Abstract
Background:
Early detection of recurrence of head and neck squamous cell carcinoma (HNSCC), which is often obscured by surgical or radiotherapy-induced tissue distortion, is essential for proper patient management.
Methods:
A total of 143 consecutive patients with previously untreated HNSCC were evaluated by whole-body fluorine 18-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) and regular clinical follow-up after curative treatment. The 18F-FDG PET/CT was performed ∼3–6 and 12 months after treatment and findings suspicious for recurrence or SPC were confirmed using histopathology.
Results:
The sensitivities of 3–6- and 12-month PET/CT scans at patient level were 96% and 93%, respectively, and those of regular clinical follow-up were 11% and 19%, respectively (McNemar test, P<0.001). In patients with no clinical suspicion, PET/CT detected 95% and 91% of recurrent patients at 3–6 and 12 months, respectively. The sensitivity of PET/CT for the identification of SPC was 29% and 80% at 3–6 and 12 months, respectively. A positive interpretation of PET/CT was significantly associated with poor overall survival (log-rank test, P<0.001).
Conclusion:
The 18F-FDG PET/CT surveillance is beneficial for the detection of recurrence that may be missed by regular follow-up physical and endoscopic examinations of the head and neck area after curative treatment for HNSCC.
Similar content being viewed by others
Main
Head and neck cancer describes a group of tumours that arise in the upper aerodigestive tract including the larynx, pharynx, oral cavity, nasal cavity, and paranasal sinus, and the predominant histological type is squamous cell carcinoma. Head and neck squamous cell carcinoma (HNSCC) is the eighth most common cancer worldwide, with more than half a million patients diagnosed each year (Jemal et al, 2011). Tobacco and alcohol consumption increases the risk of developing HNSCC, and oncogenic human papilloma virus is associated with a high risk of oropharyngeal cancer (Pai and Westra, 2009). Approximately two-thirds of HNSCC patients are initially diagnosed with advanced-stage disease including regional lymph node metastasis. Patients with HNSCC are usually treated by a multidisciplinary approach involving surgery, radiotherapy, and chemotherapy (Argiris et al, 2008; Haddad and Shin, 2008).
Despite the aggressive multimodal approach, the locoregional recurrence rate remains high in up to 54% of patients with advanced HNSCC, and distant metastases, which are less frequent, are reported in ∼5% to 10% of HNSCC patients (Ang et al, 2001; Xu et al, 2011). Moreover, recurrence occurs predominantly within the first 2 years after curative treatment (Leemans et al, 1994). Early detection of recurrent disease or second primary cancers may provide a chance of cure by early salvage treatment, and potentially a survival benefit (Wong et al, 2003). However, postsurgical and radiation-induced changes in the normal tissues may interfere with the early detection of recurrence by regular standard examinations of the head and neck including physical examination, endoscopy, computed tomography (CT) and magnetic resonance imaging (MRI) (Lell et al, 2000).
The development of fluorine 18-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET) or PET/CT has improved the post-treatment detection of residual or recurrent disease. The 18F-FDG PET or PET/CT is capable of distinguishing post-treatment tissue changes from recurrence that is undetectable by routine clinical follow-up of physical examination, CT, or MRI (Salaun et al, 2007; Abgral et al, 2009; Krabbe et al, 2009; Zundel et al, 2011; Ho et al, 2013). Therefore, 18F-FDG PET or PET/CT should be used after treatment as a sequential diagnostic tool regardless of the clinical suspicion of recurrence.
Currently, no clear consensus exists regarding the interval and frequency of 18F-FDG PET or PET/CT scans for post-treatment surveillance in HNSCC patients. A prospective study involving 48 oral and oropharyngeal SCC patients undergoing curative treatment recommended systematic 18F-FDG PET scanning 3–6 months after treatment (Krabbe et al, 2009). Another prospective study that included 53 patients without clinically apparent recurrence proposed the systematic use of 18F-FDG PET/CT at 12 months after treatment (Abgral et al, 2009). However, the use of post-treatment 18F-FDG PET/CT in HNSCC patients needs to be further examined. In the present study, we evaluated the diagnostic value of 18F-FDG PET/CT at 3–6 and 12 months after treatment for the detection of recurrence and second primary cancers in patients with HNSCC who underwent curative treatment. The early detection of recurrence is of value to guide clinicians in the management of these patients.
