Abstract
Background:
In the current study, mammography adherence of women who had experienced a false-positive referral is evaluated, with emphasis on the probability of receiving surveillance mammography outside the national screening programme.
Methods:
We included 424 703 consecutive screens and collected imaging, biopsy and surgery reports of 3463 women who experienced a false-positive referral. Adherence to screening, both in and outside the screening programme, was evaluated.
Results:
Two years after the false-positive referral, overall screening adherence was 94.6%, with 64.7% of women returning to the national screening programme, compared with 94.9% of women re-attending the screening programme after a negative screen (P<0.0001). Four years after the false-positive screen, the overall adherence had decreased to 85.2% (P<0.0001) with a similar proportion of the women re-attending the screening programme (64.4%) and a lower proportion (20.8%) having clinical surveillance mammography. Women who had experienced a false-positive screen at their first screening round were less likely to adhere to mammography than women with an abnormal finding at one of the following screening rounds (92.4% vs 95.5%, P<0.0001).
Conclusion:
Overall screening adherence after previous false-positive referral was comparable to the re-attendance rate of women with a negative screen at 2-year follow-up. Overall adherence decreased 4 years after previous false-positive referral from 94.6% to 85.2%, with a relatively high estimate of women who continue with clinical surveillance mammography (20.8%). Women with false-positive screens should be made aware of the importance to re-attend future screening rounds, as a way to improve the effectiveness of the screening programme.
Similar content being viewed by others
Main
Many Western countries have implemented screening mammography programmes with the aim to reduce breast cancer mortality. However, the extent of the mortality reduction through screening alone remains subject to discussion worldwide (Independent UK panel on breast cancer screening, 2012). Moreover, the unintended negative consequences of screening mammography, including overdiagnosis and subsequent overtreatment (Jorgensen and Gotzsche, 2009) and false-positive referrals (Brewer et al, 2007; Bond et al, 2013) are of particular concern in the debate concerning the effectiveness of screening mammography. Women with false-positive screening results undergo additional imaging and biopsy procedures and many of them experience anxiety and distress (Aro et al, 2000; Gotzsche and Nielsen, 2011; Van der Steeg et al, 2011), particularly in the first month post-screening. At 12 months, concerns that seem to prevail are intrusive thinking and a higher perceived risk of breast cancer (Aro et al, 2000). In some women, breast cancer-specific distress is reported to last for up to 3 years after a false-positive screen (Bond et al, 2013). Whether or not receiving a false-positive mammogram undermines attendance at subsequent scheduled screening mammography is controversial. A meta-analysis of 12 studies reported no significant relationship between false-positive screening mammograms and return for routine screening among European women. On the other hand, a decreased likelihood of re-attendance among Canadian women and even an increased re-attendance among women who experienced a false-positive mammogram in the United States was demonstrated (Brewer et al, 2007).
Because the effectiveness of screening is closely related to adequate adherence among the target population, it is important to know whether women who experience a false-positive referral do return for routine testing. To our knowledge, screening behaviour after false-positive referral has only been evaluated with regard to re-attendance in the screening programme. In the current study, we evaluated whether women who did not re-attend the national screening programme after a false-positive referral, underwent surveillance mammography outside the screening programme, or refrained from repeated mammography at all.
Materials and methods
Study population
We used the information of a consecutive series of 91 570 women who underwent screening mammography in a southern breast cancer screening region of the Netherlands (BOZ, Bevolkings Onderzoek Zuid) between 1 January 1995 and 1 January 2010. Biennial screening was started in this region in 1995. Initially, it included women aged 50–69 years, but from 1998 onwards women aged 70–75 years were invited as well. The overall attendance rate was around 84% and varied a little over time (Annual report BOZ (bevolkings Onderzoek Zuid), 2009).
Before screening examination women were asked whether their screening and follow-up data can be used for evaluation purposes. Three women refused this and they were excluded from the study. Ethical approval by our local institutional review board was not required for this study, according to the Dutch Central Committee on Research involving Human Subjects (CCMO).
