Abstract
Background:
The efficacy of hepatic arterial infusion chemotherapy for the treatment of advanced hepatocellular carcinoma (HCC) remains unclear.
Methods:
The outcome of 476 patients with HCC who underwent hepatic arterial infusion chemotherapy with 5-fluorouracil and cisplatin (HAIC) were compared with 1466 patients who did not receive active therapy.
Results:
A survival benefit of the therapy after adjusting for known risk factors was observed (hazard ratio, 0.48; 95% CI, 0.41–0.56; P<0.0001). In propensity score-matched analysis (n=682), median survival time was longer for patients who underwent chemotherapy (14.0 months) than for patients who did not receive active treatment (5.2 months, P<0.0001).
Conclusion:
For advanced HCC, HAIC is considered to be an effective treatment.
Similar content being viewed by others
Main
Hepatocellular carcinoma (HCC) is one of the most common malignancies worldwide (Jemal et al, 2011). Screening patients with chronic liver diseases increases the chance that HCC can be diagnosed in the early stage (Kudo et al, 2011; European Association for Study of Liver; European Organisation for Research and Treatment of Cancer, 2012; Sherman et al, 2012). However, many HCCs are detected at an advanced stage.
According to the treatment algorithm of HCC, patients with advanced disease are candidates for chemotherapy (Kudo et al, 2011; European Organisation for Research and Treatment of Cancer, 2012; Sherman et al, 2012). Currently, sorafenib is the only chemotherapy proven to be effective for advanced HCC (Llovet et al, 2008; Cheng et al, 2009). Several other therapies have been evaluated, including hepatic arterial infusion of 5-fluorouracil (5-FU) and cisplatin, which was the most common regimen in Japan (Ueshima et al, 2010; Kim do et al, 2011; Yamashita et al, 2011). However, most of these studies were retrospective and nonrandomised; therefore, its efficacy remains unclear.
The Liver Cancer Study Group of Japan uses questionnaires to collect data from patients with HCC every 2 years, with several minor modifications of the contents since 1965 (Ikai et al, 2005, 2007). We used the three most recent sets of data to determine the efficacy of arterial infusion therapy with 5-FU and cisplatin for advanced HCC.
Materials and methods
Data sources
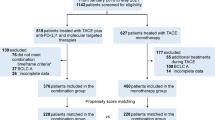
From January 2000 to December 2005, a total of 62 315 patients with primary liver cancer were newly registered by the Liver Cancer Study Group of Japan (Ikai et al, 2005, 2007). The cohort was followed up biannually and their clinical outcome was examined. Of these 62 315 patients, 57 445 (92.2%) received a diagnosis of HCC, and 31 743 patients with complete data were selected for this study. Among the patients, 1150 patients initially underwent chemotherapy and 1466 patients received no active therapy (no therapy group). In patients who underwent chemotherapy, 476 (41.4%) underwent arterial infusion chemotherapy with 5-FU and cisplatin using a subcutaneous infusion port (HAIC group). All patients in the HAIC group and in the no therapy group were enrolled in this study (Supplementary Figure 1).
Hepatocellular carcinoma was diagnosed primarily by imaging modalities such as computed tomography (1579, 81.3%), magnetic resonance imaging (257, 13.2%), ultrasonography (1167, 60.1%), and/or angiography (360, 18.5%) with the findings of hyperattenuation at the arterial phase and hypoattenuation at the portal phase and/or tumour staining. A histological diagnosis was made in 4.5% (n=87) of the patients. Treatment effect was evaluated by a criteria, ‘Treatment effect of the target nodule’, outlined by the Liver Cancer Study Group of Japan (Liver Cancer Study Group of Japan, 2003).
All data were provided anonymously. This study was approved by the review board of the Liver Cancer Study Group of Japan.
Statistical analysis
Continuous variables were compared by t-test, and categorical variables were compared by χ2 test. Survival was estimated by the Kaplan–Meier method and compared by the log-rank test.
Univariate and multivariate analyses of the primary cohort (n=1942) were carried out using the Cox proportional hazard model. Adjusted hazard ratios for HAIC according to subgroups (prognostic tumour factors in multivariate analysis) were also analysed and presented as a forest plot.