Materials and methods
Patients
Consecutive patients who were treated curatively for HNSCC from October 2009 to September 2010 at Asan Medical Center were reviewed. Inclusion criteria were previously untreated HNSCC, undergoing curative treatment, 3–6- or 12-month post-treatment imaging with whole-body 18F-FDG PET/CT, and complete follow-up of at least 18 months after completion of treatment. Not eligible for inclusion were patients with distant metastasis at the initial staging and those treated with palliative intent. Tumours were staged according to the tumour–node–metastasis (TNM) staging system (7th edition, 2010) of the American Joint Committee on Cancer (AJCC) (Edge et al, 2010). Study protocols were reviewed and approved by the Institutional Review Board of Asan Medical Center and the informed consent required from each patient was waived.
Follow-up
After initial therapy with curative intent, patients were regularly followed by clinical examination and serial 18F-FDG PET/CT scanning. All eligible patients were examined by palpation of all anatomic subsites of the head and neck and an endoscopic examination of the nasal and oral cavity, pharynx, and larynx at every clinic visit after curative treatment. The patients were scheduled for clinic visits every 1 to 2 months during the first year, every 2 to 4 months during the second and third years, and every 6 months during the fourth and fifth years. Regardless of the clinical suspicion of recurrence, a systematic follow-up protocol was established in our institution consisting of whole-body 18F-FDG PET/CT with/without head and neck CT/MRI at ∼3–6 and 12–18 months after curative therapy. Flexible esophagogastroduodenoscopy was performed annually.
The presence of clinical or imaging findings suggestive of local or regional recurrence, distant metastasis, or a second primary tumour was confirmed by biopsies. In cases of suspicious findings outside the head and neck region, the appropriate specialists examined the patient to confirm the lesions. Patients with confirmed recurrence or a second primary tumour were scheduled for salvage or palliative treatment. The positive results of regular follow-up or 18F-FDG PET/CT scan were compared with the gold standard, namely the outcome of biopsies and imaging follow-up.
18F-FDG PET/CT imaging and interpretation
The patients received whole-body 18F-FDG PET/CT scans using a multi-slice PET/CT camera system (Biograph Sensation 16 and Truepoint 40, Siemens Medical System, Knoxville, TN, USA; or Discovery STE 8, GE Healthcare, Milwaukee, WI, USA) equipped with 16-, 40-, or 8-slice CT scanners. All patients fasted for at least 6 h before 18F-FDG PET scanning and whole-blood glucose concentrations were <150 mg dl−1 before scanning. Whole-body image acquisition was started ∼60 min after intravenous injection of 370–555 MBq. The 18F-FDG/CT scanning without contrast enhancement was performed in spiral mode from the skull to the proximal thigh for attenuation correction and image fusion, followed by three-dimensional caudocranial PET scanning. The emission scan time per bed position was 2.5 min, and six or eight bed positions were used. The PET data were reconstructed using a standard iterative algorithm with attenuation correction based on the CT data.
A nuclear medicine physician with more than 15 years of experience interpreted the PET or PET/CT images by visual inspection. Foci with increased 18F-FDG uptake in the primary tumours and metastatic nodes were evaluated and compared with the background and blood pool activities. Image interpretation was based on visual and semiquantitative analyses of abnormally increased focal 18F-FDG uptakes but no strict standardised uptake value cutoffs were used. Local, regional, and distant sites were independently assessed and the presence of any primary site tumours, metastatic lymph nodes or soft tissues of the neck, and distant site of each patient was recorded.
Statistical analysis
Any 18F-FDG PET/CT findings suspicious for recurrence or a second primary cancer were confirmed by histopathology. Patients showing negative 18F-FDG PET/CT results were regularly followed to confirm the absence of recurrence or new lesions by clinical and imaging examinations. The absence of evidence of recurrence or a second primary cancer at the indicated time points and subsequent early follow-up was considered when interpreting the negative 18F-FDG PET/CT result at that time point.
