAs in some kinds of secretory particles including apoptotic bodies and exosomes in plasma/serum (Kosaka et al, 2010). Recent studies also found miRNAs in protein complexes including argonaute (AGO) or high-density lipoproteins (Arroyo et al, 2011; Vickers et al, 2011). In addition, the expression level of serum/plasma miRNAs is reproducible and consistent among individuals and miRNAs are measurable with a much greater sensitivity than proteins (Chen et al, 2008; Mitchell et al, 2008). The presence of circulating miRNAs that could be used for early detection of cancer has successfully been investigated in several malignancies such as prostate cancer, lymphoma, ovarian cancer, lung and breast cancer, gastric, oesophageal, and colorectal cancer (Cortez et al, 2011).
The identification of disease-specific miRNAs is hampered by the fact that blood also contains miRNAs derived from the haemolysis of cells of different hematopoietic origins, whose levels correlate with the blood cell count. Some of these cellular miRNAs are included in the lists of tumour-related miRNA circulating biomarkers reported in the literature, and differences in their levels might be related to blood cell events rather than the presence of cancer (Pritchard et al, 2012). One possible test method to avoid misidentification of non-specific miRNAs might be the measurement of haemoglobin levels as markers of haemolysis in plasma samples to determine whether they are suitable for miRNA analysis (Kirschner et al, 2011).
In this study, we investigated whether the plasma concentration of a group of miRNAs that were differently expressed in tumour vs normal colon tissues (Reid et al, 2012) could be used to screen for the presence of CRC or for monitoring recurrence. Our results provided evidence that the plasma level of miR-378 could be used to discriminate CRC patients from healthy individuals, irrespective of the level of haemoglobin of plasma samples and confirmed that miRNA analysis in plasma samples represents a useful non-invasive tool to detect CRC as well as to monitor recurrence.
Materials and methods
Patient cohort
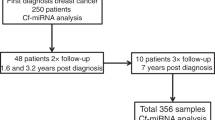
The study design, approved by the institutional review board of Fondazione IRCCS Istituto Nazionale dei Tumori Milano (INT), includes a total of 65 patients (cases). Peripheral blood was collected in EDTA tube the day before surgery (T0) and for 46 patients also 4–6 months after surgical resection (T1), during the scheduled medical examinations. Patients who had received preoperative radiotherapy or chemotherapy were excluded. Overall, a series of 70 blood donors recruited through the Transfusion Medicine Service of our Institute and the Associazione Volontari Italiani Sangue of Milan who appeared to be disease free by routine serological and instrumental analyses were considered as a normal control. The distribution of sex and age was quite comparable in cases and controls.
All samples were collected at INT between 2009 and 2011 and each patient and donor provided written informed consent to donate blood samples for research purposes. Tumours were classified according to Dukes classification (Dukes, 1932), 54% of them were stages I and II, the remaining were at stages III and IV. Plasma was immediately separated from the cellular fraction by centrifugation at 3000 g for 10 min at room temperature and stored at −80 °C. An additional centrifugation (1000 g for 5 min at 4 °C) was performed before RNA extraction to remove cell debris.
Free haemoglobin concentrations in plasma samples were analysed by spectrophotometric analysis. The ratio between the absorbance peaks at 414 and 375 nm, suggestive of the presence of free haemoglobin, was used for quantitative determination of haemolysis (Kirschner et al, 2011). Samples with a haemolysis ratio of ⩽2 were considered as haemolysis free. Starting from the overall cohort of 135 subjects (65 cases and 70 controls) the training and the validation sets were selected.
Nucleic acids extraction and plasma RNA quantification
Total RNA (including small RNAs) was extracted from 400 μl of plasma. Trizol reagent (Invitrogen, Carlsbad, CA, USA) and the miRNeasy Mini Kit (Qiagen, Chatsworth, CA, USA) were used for samples included in the training set, with the following modifications: Trizol was added to plasma samples in a ratio of 3 : 1. After chloroform addition and centrifugation at 16 100 g for 15 min at 4 °C, nucleic acids were precipitated at −80 °C with 1.5 volumes of 96% ethanol and isolated on miRNeasy columns. DNAse treatment was carried out following the manufacturer’s instructions. Qiazol Lysis reagent (Qiagen) added with the MS2 RNA Carrier (Roche Applied Science, Milan, Italy) and the miRNeasy Mini Kit modified by Exiqon (Vedbaek, Denmark; ‘RNA Purification from blood and Serum Protocol’) were used for samples from the validation set and for samples collected after surgery. Qiazol mixture was combined to plasma in a ratio of 3.75 : 1. Centrifugation was done at 12 000 g for 15 min at 4 °C and samples were washed three times with 500 μl of RPE buffer. RNA was eluted in 40 μl of water pre-warmed at 42 °C.