Screening procedure and referral
Screening mammography in the BOZ region was performed at one of two specialised screening units (one fixed and one mobile unit). The two analogue (screen film) units were replaced by digital screening units in May 2009. Details of the nation-wide breast cancer screening programme in the Netherlands have been described in detail previously (Otto et al, 2003). All examinations were performed by specialised screening mammography radiographers. At analogue screening, two-view mammography (medio-lateral-oblique and cranio-caudal view) of each breast was performed at the first screening round. At subsequent analogue screening rounds, one view mammography (medio-lateral-oblique) was obtained routinely and additional views (cranio-caudal) were obtained in 45% of cases. Indications for this two-view mammography included any changes in mammographic findings at screening, complicated judgement because of dense fibroglandular tissue, a more than 2-year interval since the previous screen and previous breast surgery. Digital screening mammography always consisted of two-view mammography.
All screens were independently double read by 16 certified screening radiologists and each radiologists evaluated at least 3000 screening mammograms per year. Mammograms of previous screening round were always available for comparison. Women with normal, benign or nonspecific findings (Maes et al, 1997) at screening mammography were not referred. For each referred woman, the screening radiologists classified the abnormal mammographic findings according to one of five categories: (1) suspicious high density (spiculated density or density with irregular borders); (2) suspicious microcalcifications (pleiomorphic, branching or amorphous/indistinct microcalcifications; (3) high density in combination with microcalcifications; (4) architectural distortion or (5) asymmetry. Women with suspicious or malignant findings at screening mammography were referred to their general practitioner and subsequently to a regional hospital of their choice for further diagnostic assessment. A total of 16 hospitals were involved in the work-up of referred women. This work-up consisted of physical examination by a surgical oncologist and additional mammographic views. Breast ultrasonography, magnetic resonance mammography and/or biopsy were performed at the radiologist’s discretion.
Follow-up procedure and re-attendance after a false-positive referral
One radiologist (LD) yearly visited the regional hospitals involved in the work-up of referred women, to collect data on any imaging procedures, breast biopsy outcomes and breast surgery procedures of each referred woman. For women diagnosed with breast cancer after referral, diagnostic and therapeutic data were collected from the time of referral through the moment of final therapy (e.g., breast conserving therapy, mastectomy or palliative treatment). For all women not diagnosed with breast cancer (i.e., those with a false-positive referral), the radiologist collected outcome data for 2 years (until the next scheduled biennial screening examination) at the hospitals the women had been referred to. Furthermore, for those women who did not re-attend the screening programme after a false-positive screen, the radiologist checked each year if they had undergone any breast imaging procedure, breast biopsy or breast surgery at one of the regional hospitals. This information enabled us to determine whether or not these women had undergone clinical mammographic surveillance outside the screening programme. Moreover, the radiologist obtained information on the reasons for not being under clinical mammographic surveillance outside the screening programme, such as having undergone preventive mastectomy or suffering from serious other illness. Information was also retrieved on how long a woman underwent clinical follow-up after a false-positive referral. Linkage of our database to the national screening database and the regional register of Death (Gemeentelijke Basisadministratie Persoonsgegevens) enabled us to identify the referred women who had died and to identify the referred women who had attended the screening programme in another screening region (Duijm et al, 2004). Strategies used to identify interval cancers have been described previously (Duijm et al, 2007).
Follow-up and re-attendance after a negative screen
Data on women who had received a negative screen (i.e., no referral) during the study period were collected from the BOZ screening database. The women who were not eligible for re-screening were identified (i.e., women who had died, who had moved to another screening region, as well as women who informed the screening organisation that they did not appreciate a re-invitation for screening). The screening adherence at the subsequent screening round was determined.
In the current study, surveillance mammography is defined as a mammogram performed in the clinical setting, in one of the adherent hospitals in the BOZ region, in the 2-year and 4-year period after actual referral in women who experienced a false-positive screen. This mammogram could have been performed on the woman’s request, or at the surgeon’s or radiologist’s discretion.
We defined re-attendance in the screening programme as participation at the next routine screening round following a screening invitation. For the current study, we used a follow-up period of at least 2 years (until the next biennial screening) for women screened between April 2008 and April 2010 and of at least 4 years for women screened between January 1995 and April 2008 (until the second round after the index mammography).
To determine which women were no longer eligible for screening after a previous screen, we identified the ones who had died from other causes than breast cancer, the women who had been diagnosed with an interval cancer and those who had moved to another screening region or had turned 76 years before the next screening round. These women constitute the ‘non-target’ group. An interval cancer was defined as a breast cancer diagnosed before the next (biennial) screening round after a previous negative screen.