Continuous variables were expressed as the median and range, and categorical variables were expressed as numbers and percentages. The sensitivity, specificity, accuracy, and predictive values of the imaging methods for assessing recurrence and secondary primary cancer were evaluated. Before referring to interpretation of 18F-FDG PET/CT or other imaging, the clinicians recorded their clinical findings including endoscopic and physical examinations at the clinic visits. The diagnostic value of 18F-FDG PET/CT was compared with that of regular clinical examination at the time points of 18F-FDG PET/CT scans using the McNemar test. Estimates of survival functions for overall and disease-free survivals were generated by the Kaplan–Meier method and compared by the log-rank test. A two-tailed P-value of <0.05 was considered statistically significant. All statistical analyses were performed using SPSS software version 21.0 (IBM, Armonk, NY, USA).
Results
Patient characteristics and follow-up summary
A total of 143 patients, 113 men and 30 women with a median age of 63 years (range, 20−83 years), were included in the study. The characteristics of the patients are shown in Table 1. The primary tumours were most frequently detected in the larynx (27%) and the oral cavity (24%). At the time of initial staging, 41% of the patients were T3–4, 37% were N1–3, and 62% were overall TNM stage III or IV.
Follow-up data of patients after curative treatment are summarised in Table 2. Local or regional recurrence or distant metastases developed in 47 (33%) patients and second primary cancers occurred in 13 (9%) patients at a median of 12 months (range, 2–30 months). Considering the time points of post-treatment 18F-FDG PET/CT scans, recurrences occurred in 27 patients at ∼3–6 months (range, 2–9 months) and in 27 patients at 12 months (range, 9–20 months), of whom 12 had recurrences at both time points. Of 15 patients with late recurrences alone, 13 had negative PET/CT results at 3–6 months and 2 received no early PET/CT scans. All surviving patients were followed-up to a median of 30 months with a range of 18 to 45 months. At the last follow-up, 18 (13%) patients had died of HNSCC, 3 (2%) had died of other causes, 20 (14%) were alive with disease, and 102 (71%) had no evidence of disease. The 3-year overall and disease-free survival rates of all patients were 81% and 63%, respectively.
Value of 18F-FDG PET/CT for post-treatment surveillance
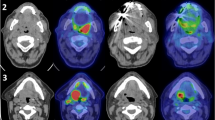
The 3–6-month 18F-FDG PET/CT was performed in 133 patients at a median of 5 months (range, 2–9 months), and the 12-month 18F-FDG PET/CT was performed in 119 patients at a median of 13 months (range, 9–20 months) after curative therapy. Of the 143 study patients, 109 had the 18F-FDG PET/CT scans at both time points. The diagnostic accuracy of 18F-FDG PET/CT for the detection of post-treatment recurrence or second primary cancers is shown in Table 3. The sensitivity of the 3–6-month 18F-FDG PET/CT for detecting local recurrence, regional recurrence, and distant metastasis was 100%, 92%, and 100%, respectively, and the specificity was 97%, 95%, and 99%, respectively. The sensitivity of the 12-month 18F-FDG PET/CT for detecting local recurrence, regional recurrence, and distant metastasis was 83%, 100%, and 85%, respectively, and the specificity was 95%, 95%, and 100%, respectively. The 3–6- and 12-month 18F-FDG PET/CT scans detected post-treatment recurrence in most cases despite the absence of clinical suspicion (Figure 1). Abnormal focal 18F-FDG uptake read as false positive was reported in 10 patients on the 3–6-month PET/CT and in 5 patients on the 12-month PET/CT. However, the sensitivity of 18F-FDG PET/CT for the identification of a second primary cancer was 29% and 80% at 3–6 and 12 months, respectively. Second primary cancers detected by 3–6- and 12-month 18F-FDG PET/CT and later confirmed were 1 out of 4 (sensitivity, 25%) in the oesophagus, 1 out of 3 (33%) in the stomach, 1 out of 2 (50%) in the lung, 1 out of 1 (100%) in the thyroid gland, 1 out of 1 (100%) in the prostate gland, and 1 out of 1 (100%) in the nasopharynx.