miRNA quantitative real-time PCR
Taqman MicroRNA Assays were used for miRNA quantification. In brief, 2 μl of RNA was reverse transcribed to cDNA using the High-Capacity cDNA Reverse Transcription Kit and miRNA-specific primers (Applied Biosystems, Foster City, CA, USA) according to the manufacturer’s instructions in a reaction volume of 15 μl. qPCR was done using the FAST chemistry (Applied Biosystems) with the manufacturer provided miRNA-specific assays in ABI PRISM 7900 HT Real-Time PCR system (Applied Biosystems). The assays analysed are listed in Table 1.
miR-29a and miR-92 were tested using the Qiagen technology as reported by Huang et al (2010) and Ng et al (2009). Briefly, 4 μl of RNA was reverse transcribed to cDNA using the miScript Reverse Transcription Kit (Qiagen) according to the manufacturer’s instructions in a reaction volume of 20 μl. SYBR Green chemistry (Qiagen) was used to perform the qPCR with the manufacturer provided miScript Universal Primer and miScript Primer Assay in LightCycler 480 II Roche.
Statistical analysis
The relative quantity (RQ) of each miRNA was calculated using the comparative threshold cycle (Ct) method with the equation 2−ΔCt, where ΔCt=Ct miRNA−Ct miRNA-16 (Livak and Schmittgen, 2001). The association between the RQ, expressed in logarithmic scale (log2 RQ=−ΔCt), of each miRNA and the risk of colon cancer was evaluated by resorting to a univariate logistic regression model (Hosmer and Lemeshow, 1989) that estimates odds ratio (OR) and its 95% confidence intervals (CIs). We implemented this model in the training set to first select the promising miRNAs. These miRNAs were then evaluated in the validation set. Next, receiver operating characteristic (ROC) curves were implemented for the validated miRNA(s) and the area under the ROC curve (AUC), with the corresponding 95% CI, was estimated to assess their predictive capability (Harrell et al, 1982). For the 46 patients where peripheral blood was collected both the day before surgery (T0) and 4–6 months after surgery (T1) the RQ of the validated miRNA(s) was compared using a mixed regression model (McCulloch and Searle, 2001) with patient as the random factor and time (T0 vs T1) as the fixed factor. Statistical analyses were performed by the SAS software v. 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
Selection of tumour-associated miRNAs
Twenty-five miRNAs differentially expressed in tumour vs normal colon tissue (Schetter et al, 2008; Reid et al, 2012) or previously found in plasma of CRC patients (Ng et al, 2009; Huang et al, 2010) were selected to evaluate their possible use as circulating biomarkers of CRC (see Table 1). A pilot analysis, performed on RNA extracted from plasma of 10 patients with CRC and from 10 healthy donors, showed that 17 of the analysed miRNAs were expressed at detectable levels (mean Ct values <34) also in the plasma (see Table 1). Among them, miR-885-5p presented a detection rate of <50% in both control and CRC plasma samples and was discarded.
Identification of CRC-related plasma circulating miRNAs
Expression of the 16 selected miRNAs was measured in the training and validation sets. The miRNAs that resulted different among patients and healthy individuals also in the validation set were tested on plasma collected 4–6 months after surgery from disease-free patients.
Training set
In Figure 1 are reported the ORs and the corresponding 95% CI obtained from the univariate logistic model implemented for each of the 16 miRNAs evaluated in the training set consisting of plasma samples from 36 patients with cancer and from 41 donors. The four miRNAs with an OR significantly different from 1.00 were miR-21, miR-135b, miR-378, and miR-204. The distributions of the RQ of these miRNAs in cases and controls are shown in Figure 2 by box-plots. miR-204 and miR-378 were not detected in two controls and miR-135 in three controls. All the data were available for miR-21. The median RQ was higher in cases than in controls for miR-135b, miR-21, and miR-378.