Statistical analysis
Descriptive statistics were performed using Statistical Package for Social Sciences 17.0 (SPSS, Chicago, IL, USA). The χ2 test was used to test the differences for a statistical significance. The significance level was set at P=0.05. The main outcome measure was the adherence to screening, which was defined as the proportion of women returning to the screening programme or having surveillance mammography 2 and 4 years following a false-positive screening result. Differences in the proportion of women re-attending the screening programme were tested between women who experienced a false-positive referral and those with a negative screen. The proportion of women re-attending the screening programme was also studied over time, looking at three time intervals (1995–1999, 2000–2004 and 2005–2009), and according to screening history (first screening round versus subsequent screening rounds).
Results
Overall screening results
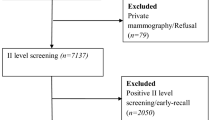
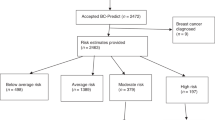
A total of 424 703 screens (406 856 analogue and 17 847 digital screens) were obtained in 91 570 women between 1 January 1995 and 1 January 2010. Of these, 85 099 were initial screens and 339 604 were subsequent screens. The screening programme in our region started in 1995. Several women had already been screened in another region before this date and were then added to our screening region, explaining why the number of women with a first screen is lower than the number of women screened in the study period 1995–2009. In the whole study period, 512 262 invitations were sent and the overall attendance, therefore, was 82.9%. The mean age of all women screened was 62.5 years. Altogether, 5529 women (5676 screens) were referred for further diagnostic testing (1528 referrals at initial screen and 4148 referrals at subsequent screens). The overall referral rate was 1.3%. Altogether, 2204 of the referred women were diagnosed with breast cancer (including 372 ductal carcinomas in situ), yielding an overall detection rate of 5.2 per 1000 women screened and a positive predictive value of referral of 38.8%. A total of 3463 women experienced a false-positive referral resulting in an overall false-positive referral rate of 8.2 per 1000 women screened. The follow-up of the remaining nine referred women was unknown and these women were excluded from analysis (Figure 1).
In addition to the 2204 women diagnosed with a screen detected cancer, 806 women were diagnosed with an interval cancer (including 33 ductal carcinomas in situ), resulting in a 73.2% (2204 out of 3010) sensitivity and 99.2% (418 221 out of 421 693) specificity of breast cancer screening (based on 418 221 true-negative screens and 3472 false-positive screens, including 9 referrals with unknown follow-up). Of the 3463 false-positive referrals, diagnostic work-up was limited to additional breast imaging in 2117 (61.1%) women, whereas 1035 (29.9%) also underwent percutaneous biopsy (fine needle aspiration cytology and/or core needle biopsy). Excisional biopsy (with or without preceding percutaneous biopsy) had been performed in 305 (8.8%) women who experienced a false-positive screen. Six women refused any kind of work-up and were not referred to a hospital for further assessment.
Re-attendance 2 years after a negative screening result
The screening radiologists found no indication for referral in 419 027 screens. A total of 20 890 women were not eligible for re-attendance (non-target group, Table 1A). There were 20 377 women who did not re-attend the subsequent screening round (non-responders). Therefore, the re-attendance rate after a negative screen was 94.9% (377 760 out of 398 137; Figure 1; Table 1A).
Re-attendance 2 years after a false-positive referral
After 2-year follow-up, 3269 women were still eligible for screening mammography. At that time, 194 (5.6%) of the 3463 women who had experienced a false-positive referral were no longer available for screening (non-target group; Table 1A). After 2 years, 2116 (64.7%) of the 3269 women still eligible for screening returned for their screening mammogram, which was significantly lower than for the women with a true-negative screen (94.9%, P<0.0001). A group of 976 women (29.9%) had undergone surveillance mammography in the clinical setting. Of all women in the target population, 94.6% (3092 out of 3269) therefore underwent mammography after a previous false-positive referral, either being a scheduled screening examination or a clinical surveillance mammogram outside the screening programme. A total of 177 (5.4%) women had no mammography performed in or outside the screening programme within 2 years after their false-positive referral (Figure 1; Table 1A and B).