The 18F-FDG PET/CT images showing true-positive foci (arrows) of post-treatment recurrence. Whole-body 18F-FDG PET/CT scans correctly detected lymph node recurrence on the right neck at 3 months (A–D) and hepatic metastasis at 10 months (E–G) after chemoradiotherapy for oropharyngeal carcinoma. (A, B, E, and F) The 18F-FDG PET images; (C) axial CT image; (D and G) fused 18F-FDG PET/CT images.
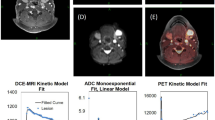
Impact of 18F-FDG PET/CT on patient management
The diagnostic performance of 18F-FDG PET/CT for the detection of post-treatment recurrence was compared with that of regular clinical follow-up at patient level and the results are shown in Table 4. The sensitivities of 3–6- and 12-month 18F-FDG PET/CT scans at patient level were 96% and 93%, respectively, and those of regular follow-up were 11% and 19%, respectively, showing statistically significant differences (P<0.001). In patients with no clinical suspicion, recurrence was detected by PET/CT at 3–6 months in 23 (95%) patients and at 12 months in 20 (91%) patients. The detection of recurrence by follow-up 18F-FDG PET/CT contributed to patient management for salvage or palliative treatment. However, patients with a positive detection of recurrence by 18F-FDG PET/CT had overall poorer survival outcome than those with negative results (P<0.001; Figure 2). A positive PET/CT interpretation was associated with an eight-fold increase in the relative risk of overall death (8.60, 95% CI 3.32–22.29).
Discussion
The National Comprehensive Cancer Network (NCCN, 2013) guidelines for follow-up care in head and neck cancer patients recommend post-treatment baseline imaging within 6 months after initial treatment for cancers of the oropharynx, hypopharynx, larynx, and nasopharynx in patients with T3–4 or N2–3 disease only, and further re-imaging is not recommended except in clinically suspected patients. However, post-treatment recurrence may occur in patients negative for disease on clinical follow-up (Salaun et al, 2007). Tissue fibrosis, oedema, necrosis, and anatomic changes after RT and/or surgery can interfere with early detection of residual viable tumour or recurrence by the usual sequential physical and endoscopic examinations of the head and neck (Lell et al, 2000; Zundel et al, 2011). In the present study, 18F-FDG PET/CT was significantly more effective at detecting recurrence than clinical follow-up examination, suggesting that the inclusion of 18F-FDG PET/CT as a sequential diagnostic tool is beneficial regardless of the presence or absence of clinical findings suggestive of recurrence.
The results of our study indicated that 18F-FDG PET/CT is a useful tool for the detection of recurrent tumours at ∼3–6 and 12 months after curative treatment. However, the recommended intervals and frequencies of post-treatment 18F-FDG PET/CT are controversial. The 18F-FDG PET or PET/CT is highly effective for distinguishing persistent disease from nonviable tumours or treatment sequelae, with potential to guide therapeutic decision making, but the timing of post-treatment 18F-FDG PET or PET/CT has a significant impact on its diagnostic accuracy (Isles et al, 2008; Ong et al, 2008; Gupta et al, 2011). Because of its limited accuracy within 2 months after treatment, 18F-FDG PET/CT at 3 months after treatment is now accepted as a standard method of post-treatment surveillance at many institutions (Isles et al, 2008; Gupta et al, 2011). Furthermore, in a recent retrospective study that included 388 HNSCC patients with definitive chemoradiation therapy, 45% of the observed asymptomatic recurrences were detected during the first 6 months of surveillance (Beswick et al, 2012). A prospective study recommended one systematic 18F-FDG PET/CT at 3–6 months after treatment as the optimal timing (Krabbe et al, 2009), which was confirmed by our data showing the sensitivity of a 3–6-month 18F-FDG PET/CT scan for the detection of early recurrence.