Distribution of the relative quantity of the four relevant miRNAs in the training set. Box-plots reflect the distribution in cases and controls of the relative quantity of the miRNAs with odds ratio statistically significant in the training set. Each box indicates the 25th and 75th percentiles of the distribution. The horizontal line inside the box indicates the median, and the whiskers indicate the extreme measured values. Each individual value is represented by a dot.
Validation set
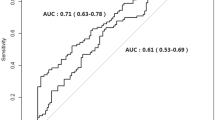
In Table 2 are presented the results of the univariate logistic models and the AUC for the four selected miRNAs in the validation set, consisting in a total of 58 samples including 29 cases from cancer patients and 29 from controls. From this analysis, it appears that the OR of miR-21 and miR-378 remains statistically significant in the validation set. For both these miRNAs, we observed a significant predictive capability to discriminate between case and control with a lower limit of AUC 95% CI>0.5 (Table 2). In particular, miR-378 has the highest predictive capability (AUC 95% CI: 0.68–0.91). Figure 3 reports the ROC curves (panels B and D) and the box-plots (panels A and C) of the RQ of the two validated miRNAs. The level of correlation between the two validated miRNAs was moderate (Spearman’s correlation coefficient: 0.26; 95% CI: 0.005–0.488), and in the logistic model including both miRNAs only miR-378 maintains its significance with an OR similar to that obtained in the univariate model (miR-21: OR=1.59, 95% CI: 0.69–3.64; miR-378: OR=4.03, 95% CI: 1.67–9.73).
Distribution of the relative quantity of the two validated miRNAs and the corresponding receiver operating characteristic (ROC) curves. (A and C) The box-plots reflect the distribution in cases and controls of the relative quantity of miR-378 (A) and miR-21 (C) in the validation set. Each box indicates the 25th and 75th percentiles of the distribution. The horizontal line inside the box indicates the median, and the whiskers indicate the extreme measured values. (B and D) The ROC curves derived from the univariate logistic analysis in the validation set for miR-378 (B) and miR-21 (D), respectively.
Analysis of miRNA expression after CRC surgery
To assess the possible value of the two validated miRNAs in monitoring outcome after surgery, we measured their expression levels in plasma from 46 patients undergoing planned surgery, collected the day before surgery (T0) and 4–6 months after surgery (T1) during scheduled clinical evaluation, and the relative expression levels at the two time points were compared. All the patients analysed at T1 were disease free. A statistically significant reduction was observed for miR-378 after surgery (P-value=<0.0001), whereas the expression of miR-21 was not significantly different at the two considered time points (P-value=0.8611). Figure 4 reports the box-plot of the relative expression of miR-378 according to the two time points.
Distribution of the relative quantity of miR-378 in plasma collected before and after surgery. Box-plot reflects the distribution of the relative quantity of miR-378 in plasma collected the day before surgery (T0) and 4–6 months after it (T1) in disease-free patients. Each box indicates the 25th and 75th percentiles of the distribution. The horizontal line inside the box indicates the median, and the whiskers indicate the extreme measured values. Each individual value is represented by a dot and the two points corresponding to the same individual are connected by a line.
Identification of CRC-related circulating miRNAs in the haemolysis-free subgroup
Data were analysed by considering only haemolysis-free cases (haemolysis ratio ⩽2, measured as described in Materials and Methods).
From the training set, we selected the 24 cancer patients and 19 donor samples with a haemolysis ratio of ⩽−2 and implemented a univariate logistic regression model for each of the 16 considered miRNAs. The only two miRNAs with an OR significantly different from 1.00 were miR-21 (OR: 2.83; 95% CI: 1.42–5.63; P-value=0.003) and miR-378 (OR: 3.43; 95% CI: 1.27–9.26; P-value=0.015). For both of them, median relative expression was higher in cases than in controls (see Supplementary Figure 1). Expression of miR-21 and miR-378 was compared by considering 18 cancer patients and 20 controls with a haemolysis ratio of ⩽2 from the validation set. The results of the univariate logistic models showed that only miR-378 remains statistically significant (OR: 3.03; 95% CI: 1.17–7.86, P-value=0.023). The ROC analysis confirmed also the significant predictive capability of miR-378 (AUC 0.74; 95% CI: 0.58–0.90). Supplementary Figure 2 reports the ROC curve (panel B) and the box-plot (panel A) of the relative expression of miR-378.