Re-attendance after 4-year follow-up
The 4-year follow-up could be determined for 2575 of the 3463 women who experienced a false-positive referral in the study period. For the other 888 women screened after March 2008, 4-year follow-up was not reached yet. A total of 303 (11.7%) women were not eligible for re-screening (non-target group; Table 1A). Four years after a false-positive referral, 64.4% (1464 out of 2272) of the women in the target population had re-attended the screening programme. A total of 472 women (20.8%) had a surveillance mammogram performed in the clinical setting. Therefore, after 4 years 85.2% (1936 out of 2272) of the women underwent mammography after a previous false-positive screen in or outside the screening programme, which was significantly lower compared with the adherence of 95.6% after 2 years (P<0.0001; Table 1B). A total of 336 women (14.8%) did not attend screening 4 years after their false-positive referral, although 207 (61.6%) of these women did participate in the screening programme at 2-year follow-up (Figure 1, Table 1A and B).
Re-attendance in time and according to screening history
When comparing the re-attendance rate 2 years after false-positive referral in the national screening programme for three different screening periods (1995–1999, 2000–2004 and 2005–2009), we found a statistically significant increase from 59.8% in 1995–1999 to 67.9% in 2005–2009 (P<0.0001). The proportion of women who underwent clinical surveillance mammography decreased from 33.2% in 2000–2004 to 26.8% in 2005–2009 (P<0.0001; Table 2).
The proportion of women who re-attended after a false-positive referral in their first screening round remained stable over the years (Table 2). Of the 3269 women with a false-positive screen eligible for re-screening, 970 experienced their false-positive screen at initial screening and 2299 women at subsequent screening. Women who had experienced a false-positive screen at their first screening round were significantly less likely to return for screening or clinical surveillance mammography than those with a false-positive referral at subsequent screening rounds (92.4% (896 out of 970) vs 95.5% (2196 out of 2299), P<0.0001; Table 1B)
Discussion
To our knowledge, the current population-based study is the first that is able to determine to what extent women, not returning to the screening programme after a previous false-positive screen, were undergoing surveillance mammography outside the screening programme. The study gives a virtually complete picture of screening behaviour after false-positive referral in a southern screening region of the Netherlands, in which we were able to determine almost all causes related to nonattendance at subsequent screening. We found that 2 years after a previous false-positive screen 64.7% of women had re-attended the screening programme. This percentage was significantly lower compared to women with a negative screen (94.9%) in the same period. Almost one-third (29.9%) of women with a previous false-positive screen had a clinical surveillance mammography performed, resulting in an overall mammography adherence of 94.6%, which is comparable to the adherence among women with a true-negative screen. After 4 years, we found a significant decrease in the overall adherence to 85.2% for women who experienced a false-positive referral. The compliance to the screening programme, in women who experienced an abnormal mammogram, increased significantly in time and overall adherence in women with an abnormal initial screen was significantly lower compared with women who received a subsequent false-positive screen.
Published estimates of re-attendance after experiencing a false-positive screen range between 27 and 52% in Canada (Johnson et al, 1996; Chiarelli et al, 2003), with a lower likelihood of re-attendance in this group as compared with the women without a previous false-positive screening result. In the United States, the reported re-attendance rates vary between 63 and 87% (Lipkus et al, 2000; Pinckney et al, 2003), but with a higher re-attendance among those with a false-positive exam. Estimates of re-attendance in European studies range between 71 and 95%, two of which have reported comparable re-attendance between women with a false-positive screen or negative screen (O’Sullivan et al, 2001; Lampic et al, 2003), whereas two others reported lower re-attendance after previous false-positive referral (Roman et al, 2011; Seigneurin et al, 2011). The study by Seigneurin et al (2011) reported estimates of 72.9% vs 80.6%, respectively, for women with and without a previous false-positive screening mammogram, and in the study by Roman et al (2011), the re-attendance rate was 79% for women with and 85% for those without a false-positive screening result.
It is difficult to compare the reported differences in adherence after a false-positive screen, because of the known differences in the organisation of screening procedures between countries worldwide. There is an important difference in the diagnostic work-up after referral between the Netherlands and other countries with regard to intermediate mammograms. In the Netherlands, diagnostic work-up after referral is not an integrated part of the screening programme. Such intermediate follow-up mammograms are performed in the clinical setting at the radiologist’s discretion.