Moreover, further re-imaging with 18F-FDG PET/CT may be necessary to properly detect later recurrence. In this regard, few systematic studies have been conducted to assess the use of repeated routine post-treatment 18F-FDG PET/CT scans. The results of a prospective study suggested that 18F-FDG PET/CT scanning at 12 months improves the detection of HNSCC recurrence with 90% overall accuracy in patients with clinically unsuspected disease (Abgral et al, 2009). However, retrospective studies showed that patients with negative results on 3–6-month imaging had limited benefit from subsequent 18F-FDG PET/CT surveillance (Périé et al, 2007; Ho et al, 2013). In this patient cohort, considerable numbers of the recurrent patients had recurrences later than 9 months. This may be a discrepancy with other published data showing that negative 3–6-month PET/CT scans were a prognostic predictor (Ho et al, 2013). The results of our study showed that 18F-FDG PET/CT at 12 months detected recurrence in 25 of 27 patients (93%), supporting the use of 18F-FDG PET/CT at 12 months after treatment for the accurate detection of recurrence that may occur >9 months after treatment. In the present study, systematic 18F-FDG PET/CT scans at 12 months in addition to 3–6 months after treatment may also significantly impact salvage treatment planning. Our results showed that 18F-FDG FDG PET is a highly sensitive method for the detection of recurrence of HNSCC, thus providing important prognostic information for survival outcomes, as a positive PET interpretation was associated with an eight-fold increase in the relative risk of patient death.
Systemic reviews have been conducted on the role of 18F-FDG PET or PET/CT in the follow-up of head and neck cancer patients. A meta-analysis of 51 trials involving 2335 patients showed that the pooled sensitivity and specificity of post-treatment 18F-FDG PET or PET/CT for the primary site were 80% and 88%, respectively, and those for the neck were 73% and 88%, respectively (Gupta et al, 2011). In 27 of 1871 identified studies evaluating 18F-FDG PET or PET/CT for the detection of residual or recurrent HNSCC after RT or CRT, the pooled sensitivity and specificity of 18F-FDG PET or PET/CT were 94% and 82%, respectively, whereas those of CT were lower (67% and 78%, respectively) (Isles et al, 2008). The positive predictive value (PPV) and negative predictive value (NPV) of 18F-FDG PET or PET/CT were 75% and 95%, respectively. Several studies analysing the diagnostic performance of post-treatment 18F-FDG PET or PET/CT for the detection of HNSCC recurrence report sensitivities of 89–100%, specificities of 64–100%, PPVs of 64–100%, NPVs of 92–100%, and overall accuracy of 88–91% (Wong et al, 2002; Kitagawa et al, 2003; Salaun et al, 2007; Abgral et al, 2009; Kao et al, 2009; Krabbe et al, 2009; Kim et al, 2011; Zundel et al, 2011; Ho et al, 2013). The diagnostic value of 18F-FDG PET/CT determined in the present study was comparable to those of the previous reports. The NPV of 18F-FDG PET remained exceptionally high (99%), whereas its PPV was somewhat suboptimal (72%). This implies that a negative post-treatment scan is highly suggestive of the absence of recurrence. The low sensitivity and PPV of clinical examination may result from the potential difficulty in detection of distant metastases or early small-volume recurrences because of postsurgical and radiation-induced changes in both primary sites and the neck (Lell et al, 2000).
In the present study, we examined the role of 18F-FDG PET/CT in the detection of second primary cancers after treatment. The 3–6- and 12-month 18F-FDG PET/CT scans correctly identified 6 of 12 (50%) second primary cancers. The relatively low sensitivity of 18F-FDG PET/CT for the detection of post-treatment second primary cancers could be attributed to its low detection rate (29%) in the oesophagus or the stomach. The ability of 18F-FDG PET or PET/CT to detect superficial or early-stage second primary cancers in the upper gastrointestinal tract is limited (Little et al, 2007; Shoda et al, 2007). These can be better diagnosed using systematic endoscopic screening (Petit et al, 2001; Takenaka et al, 2009). However, because the anatomic site and incidence of second primary cancers may differ among different ethnic groups, the follow-up protocols for detecting second primary cancers should be examined in further studies. In addition, because second primary cancers can arise after initial presentation of index HNSCC at an annual rate of 2.8% (Jovanovic et al, 1994), the efficacy and timing of the diagnostic methods for detecting second primary cancers need to be further examined.