Analysis of the expression levels of miR-378 in plasma collected after surgery from the 21 patients with a haemolysis ratio of ⩽2 at both collection times (the day before surgery and 4–6 months after it) confirmed a statistically significant reduction in the expression of miR-378 after cancer removal (P-value=0.0002). Supplementary Figure 3 reports the box-plot of the relative expression of miR-378 according to the two time points.
Discussion
Tumour-specific alterations in nucleic acids detectable in the plasma of cancer patients are promising non-invasive biomarkers for diagnosis and for monitoring of various cancers (Frattini et al, 2008). Tumour-derived miRNAs have been found in plasma, where they show tissue-specific signatures and exhibit high stability compared with circulating DNA and mRNA (Mitchell et al, 2008), highlighting their possible use as new biomarkers for identifying patients with cancer.
To find possible CRC-derived circulating miRNAs, we focused on plasma levels of a set of 23 tumour-associated miRNAs differently expressed between matched normal and tumoral colorectal tissues we had previously identified (Reid et al, 2012). Among the top miRNAs differentially expressed in tumours reported in the work of Schetter et al (2008), we included miR-93, as well as miR-29a, miR-92, and miR-203 that have been described in plasma from CRC patients (Ng et al, 2009; Huang et al, 2010). Sixteen of the analysed miRNAs were expressed at detectable levels also in plasma, supporting the hypothesis that CRC cells can release miRNAs. Four of them, miR-135b, miR-204, miR-21, and miR-378, were present at significant different levels in plasma from cancer patients, in comparison with cancer-free individuals. miR-21 and miR-378 confirmed these results in an independent cohort of samples, selected with the same criteria as the test set, thus providing strong evidence that miR-21 and miR-378 are valid plasma markers of the presence of CRC. Among the two miRNAs, miR-378 has the highest predictive capability (AUC=0.796). Results were further confirmed when 12 more cases and 13 control samples were added to the validation set (data not shown). In addition, plasma levels of miR-378 significantly decreased after surgical removal of CRCs, indicating that this miRNA is also a potential marker for monitoring therapeutic outcome.
A comparison between the predictive capability of the two identified miRNAs and other known CRC biomarkers shows that miR-378 predicts the presence of CRC similarly to DNA methylation markers (Lange et al, 2012), while miR-21 has a predictive value similar to ctDNA (Perrone et al, in press).
No significant association was observed between miR-378 and miR-21 expression among the different tumour stages of the cases, categorised as early (stages I and II) and late (stages III and IV) (data not shown), suggesting that the two miRNAs could potentially be used as novel non-invasive biomarkers for early CRC detection after successful treatment. This possibility needs to be further investigated in larger case series. In addition, patients included in this study are under follow-up at our Institute and therefore we will also be able to assess the predictive value of recurrence of the two markers.
Previous studies identified CRC-related circulating miRNAs: Ng et al (2009) found that miR-92a was significantly increased in CRC patients plasma and its levels decreased after surgery, suggesting that plasma miRNAs may be used to monitor cancer patients. Huang et al (2010) found that miR-29a and miR-92a levels were higher in plasma from patients with advanced CRC than in plasma samples from healthy individuals and differentiated advanced adenomas from normal controls. miR-29a was also found higher in serum of CRC patients carrying liver metastases (Wang and Gu, 2012). Other researchers found an association between CRC and expression of miR-221 in directly amplified plasma (Pu et al, 2010). The three miRNAs were included in the set we analysed, but were not specifically associated with CRC, as also found by Faltejskova et al (2012). Possible reasons for these discrepancies could be the different methods used for RNA extraction and miRNA detection, although miR-92a was analysed using the same technology of Huang et al (2010) and Ng et al (2009), or differences in the endogenous controls used for normalisation. The genetic variations among different ethnic groups and environmental factors may also contribute to the differing results.