To determine the efficacy of HAIC, propensity score-matching analysis was performed (HAIC, n=476; no therapy, n=1466). A propensity score for use of HAIC was estimated using a logistic regression model fit with 15 variables: sex, age, hepatitis B surface antigen (HBsAg) positivity, hepatitis C virus (HCV) antibody positivity, alcohol intake, presence of encephalopathy, presence of ascites, total bilirubin, albumin, prothrombin time, maximum tumour size, tumour number, portal vein invasion, extrahepatic metastasis, and α-fetoprotein level. To create a propensity-matched cohort of patients who underwent HAIC or no therapy (1 : 1 match), a nearest-neighbour-matching algorithm with a ‘greedy’ heuristic was used (Austin and Mamdani, 2006).
The same matching procedure was carried out in patients with Child–Pugh A/B disease and portal vein invasion or more than three tumours, and survival rates for each matched cohort were compared.
Results
Patient characteristics
The HAIC group was significantly younger and had more males than the no therapy group (Supplementary Table 1). Patients in the HAIC group had better liver function but more cases of hepatitis B infection and more advanced tumours than the no therapy group. These differences except follow-up period disappeared after propensity score matching.
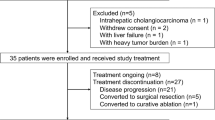
Treatment effect of HAIC
In the HAIC group, the response rates were as follows: complete response (CR, n=19, 4.0%), partial response (PR, n=173, 36.5%), stable disease (SD, n=112, 23.6%), progressive disease (PD, n=129, 27.2%), and undefined (n=41, 8.7%). The 1- and 3-year survival rates according to response were CR/PR (77.7% and 34.6%), SD (44.2% and 13.3%), and PD (23.7% and 10.3%), respectively (P<0.0001, Figure 1). All factors including HAIC treatment correlated with prognosis in the univariate analysis (Table 1). Multivariate analysis revealed that HBsAg, more than three tumours, large tumours (>3 cm), distant metastasis, portal vein invasion (VP3 and VP4), and high α-fetoprotein levels (>400 ng ml−1) were associated with poor survival. The VP3 and VP4 indicated tumour invasion to the first-order branches of the portal vein and the invasion to the main trunk of the portal vein, respectively (Liver Cancer Study Group of Japan, 2003). Conversely, Child–Pugh A/B disease (hazard ratio, 0.51; 95% confidence interval (CI), 0.45–0.59; P<0.0001) and HAIC (hazard ratio, 0.48; 95% CI, 0.41–0.56; P<0.0001) were associated with better survival.
Survival of patients who underwent hepatic arterial infusion of 5-fluorouracil and cisplatin using a subcutaneous infusion port. The 1- and 3-year survival rates and median survival times according to response were as follows: CR/PR (77.7%, 34.6%, 25.8 months), SD (44.2%, 13.3%, 9.5 months), and PD (23.7%, 10.3%, 6.0 months) (P<0.0001). Abbreviations: CR=complete response; PD=progressive disease; PR=partial response; SD=stable disease.
An exploratory subgroup analysis of patients who underwent HAIC therapy evaluated six prognostic variables: presence of HBsAg, tumour number, tumour size, presence of extrahepatic metastasis and vascular invasion, and α-fetoprotein levels. Compared with no therapy, HAIC improved survival, regardless of the values of these six prognostic factors (Supplementary Figure 2).
Survival rates of propensity score-matched cohorts
In the propensity score-matched cohort (n=682), 198 patients in the HAIC group and 199 patients in the no therapy group died during the observation period. The cause of death was liver related that included death by liver cancer as well as by liver failure in 184 patients (92.9%) in the HAIC group and 180 patients (90.4%) in the no therapy group (P=0.47). Median survival times were 14.0 months (HAIC group) and 5.2 months (no therapy group), and survival was significantly higher in the HAIC group (P<0.0001) (Figure 2). Hazard ratio of HAIC in this propensity score-matched cohort was 0.60 (95% CI, 0.49–0.73; P<0.0001). The same relationship was observed even when the event was limited to liver-related death (P<0.0001). Median survival times were 15.4 months (HAIC group) and 7.3 months (no therapy group).