Our study has revealed the potential role of post-treatment 18F-FDG PET/CT surveillance for early detection of recurrences. However, there is no clear evidence of any survival benefit of treating as asymptomatic recurrence compared with symptom-directed recurrences. This may be from a lack of prospective studies on the issues and small number of inclusion patients. This needs to be elucidated by further prospective studies with large HNSCC population. Furthermore, the cost effectiveness of 18F-FDG PET/CT for routine post-treatment surveillance vs for clinically suspected recurrence should be determined. In addition, the 3–6- and 12-month 18F-FDG PET/CT showed a relatively wide range of 2–9 and 9–20 months, respectively. This might result from the retrospective nature of our study despite a systematic follow-up protocol established in our institution consisting of whole-body 18F-FDG PET/CT at ∼3–6 and 12–18 months after curative therapy.
In conclusion, 18F-FDG PET/CT showed high sensitivity and NPV for the detection of recurrence after curative treatment in HNSCC patients. Our data indicated that 18F-FDG PET/CT surveillance is beneficial for the detection of recurrence that may be missed by regular physical and endoscopic examinations of the head and neck area. In addition, follow-up 18F-FDG PET is important to provide clinicians with information on patient survival. The results of our study indicate that systematic 18F-FDG PET/CT scanning at 3–6 months and at 12 months after treatment is beneficial for the early detection of recurrence and may facilitate proper salvage intervention in these patients. Although this study shows a benefit to 18F-FDG PET/CT surveillance, further studies are needed to optimise frequency and timing.
Change history
10 December 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abgral R, Querellou S, Potard G, Le Roux PY, Le Duc-Pennec A, Marianovski R, Pradier O, Bizais Y, Kraeber-Bodéré F, Salaun PY (2009) Does 18F-FDG PET/CT improve the detection of posttreatment recurrence of head and neck squamous cell carcinoma in patients negative for disease on clinical follow-up? J Nucl Med 50 (1): 24–29.
Ang KK, Trotti A, Brown BW, Garden AS, Foote RL, Morrison WH, Geara FB, Klotch DW, Goepfert H, Peters LJ (2001) Randomized trial addressing risk features and time factors of surgery plus radiotherapy in advanced head-and-neck cancer. Int J Radiat Oncol Biol Phys 51 (3): 571–578.
Argiris A, Karamouzis MV, Raben D, Ferris RL (2008) Head and neck cancer. Lancet 371 (9625): 1695–1709.
Beswick DM, Gooding WE, Johnson JT (2012) Temporal patterns of head and neck squamous cell carcinoma recurrence with positron-emission tomography/computed tomography monitoring. Laryngoscope 122 (7): 1512–1517.
Edge SB, Byrd DR, Compton CC, Fritz AG, Green FL, Trotti A eds. (2010) AJCC Cancer Staging Manual 7th edn pp 21–78. Springer-Verlag: New York.
Gupta T, Master Z, Kannan S, Agarwal JP, Ghsoh-Laskar S, Rangarajan V, Murthy V, Budrukkar A (2011) Diagnostic performance of post-treatment FDG PET or FDG PET/CT imaging in head and neck cancer: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging 38 (11): 2083–2095.
Haddad RI, Shin DM (2008) Recent advances in head and neck cancer. N Engl J Med 359 (11): 1143–1154.
Ho AS, Tsao GJ, Chen FW, Shen T, Kaplan MJ, Colevas AD, Fischbein NJ, Quon A, Le QT, Pinto HA, Fee WE Jr, Sunwoo JB, Sirjani D, Hara W, Yao M (2013) Impact of positron emission tomography/computed tomography surveillance at 12 and 24 months for detecting head and neck cancer recurrence. Cancer 119 (7): 1349–1356.