Another strong possible explanation of the discrepancies comes from recent studies on the origin of the miRNAs reported in the literature as circulating cancer biomarkers. These studies indicate that the majority of those miRNAs do not have a tumour cell-specific origin and may derive from the rupture of blood cells still present in plasma (haemolysis) because of collection procedures or specimen processing conditions (Pritchard et al, 2012), thus impacting on their possible use as tumour biomarkers. Interestingly, miR-92a, miR-29a, and miR-221 are expressed by red blood cells (Pritchard et al, 2012) and miR-92a is strongly affected by haemolysis. The fact that the range of haemolysis ratio in our cases was quite narrow (from 1.03 to 2.53 for cases and from 1.11 to 3.05 for controls in the training set and from 1.18 to 2.90 for cases and from 1.03 to 2.74 for controls in the validation set) could also explain why we did not confirm the three miRNAs as CRC biomarkers.
When we considered samples with haemolysis ratio ⩽2 (24 cases and 19 controls in the training set and 18 cases and 20 controls in the validation set), only miR-378 was confirmed as a CRC biomarker also able to monitor therapeutic outcome. Since miR-21 has recently been found expressed by red blood cells (Kirschner et al, 2013), we cannot exclude that the result we observed in the whole case series is linked to the few haemolysed samples present. Alternatively, the reduced number of haemolysis-free samples was insufficient to highlight differences between cases and controls.
Normalisation was done using miR-16 as an internal control, according to the initial studies on plasma circulating miRNAs (Mitchell et al, 2008), and under the same conditions as the first studies on plasma from CRC patients, to compare the obtained results (Chang et al, 2010; Huang et al, 2010). Plasma levels of miR-16 are affected by haemolysis (Pritchard et al, 2012), but the levels of haemolysis observed in our samples were so low as to justify their inclusion in our analysis. In fact, Kirschner et al (2011) have shown that, in the absence of haemolysis, the levels of miR-16 are sufficiently constant to serve as a normaliser.
Regarding the two miRNAs we found highly expressed in plasma from CRC patients, miR-21 is an oncogenic miRNA altered in many tumours that regulates the expression of multiple cancer-related target genes such as PTEN and TPM1 (Meng et al, 2007; Zhu et al, 2007). Several studies have highlighted the potential of miR-21 as a highly promising prognostic marker. In fact, we and others found that miR-21 is upregulated in CRCs tumours compared with matched non-tumour tissues (Schetter et al, 2008; Reid et al, 2012) and its expression increases during tumour progression (Schetter et al, 2008). In addition, higher miR-21 levels in primary tumours were correlated with shorter disease-free interval (Kulda et al, 2010) and high miR-21 expression was associated with poor response to adjuvant therapy and more rapid recurrence in patients with stage III disease (Schetter et al, 2008). miR-21 is highly expressed in serum from several cancers including CRC, breast, oesophageal, gastric, and lung cancer (Wang and Zhang, 2012) and has also been found higher in plasma from 30 CRC carrying patients (Kanaan et al, 2012).
miR-378 was overexpressed in plasma from CRC patients and its levels were strongly reduced after surgery; it is a target of the c-Myc oncoprotein and can promote cellular transformation, at least in part, by targeting and inhibiting TOB2, an anti-proliferative member of the BTG family that could repress cyclin D1 transcription (Feng et al, 2011). This miRNA targets the tumour suppressor genes Sufu and Fus-1 and can enhance cell survival, tumour growth, and angiogenesis (Lee et al, 2007). miR-378 was higher in serum from patients with renal cell carcinoma (Redova et al, 2012) and in serum from gastric cancer patients than in healthy individuals (Liu et al, 2012). Similarly to what has been observed for gastric and renal cancer (Chow et al, 2010; Redova et al, 2012) miR-378 is downregulated in CRC tissues (Reid et al, 2012; Mazeh et al, 2013). Regarding gastric cancer, some authors speculated that cancer cells may selectively release or capture cellular miRNAs, resulting in increased (as for miR-378) or decreased serum miRNA levels with respect to tumour tissue. Further analyses are needed to clarify the existence of a cellular mechanism that selects and regulates miRNA circulation.
Our study suggests that the ongoing search for plasma miRNA markers can be a fruitful approach. Our results, further validated in an independent cohort of samples, show that plasma circulating miR-378 could be a valuable haemolysis-free biomarker for the early detection and monitoring of CRC. Even if our observations are promising, further large-scale prospective studies are necessary to validate miR-378 clinical potential as a non-invasive, cost-effective screening tool for CRC.