In our study, the re-attendance rate to the national screening programme was 64.7%, which seems relatively low compared with the rates reported in other European countries. However, we now know that a substantial part of the Dutch women continues to undergo a surveillance mammography in the clinical setting, and taking these women into account the overall attendance for mammography after a previous false-positive screen is well above the attendance of 84% for the screening programme as a whole (Annual report BOZ (bevolkings Onderzoek Zuid), 2009) and comparable to women with a negative previous screen. We presume that in our population there is a tendency to keep referred women with a non-malignant diagnosis at additional work-up under clinical surveillance, instead of advising them to return to the screening programme. A major part of our study population was referred before the introduction and gradual implementation of the BI-RADS lexicon (American College of Radiology, 2003) in the Netherlands, but it is likely that the policy was to keep these women for clinical routine follow-up, like a BI-RADS 3 lesion nowadays. After the implementation of the BI-RADS criteria, probably more lesions are pathology proven, as both radiologists and patients prefer a definite diagnosis instead of a wait and see policy. Therefore, more lesions will be classified as BI-RADS 1 or 2 and these women with a normal or benign screening result are directly advised to return to the screening programme. This hypothesis is supported by our data, which showed a significant decrease in the proportion of women undergoing clinical surveillance after false-positive referral after 2004. The recommendation within the Dutch health system is that women should return to the screening programme if the suspicion of breast cancer has been ruled out by additional imaging or invasive procedures (mammographic abnormality classified BI-RADS 1 or 2). For women with a BI-RADS 3 lesion, meaning that the presence of breast cancer is unlikely, a standardised follow-up can be advised (at 6 months, 18 months and 30 months after referral) or the lesion can be biopsied. Those women who end up in follow-up for a BI-RADS 3 lesion are therefore not expected to return in the screening programme 2 years after a false-positive referral. However, at 4 years, these women should have returned in the screening programme. We determined that at 4 years still 20% of women with a previous false-positive referral undergo a clinical surveillance mammography. Unfortunately, for this group of women, we do not know the reasons for not re-attending screening.
The effect of false-positive referral on screening behaviour might also depend on the general attitude of women towards screening and higher participation rates may reflect greater confidence in the benefit of screening. Before 2000, the adherence rate in the Netherlands was around 78%, and between 2000 and 2008 it showed a continuous increase up to 82.0% (84% in the southern breast cancer screening region, BOZ; Annual report BOZ (bevolkings Onderzoek Zuid), 2009; NETB interim report, 2011). This increase is thought to be the result of information campaigns aimed at promoting screening. Parallel to the increase in overall adherence, we found a significant increase over time in re-attendance among women with a previous false-positive referral (form 59.8% to 67.9%). From these observations, we may conclude that the attitude towards breast cancer screening and behavioural intent have evolved in a similar way among women with normal and false-positive mammograms. However, our study showed that even after 2004 more than 20% of women who were referred with a false-positive screening result, continued with clinical surveillance mammography, at least until 4 years after referral. This prolonged clinical surveillance results in additional costs compared with mammography performed within the national screening programme.
Previous research in our screening population showed that a prolonged screening interval within the screening programme is associated with the detection of breast cancer in a more advanced stage (Nederend et al, 2012a). For women with a previous false-positive referral, Von Euler-Chelpin et al (2012) found an excess breast cancer risk, not only in the period 2–4 years after false-positive referral, but even up to 12 years after it. For effective screening, both high re-attendance rates as well as repeated sequential screening with adequate intervals are essential to reduce breast cancer mortality. In order to prevent a possible delay in cancer diagnosis with the risk of more advanced disease, additional information and advice with regard to re-attendance, specifically for women experiencing a false-positive screen, is of great importance. General practitioners as well as surgical oncologists should emphasise the importance of re-attendance to these women.
The false-positive risk has been shown to be higher at first screening (Hofvind et al, 2004). We found that women with an abnormal screening mammogram at their first screening round were somewhat less likely to return for screening (in or outside the screening programme) than women with a false-positive subsequent screen (92.4% vs 95.5%). This in line with previous investigations (McCann et al, 2002; Roman et al, 2012). Moreover, McCann et al (2002) reported that the risk of an interval cancer is increased in these women. It is therefore important to provide women who attend screening for the first time, with the information on the risk of a false-positive screening result and to make them more aware of the significance of their future attendance, to reduce the risk of an interval cancer.