Isles MG, McConkey C, Mehanna HM (2008) A systematic review and meta-analysis of the role of positron emission tomography in the follow up of head and neck squamous cell carcinoma following radiotherapy or chemoradiotherapy. Clin Otolaryngol 33 (3): 210–222.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61 (2): 69–90.
Jovanovic A, van der Tol IG, Kostense PJ, Schulten EA, de Vries N, Snow GB, van der Waal I (1994) Second respiratory and upper digestive tract cancer following oral squamous cell carcinoma. Eur J Cancer B Oral Oncol 30B (4): 225–229.
Kao J, Vu HL, Genden EM, Mocherla B, Park EE, Packer S, Som PM, Kostakoglu L (2009) The diagnostic and prognostic utility of positron emission tomography/computed tomography-based follow-up after radiotherapy for head and neck cancer. Cancer 115 (19): 4586–4594.
Kim SY, Kim JS, Yi JS, Lee JH, Choi SH, Nam SY, Cho KJ, Lee SW, Kim SB, Roh JL (2011) Evaluation of 18F-FDG PET/CT and CT/MRI with histopathologic correlation in patients undergoing salvage surgery for head and neck squamous cell carcinoma. Ann Surg Oncol 18 (9): 2579–2584.
Kitagawa Y, Nishizawa S, Sano K, Ogasawara T, Nakamura M, Sadato N, Yoshida M, Yonekura Y (2003) Prospective comparison of 18F-FDG PET with conventional imaging modalities (MRI, CT, and 67Ga scintigraphy) in assessment of combined intraarterial chemotherapy and radiotherapy for head and neck carcinoma. J Nucl Med 44 (2): 198–206.
Krabbe CA, Pruim J, Dijkstra PU, Balink H, van der Laan BF, de Visscher JG, Roodenburg JL (2009) 18F-FDG PET as a routine posttreatment surveillance tool in oral and oropharyngeal squamous cell carcinoma: a prospective study. J Nucl Med 50 (12): 1940–1947.
Leemans CR, Tiwari R, Nauta JJP, van der Waal DDS, Snow GB (1994) Recurrence at the primary site in head and neck cancer and the significance of neck lymph node metastases as a prognostic factor. Cancer 73 (1): 187–190.
Lell M, Baum U, Greess H, Nömayr A, Nkenke E, Koester M, Lenz M, Bautz W (2000) Head and neck tumors: imaging recurrent tumor and post-therapeutic changes with CT and MRI. Eur J Radiol 33 (3): 239–247.
Little SG, Rice TW, Bybel B, Mason DP, Murthy SC, Falk GW, Rybicki LA, Blackstone EH (2007) Is FDG-PET indicated for superficial esophageal cancer? Eur J Cardiothorac Surg 31 (5): 791–796.
NCCN (2013) NCCN clinical practice guidelines in oncology: head and neck cancers. Version 1.2012. National Comprehensive Cancer Network Website http://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf. Accessed 14 July 2013.
Ong SC, Schöder H, Lee NY, Patel SG, Carlson D, Fury M, Pfister DG, Shah JP, Larson SM, Kraus DH (2008) Clinical utility of 18F-FDG PET/CT in assessing the neck after concurrent chemoradiotherapy for locoregional advanced head and neck cancer. J Nucl Med 49 (4): 532–540.
Pai SI, Westra WH (2009) Molecular pathology of head and neck cancer: implications for diagnosis, prognosis, and treatment. Annu Rev Pathol 4: 49–70.
Petit T, Georges C, Jung GM, Borel C, Bronner G, Flesch H, Massard G, Velten M, Haegele P, Schraub S (2001) Systematic esophageal endoscopy screening in patients previously treated for head and neck squamous-cell carcinoma. Ann Oncol 12 (5): 643–646.