Change history
18 February 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Arroyo JD, Chevillet JR, Kroh EM, Ruf IK, Pritchard CC, Gibson DF, Mitchell PS, Bennett CF, Pogosova-Agadjanyan EL, Stirewalt DL, Tait JF, Tewari M (2011) Argonaute2 complexes carry a population of circulating microRNAs independent of vesicles in human plasma. Proc Natl Acad Sci USA 108 (12): 5003–5008.
Burch JA, Soares-Weiser K, John DJS, Duffy S, Smith S, Kleijnen J, Westwood M (2007) Diagnostic accuracy of faecal occult blood tests used in screening for colorectal cancer: a systematic review. J Med Screen 14: 132–137.
Calin GA, Croce CM (2006) MicroRNA signatures in human cancers. Nat Rev Cancer 6 (11): 857–866.
Center MM, Jemal A, Smith RA, Ward E (2009) Worldwide variations in colorectal cancer. CA Cancer J Clin 59 (6): 366–378.
Chang KH, Mestdagh P, Vandesompele J, Kerin MJ, Miller N (2010) MicroRNA expression profiling to identify and validate reference genes for relative quantification in colorectal cancer. BMC Cancer 10: 173.
Chen X, Ba Y, Ma L, Cai X, Yin Y, Wang K, Guo J, Zhang Y, Chen J, Guo X, Li Q, Li X, Wang W, Wang J, Jiang X, Xiang Y, Xu C, Zheng P, Zhang J, Li R, Zhang H, Shang X, Gong T, Ning G, Zen K, Zhang CY (2008) Characterization of microRNAs in serum: a novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res 18 (10): 997–1006.
Chow TF, Mankaruos M, Scorilas A, Youssef Y, Girgis A, Mossad S, Metias S, Rofael Y, Honey RJ, Stewart R, Pace KT, Yousef GM (2010) The miR-17-92 cluster is over expressed in and has an oncogenic effect on renal cell carcinoma. J Urol 183 (2): 743–751.
Cortez MA, Bueso-Ramos C, Ferdin J, Lopez-Berestein G, Sood AK, Calin GA (2011) MicroRNAs in body fluids—the mix of hormones and biomarkers. Nat Rev Clin Oncol 8 (8): 467–477.
Dukes C (1932) The classification of cancer of the rectum. J Pathol Bacteriol 35: 323.
Faltejskova P, Bocanek O, Sachlova M, Svoboda M, Kiss I, Vyzula R, Slaby O (2012) Circulating miR-17-3p, miR-29a, miR-92a and miR-135b in serum: evidence against their usage as biomarkers in colorectal cancer. Cancer Biomark 12 (4): 199–204.
Feng M, Li Z, Aau M, Wong CH, Yang X, Yu Q (2011) Myc/miR-378/TOB2/cyclin D1 functional module regulates oncogenic transformation. Oncogene 30 (19): 2242–2251.
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127 (12): 2893–2917.
Filipowicz W, Bhattacharyya SN, Sonenberg N (2008) Mechanisms of post-transcriptional regulation by microRNAs: are the answers in sight? Nat Rev Genet 9 (2): 102–114.
Frattini M, Gallino G, Signoroni S, Balestra D, Lusa L, Battaglia L, Sozzi G, Bertario L, Leo E, Pilotti S, Pierotti MA (2008) Quantitative and qualitative characterization of plasma DNA identifies primary and recurrent colorectal cancer. Cancer Lett 263 (2): 170–181.
Gellad ZF, Provenzale D (2010) Colorectal cancer: national and international perspective on the burden of disease and public health impact. Gastroenterology 138 (6): 2177–2190.
Harrell FE Jr, Califf RM, Pryor DB, Lee KL, Rosati RA (1982) Evaluating the yield of medical tests. JAMA 247 (18): 2543–2546.
Hosmer D, Lemeshow S (1989) Applied Logistic Regression Vol. 10. John Wiley & Sons: New York, NY, USA.
Huang Z, Huang D, Ni S, Peng Z, Sheng W, Du X (2010) Plasma microRNAs are promising novel biomarkers for early detection of colorectal cancer. Int J Cancer 127 (1): 118–126.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61 (2): 69–90.