Our study has certain limitations. We were not able to elucidate the reasons for non-attendance of women in the target group at subsequent screening after a false-positive referral. Previous studies have looked at the impact of the type of work-up after false-positive referral on adherence and they nearly all concluded that re-attendance after a false-positive screen is not influenced by the level of diagnostic work-up, whether being additional imaging evaluation only, imaging followed by percutaneous biopsy or surgical excision biopsy after referral (Lampic et al, 2003; Brett et al, 2005). Furthermore, our study is mainly based on the results with screen film mammography. From May 2009, analogue screening was replaced by digital screening units and Nederend et al (2012b) showed that the introduction of digital screening mammography significantly increased the referral rate and cancer detection rate, at the expense of a lower positive-predictive value. We have not yet evaluated the effect of the increase in the number of false-positive screening referrals by digital mammography on the re-attendance rates. No information on patient characteristics, such as family history or use of hormone replacement therapy, was available for the women with a negative screen (i.e., those who were not referred for further diagnostic assessment). For that reason, multivariate analyses to adjust for differences between women who experienced a false-positive screen and women who received a negative screen could not be performed.
In conclusion, we found that overall mammography adherence after a previous false-positive screen was 94.6%, which was comparable to the 94.9% re-attendance rate of women who had not been referred. Almost one-third of women in the first group received a surveillance mammogram at the time they were scheduled for subsequent screening mammography. At 4-year follow-up, we found a significant decrease in overall adherence to 85.2% and a relatively high estimate of women who continue with clinical surveillance mammography (20.8%). Our findings stress the significance to inform women with a previous false-positive screen and those who are invited for their first screening round, of the importance to re-attend to future screening rounds to increase their opportunities of early breast cancer detection and improve the cost-effectiveness of the screening programme.
Change history
15 October 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Annual report BOZ (bevolkings Onderzoek Zuid). (2009) www.bevolkingsonderzoekzuid.nl/page3344/Jaarverslag.
American College of Radiology. (2003) Breast Imaging Reporting and Data System (BI-RADS) 4th edn. American College of Radiology: Reston, VA.
Aro AR, Pilvikki Absetz S, van Elderen TM, van der Ploeg E, van der Kamp LJ (2000) False-positive findings in mammography screening induces short-term distress-breast cancer-specific concern prevails longer. Eur J Cancer 36: 1089–1097.
Bond M, Pavey T, Welch K, Cooper C, Garside R, Dean S, Hyde CJ (2013) Psychological consequences of false-positive screening mammograms in the UK. Evid Based Med 18: 54–61.
Brett J, Bankhead C, Henderson B, Watson E, Austoker J (2005) The psychological impact of mammographic screening. A systematic review. Psychooncology 14: 917–938.
Brewer NT, Salz T, Lilie SE (2007) Systematic review: the long-term effects of false-positive mammograms. Ann Intern Med 146: 502–510.
Chiarelli AM, Moravan V, Halapy E, Majpruz V, Mai V, Tatla RK (2003) False-positive result and reattendance in the Ontario Breast Screening Program. J Med Screen 10: 129–133.
Duijm LE, Groenewoud JH, Jansen FH, Fracheboud J, van Beek M, de Koning HJ (2004) Mammography screening in the Netherlands: delay in the diagnosis of breast cancer screening. Br J Cancer 91: 1795–1799.
Duijm LE, Groenewoud JH, Fracheboud J, de Koning HJ (2007) Additional double reading of screening mammograms by radiologic technologists: Impact on screening performance parameters. J Natl Cancer Inst 99: 1162–1170.
Gotzsche PC, Nielsen M (2011) Screening for breast cancer with mammography (review). Cochrane Database Sys Rev 19 (1): 001877.
Hofvind S, Thorensen S, Tretli S (2004) The cumulative risk of a false-positive recall in the Norwegian Breast cancer screening program. Cancer 101: 1501–1507.
Independent UK Panel on Breast Cancer Screening. (2012) The benefit and harms of breast screening: an independent review. Lancet 17: 1778–1786.
Johnson MM, Hislop TG, Kan L, Coldman AJ, Lai A (1996) Compliance with the screening mammography program of British Colombia: will she return? Can J Public Health 87: 176–180.