Périé S, Hugentobler A, Susini B, Balogova S, Grahek D, Kerrou K, Montravers F, Chater PE, Guily JL, Talbot JN (2007) Impact of FDG-PET to detect recurrence of head and neck squamous cell carcinoma. Otolaryngol Head Neck Surg 137 (4): 647–653.
Salaun PY, Abgral R, Querellou S, Couturier O, Valette G, Bizais Y, Kraeber-Bodéré F (2007) Does 18fluoro-fluorodeoxyglucose positron emission tomography improve recurrence detection in patients treated for head and neck squamous cell carcinoma with negative clinical follow-up? Head Neck 29 (12): 1115–1120.
Shoda H, Kakugawa Y, Saito D, Kozu T, Terauchi T, Daisaki H, Hamashima C, Muramatsu Y, Moriyama N, Saito H (2007) Evaluation of 18F-2-deoxy-2-fluoro-glucose positron emission tomography for gastric cancer screening in asymptomatic individuals undergoing endoscopy. Br J Cancer 97 (11): 1493–1498.
Takenaka R, Kawahara Y, Okada H, Hori K, Inoue M, Kawano S, Tanioka D, Tsuzuki T, Uemura M, Ohara N, Tominaga S, Onoda T, Yamamoto K (2009) Narrow-band imaging provides reliable screening for esophageal malignancy in patients with head and neck cancers. Am J Gastroenterol 104 (12): 2942–2948.
Wong LY, Wei WI, Lam LK, Yuen AP (2003) Salvage of recurrent head and neck squamous cell carcinoma after primary curative surgery. Head Neck 25 (11): 953–959.
Wong RJ, Lin DT, Schöder H, Patel SG, Gonen M, Wolden S, Pfister JP, Shah JP, Larson SM, Kraus DH (2002) Diagnostic and prognostic value of [(18)F]fluorodeoxyglucose positron emission tomography for recurrent head and neck squamous cell carcinoma. J Clin Oncol 20 (20): 4199–4208.
Xu GZ, Guan DJ, He ZY (2011) (18)FDG-PET/CT for detecting distant metastases and second primary cancers in patients with head and neck cancer. A meta-analysis. Oral Oncol 47 (7): 560–565.
Zundel MT, Michel MA, Schultz CJ, Maheshwari M, Wong SJ, Campbell BH, Massey BL, Blumin J, Wilson JF, Wang D (2011) Comparison of physical examination and fluorodeoxyglucose positron emission tomography/computed tomography 4-6 months after radiotherapy to assess residual head-and-neck cancer. Int J Radiat Oncol Biol Phys 81 (5): e825–e832.
Acknowledgements
This study was supported by Grants (No. 2013-417) from the Asan Institute for Life Science and Basic Science Research Program through the National Research Foundation (NRF) of Korea funded by the Ministry of Education, Science and Technology (Grant No. 2012R1A1A2002039), Seoul, Korea (to J-L Roh).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Kim, J., Roh, JL., Kim, J. et al. 18F-FDG PET/CT surveillance at 3–6 and 12 months for detection of recurrence and second primary cancer in patients with head and neck squamous cell carcinoma. Br J Cancer 109, 2973–2979 (2013). https://doi.org/10.1038/bjc.2013.668
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.668
Keywords
This article is cited by
-
Post-treatment surveillance imaging in head and neck cancer: a systematic review
Insights into Imaging (2024)
-
Narrow Band Imaging Technology: Role in the Detection of Recurrent Laryngeal and Hypopharyngeal Cancers Post-radiotherapy
Indian Journal of Otolaryngology and Head & Neck Surgery (2023)
-
FDG-PET/CT in the surveillance of head and neck cancer following radiotherapy
European Archives of Oto-Rhino-Laryngology (2020)
-
Clinical impact of PET/CT imaging after adjuvant therapy in patients with oral cavity squamous cell carcinoma
European Journal of Nuclear Medicine and Molecular Imaging (2017)
-
Predictive factors for long-term survival in head and neck squamous cell carcinoma patients with distant metastasis after initial definitive treatment
Journal of Cancer Research and Clinical Oncology (2016)