Kanaan Z, Rai SN, Eichenberger MR, Roberts H, Keskey B, Pan J, Galandiuk S (2012) Plasma miR-21: a potential diagnostic marker of colorectal cancer. Ann Surg 256 (3): 544–551.
Kirschner MB, Edelman JJ, Kao SC, Vallely MP, van Zandwijk N, Reid G (2013) The Impact of Hemolysis on Cell-Free microRNA Biomarkers. Front Genet 4: 94.
Kirschner MB, Kao SC, Edelman JJ, Armstrong NJ, Vallely MP, van Zandwijk N, Reid G (2011) Haemolysis during sample preparation alters microRNA content of plasma. PLoS One 6 (9): e24145.
Kosaka N, Iguchi H, Ochiya T (2010) Circulating microRNA in body fluid: a new potential biomarker for cancer diagnosis and prognosis. Cancer Sci 101 (10): 2087–2092.
Kulda V, Pesta M, Topolcan O, Liska V, Treska V, Sutnar A, Rupert K, Ludvikova M, Babuska V, Holubec L Jr, Cerny R (2010) Relevance of miR-21 and miR-143 expression in tissue samples of colorectal carcinoma and its liver metastases. Cancer Genet Cytogenet 200 (2): 154–160.
Lange CP, Campan M, Hinoue T, Schmitz RF, van der Meulen-de Jong AE, Slingerland H, Kok PJ, van Dijk CM, Weisenberger DJ, Shen H, Tollenaar RA, Laird PW (2012) Genome-scale discovery of DNA-methylation biomarkers for blood-based detection of colorectal cancer. PLoS One 7 (11): e50266.
Lee DY, Deng Z, Wang CH, Yang BB (2007) MicroRNA-378 promotes cell survival, tumor growth, and angiogenesis by targeting SuFu and Fus-1 expression. Proc Natl Acad Sci USA 104 (51): 20350–20355.
Liu H, Zhu L, Liu B, Yang L, Meng X, Zhang W, Ma Y, Xiao H (2012) Genome-wide microRNA profiles identify miR-378 as a serum biomarker for early detection of gastric cancer. Cancer Lett 316 (2): 196–203.
Livak K, Schmittgen T (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T). Methods 25 (4): 402–408.
Mazeh H, Mizrahi I, Ilyayev N, Halle D, Brucher B, Bilchik A, Protic M, Daumer M, Stojadinovic A, Itzhak A, Nissan A (2013) The diagnostic and prognostic role of microRNA in colorectal cancer - a comprehensive review. J Cancer 4 (3): 281–295.
McCulloch C, Searle S (2001) Generalized, Linear, and Mixed Models.. Wiley Series in Probability and Statistics: New York, NY, USA.
McLoughlin RM, O'Morain CA (2006) Colorectal cancer screening. World J Gastroenterol 12 (42): 6747–6750.
Meng F, Henson R, Wehbe-Janek H, Ghoshal K, Jacob ST, Patel T (2007) MicroRNA-21 regulates expression of the PTEN tumor suppressor gene in human hepatocellular cancer. Gastroenterology 133 (2): 647–658.
Mitchell PS, Parkin RK, Kroh EM, Fritz BR, Wyman SK, Pogosova-Agadjanyan EL, Peterson A, Noteboom J, O'Briant KC, Allen A, Lin DW, Urban N, Drescher CW, Knudsen BS, Stirewalt DL, Gentleman R, Vessella RL, Nelson PS, Martin DB, Tewari M (2008) Circulating microRNAs as stable blood-based markers for cancer detection. Proc Natl Acad Sci USA 105 (30): 10513–10518.
Ng EK, Chong WW, Jin H, Lam EK, Shin VY, Yu J, Poon TC, Ng SS, Sung JJ (2009) Differential expression of microRNAs in plasma of patients with colorectal cancer: a potential marker for colorectal cancer screening. Gut 58 (10): 1375–1381.
Perrone F, Lampis A, Bertan C, Verderio P, Ciniselli CM, Pizzamiglio S, Frattini M, Nucifora M, Molinari F, Gallino G, Gariboldi M, Meroni M, Leo E, Pierotti MA, Pilotti S (in press) Circulating Free DNA in a screening programme for early colorectal cancer detection. Tumori.