Jorgensen KJ, Gotzsche PC (2009) Overdiagnosis in publicly organised mammography screening programmes: systematic review of incidences and trends. Br Med J 9 (339): b2587.
Lampic C, Thurfjell E, Sjoden PO (2003) The influence of a false-positive mammogram on a woman‘s subsequent behaviour for detecting breast cancer. Eur J Cancer 39: 1730–1737.
Lipkus IM, Halabi S, Strigo TS, Rimer BK (2000) The impact of abnormal mammograms on psychosocial outcomes and subsequent screening. Psychooncology 9: 402–410.
Maes RM, Dronkers DJ, Hendriks JH, Thijssen MA, Nab HW (1997) Do non-specific minimal signs in a biennial mammographic breast cancer screening programme need further diagnostic assessment? Br J Radiol 70: 34–38.
McCann J, Stockton D, Godward S (2002) Impact of false-positive mammography on subsequent screening attendance and risk of cancer. Breast Cancer Res 4: R11.
Nederend J, Duijm LE, Voogd AC, Groenewoud JH, Jansen FH, Louwman MW (2012a) Trends in incidence and detection of advanced breast cancer at biennial screening mammography in the Netherlands: a population based study. Breast Cancer Res 14: R10.
Nederend J, Duijm LE, Louwman MW, Groenewoud JH, Donkers-van Rossum AB, Voogd AC (2012b) Impact of transition from analog screening mammography to digital screening mammography on screening outcome in the Netherlands: a population based study. Ann Oncol 23 (12): 3098–3103.
NETB interim report. (2011) Main Results 2008-2009 Breast Cancer Screening Programme in the Netherlands, Department of Public Health, Erasmus University, Rotterdam.
O’Sullivan I, Sutton S, Dixon S, Perry N (2001) False positive results do not have a negative effect on reattendance for subsequent breast screening. J Med Screen 8: 145–148.
Otto SJ, Fracheboud J, Looman CW, Broeders MJ, Boer R, Hendriks JH, Verbeek AL, de Koning H (2003) National evaluation team for breast cancer screening. Initiation of population-base mammography screening in the Dutch municipalities and effect on breast-cancer mortality: a systematic review. Lancet 361: 1411–1417.
Pinckney RG, Geller BM, Burman M, Littenberg B (2003) Effect of false-positive mammograms of return for subsequent screening mammography. Am J Med 114: 120–125.
Roman R, Sala M, De la Vega M, Natal C, Galceran J, Gonzalez-Roman I, Baroja A, Zubizaretta R, Ascunce N, Salas D, Castells X (2011) Effect of false-positives and women’s characteristics on long-term adherence to breast screening. Breast Cancer Res Treat 130: 543–552.
Roman R, Sala M, Salas D, Ascunce N, Zubuzarreta R, Castells X (2012) Effect of protocol-related variables and women’s characteristics on the cumulative false-positive risk in breast cancer screening. Ann Oncol 23: 104–111.
Seigneurin A, Exbrayat C, Labarere J, Delafosse P, Poncet F, Colonna M (2011) Association of diagnostic work-up with subsequent attendance in a breast cancer screening program for false-positive cases. Breast Cancer Res Treat 127: 221–228.
Van der Steeg AFW, Keyzer-Dekker CMG, de Vries J, Roukema JA (2011) Effect of abnormal screening mammogram on quality of life. Br J Surg 98: 537–542.
Von Euler-Chelpin M, Risør LM, Thorsted BL, Vejborg I (2012) Risk of breast cancer after false-positive test results in screening mammography. J Natl Cancer Inst 104: 682–689.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Setz-Pels, W., Duijm, L., Coebergh, J. et al. Re-attendance after false-positive screening mammography: a population-based study in the Netherlands. Br J Cancer 109, 2044–2050 (2013). https://doi.org/10.1038/bjc.2013.573
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.573
Keywords
This article is cited by
-
Subsequent attendance in a breast cancer screening program after a false-positive result in the Local Health Authority of Bologna (Italy)
Scientific Reports (2021)
-
Screening outcome in women repeatedly recalled for the same mammographic abnormality before, during and after the transition from screen-film to full-field digital screening mammography
European Radiology (2017)
-
Trends in incidence and tumour grade in screen-detected ductal carcinoma in situ and invasive breast cancer
Breast Cancer Research and Treatment (2017)