Because most treatment guidelines for HCC recommend chemotherapy for patients with Child–Pugh A/B disease who have portal vein invasion and/or more than three tumours, we analysed the effect of HAIC in patients who met these criteria in the propensity score-matched cohort. In cases of Child–Pugh A/B disease with more than three tumours (370 propensity score-matched patients), median survival times were 13.9 months (HAIC) and 3.7 months (no therapy), and a survival benefit of HAIC treatment was observed (P<0.0001; Supplementary Figure 3). The same relationship was also observed in cases of Child–Pugh A/B disease with portal vein tumour thrombus (378 propensity score-matched patients, P<0.0001; Supplementary Figure 4). Median survival times were 7.9 months (HAIC) and 3.1 months (no therapy).
Discussion
Hepatic arterial infusion of cisplatin and 5-FU using a subcutaneous infusion port has been widely used in Japan to treat advanced HCC because of its relatively high response rate (27.8–57.1%) (Ando et al, 2002; Eun et al, 2009; Ueshima et al, 2010; Kim do et al, 2011; Kim et al, 2011); however, no randomized control trial has been conducted to demonstrate its effectiveness and survival benefit. Most reports of HAIC were retrospective studies with small numbers of patients. In this study we used data from a large-scale nationwide survey and found that the response rate to HAIC was high (40.5%), survival was prolonged, and response to therapy could be used as a surrogate marker for overall survival. The survival benefit was also observed when only liver-related deaths were treated as ‘events’.
Cisplatin interacts with DNA, preferentially binding nucleophilic N7 sites on purine bases (Galluzzi et al, 2012). As a consequence, protein–DNA complexes and DNA–DNA inter- and intra-strand adducts are generated, inducing cytotoxicity. Cisplatin also increases the folate concentration in cancer cells, reinforcing the effect of 5-FU through the formation of an inactive ternary complex (Scanlon et al, 1986; Kim et al, 2002). This synergistic effect of cisplatin and 5-FU is the basis of HAIC therapy.
Our study has some limitations. The information of dose reduction or termination due to drug toxicity is missing. Propensity scores were used to adjust for patient characteristics; however, it is not possible to adjust for all possible confounding factors related to survival, and the exact reasons of no therapy in control group were not known. Another weak point in this study is that performance status was not included as a covariate because two-thirds of the patients enrolled in this study lacked these data. However, the survival benefit of HAIC was observed even when the event was limited to liver-related death and when analysing the most recent database, which included performance status (median observation period 3 months, data not shown). Finally, we did not know the precise regimen used in this study population; however, many studies of HAIC report the administration of low-dose cisplatin (5–20 mg) several times a week, and continuous infusion of 5-FU for a few weeks.
As sorafenib has become the standard treatment for advanced HCC, several randomized controlled trials have been planned to evaluate new drugs using sorafenib as a control (Kudo, 2012). Some of these trials will evaluate HAIC, which will clarify some of the uncertainties of the present study.
In this large-scale retrospective study, we demonstrated the effectiveness of HAIC, although it was difficult to achieve long-term survival because HCCs re-grew even after response to the drugs. Our findings indicate that HAIC could be an alternative therapy for advanced HCC. Further examination of the factors that can predict the therapeutic effect is important for achieving long survival in future.
Change history
01 October 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ando E, Tanaka M, Yamashita F, Kuromatsu R, Yutani S, Fukumori K, Sumie S, Yano Y, Okuda K, Sata M (2002) Hepatic arterial infusion chemotherapy for advanced hepatocellular carcinoma with portal vein tumor thrombosis: analysis of 48 cases. Cancer 95 (3): 588–595.
Austin PC, Mamdani MM (2006) A comparison of propensity score methods: a case-study estimating the effectiveness of post-AMI statin use. Stat Med 25 (12): 2084–2106.