Pritchard CC, Kroh E, Wood B, Arroyo JD, Dougherty KJ, Miyaji MM, Tait JF, Tewari M (2012) Blood cell origin of circulating microRNAs: a cautionary note for cancer biomarker studies. Cancer Prev Res (Phila) 5 (3): 492–497.
Pu XX, Huang GL, Guo HQ, Guo CC, Li H, Ye S, Ling S, Jiang L, Tian Y, Lin TY (2010) Circulating miR-221 directly amplified from plasma is a potential diagnostic and prognostic marker of colorectal cancer and is correlated with p53 expression. J Gastroenterol Hepatol 25 (10): 1674–1680.
Redova M, Poprach A, Nekvindova J, Iliev R, Radova L, Lakomy R, Svoboda M, Vyzula R, Slaby O (2012) Circulating miR-378 and miR-451 in serum are potential biomarkers for renal cell carcinoma. J Transl Med 10: 55.
Reid JF, Sokolova V, Zoni E, Lampis A, Pizzamiglio S, Bertan C, Zanutto S, Perrone F, Camerini T, Gallino G, Verderio P, Leo E, Pilotti S, Gariboldi M, Pierotti MA (2012) miRNA profiling in colorectal cancer highlights miR-1 involvement in MET-dependent proliferation. Mol Cancer Res 10 (4): 504–515.
Schetter AJ, Leung SY, Sohn JJ, Zanetti KA, Bowman ED, Yanaihara N, Yuen ST, Chan TL, Kwong DL, Au GK, Liu CG, Calin GA, Croce CM, Harris CC (2008) MicroRNA expression profiles associated with prognosis and therapeutic outcome in colon adenocarcinoma. JAMA 299 (4): 425–436.
Vickers KC, Palmisano BT, Shoucri BM, Shamburek RD, Remaley AT (2011) MicroRNAs are transported in plasma and delivered to recipient cells by high-density lipoproteins. Nat Cell Biol 13 (4): 423–433.
Wang B, Zhang Q (2012) The expression and clinical significance of circulating microRNA-21 in serum of five solid tumors. J Cancer Res Clin Oncol 138 (10): 1659–1666.
Wang LG, Gu J (2012) Serum microRNA-29a is a promising novel marker for early detection of colorectal liver metastasis. Cancer Epidemiol 36 (1): e61–e67.
Zhu S, Si ML, Wu H, Mo YY (2007) MicroRNA-21 targets the tumor suppressor gene tropomyosin 1 (TPM1). J Biol Chem 282 (19): 14328–14336.
Acknowledgements
We wish to thank Dr Andrea Lampis from the Laboratory of Experimental Molecular Pathology for help in blood sample handling and storage, the Real Time PCR Unit of the Technological Service at IFOM and Dr Daniela Majerna from the Scientific Directorate for her assistance in the preparation of the manuscript. This work was supported by grants from Associazione Italiana per la Ricerca sul Cancro (AIRC) (Grants no. 10529 and no. 12162) and funds obtained through a law by the Italian government which allowed Italian citizens to allocate the 5 × 1000 share of their tax payment to support a research or charitable institution of their choice.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Zanutto, S., Pizzamiglio, S., Ghilotti, M. et al. Circulating miR-378 in plasma: a reliable, haemolysis-independent biomarker for colorectal cancer. Br J Cancer 110, 1001–1007 (2014). https://doi.org/10.1038/bjc.2013.819
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.819
Keywords
This article is cited by
-
Anesthetics may modulate cancer surgical outcome: a possible role of miRNAs regulation
BMC Anesthesiology (2021)
-
The miR-378c-Samd1 circuit promotes phenotypic modulation of vascular smooth muscle cells and foam cells formation in atherosclerosis lesions
Scientific Reports (2021)
-
A microRNA panel compared to environmental and polygenic scores for colorectal cancer risk prediction
Nature Communications (2021)
-
Overexpression of miR-378 Alleviates Chronic Sciatic Nerve Injury by Targeting EZH2
Neurochemical Research (2021)
-
Faecal microRNAs as a non-invasive tool in the diagnosis of colonic adenomas and colorectal cancer: A meta-analysis
Scientific Reports (2019)