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, Luo R, Feng J, Ye S, Yang TS, Xu J, Sun Y, Liang H, Liu J, Wang J, Tak WY, Pan H, Burock K, Zou J, Voliotis D, Guan Z (2009) Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol 10 (1): 25–34.
Eun JR, Lee HJ, Moon HJ, Kim TN, Kim JW, Chang JC (2009) Hepatic arterial infusion chemotherapy using high-dose 5-fluorouracil and cisplatin with or without interferon-alpha for the treatment of advanced hepatocellular carcinoma with portal vein tumor thrombosis. Scand J Gastroenterol 44 (12): 1477–1486.
European Organisation for Research and Treatment of Cancer (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. Eur J Cancer 48 (5): 599–641.
Galluzzi L, Senovilla L, Vitale I, Michels J, Martins I, Kepp O, Castedo M, Kroemer G (2012) Molecular mechanisms of cisplatin resistance. Oncogene 31 (15): 1869–1883.
Ikai I, Arii S, Ichida T, Okita K, Omata M, Kojiro M, Takayasu K, Nakanuma Y, Makuuchi M, Matsuyama Y, Yamaoka Y (2005) Report of the 16th follow-up survey of primary liver cancer. Hepatol Res 32 (3): 163–172.
Ikai I, Arii S, Okazaki M, Okita K, Omata M, Kojiro M, Takayasu K, Nakanuma Y, Makuuchi M, Matsuyama Y, Monden M, Kudo M (2007) Report of the 17th Nationwide Follow-up Survey of Primary Liver Cancer in Japan. Hepatology Res 37 (9): 676–691.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61 (2): 69–90.
Kim BK, Park JY, Choi HJ, Kim do Y, Ahn SH, Kim JK, Lee do Y, Lee KH, Han KH (2011) Long-term clinical outcomes of hepatic arterial infusion chemotherapy with cisplatin with or without 5-fluorouracil in locally advanced hepatocellular carcinoma. J Cancer Res Clin Oncol 137 (4): 659–667.
Kim do Y, Ahn SH, Kim SU, Choi SB, Lee KH, Park MS, Park JY, Lee do Y, Han KH, Kim KS (2011) Adjuvant hepatic arterial infusional chemotherapy with 5-fluorouracil and cisplatin after curative resection of hepatocellular carcinoma. Oncology 81 (3-4): 184–191.
Kim R, Tanabe K, Inoue H, Toge T (2002) Mechanism(s) of antitumor action in protracted infusion of low dose 5-fluorouracil and cisplatin in gastric carcinoma. Int J Oncol 20 (3): 549–555.
Kudo M (2012) Targeted therapy for liver cancer: updated review in 2012. Curr Cancer Drug Targets 12 (9): 1062–1072.
Kudo M, Izumi N, Kokudo N, Matsui O, Sakamoto M, Nakashima O, Kojiro M, Makuuchi M HCC Expert Panel of Japan Society of Hepatology (2011) Management of hepatocellular carcinoma in Japan: Consensus-Based Clinical Practice Guidelines proposed by the Japan Society of Hepatology (JSH) 2010 updated version. Dig Dis 29 (3): 339–364.
Liver Cancer Study Group of Japan (2003) General Rules for the Clinical and Pathological Study of Primary Liver Cancer Second English edition. Kanehara & Co. Ltd: Tokyo.
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR, Seitz JF, Borbath I, Haussinger D, Giannaris T, Shan M, Moscovici M, Voliotis D, Bruix J, SIS Group (2008) Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 359 (4): 378–390.
Scanlon KJ, Newman EM, Lu Y, Priest DG (1986) Biochemical basis for cisplatin and 5-fluorouracil synergism in human ovarian carcinoma cells. Proc Natl Acad Sci USA 83 (23): 8923–8925.
Sherman M, Bruix J, Porayko M, Tran T, Committee APG (2012) Screening for hepatocellular carcinoma: the rationale for the American Association for the Study of Liver Diseases recommendations. Hepatology 56 (3): 793–796.
Ueshima K, Kudo M, Takita M, Nagai T, Tatsumi C, Ueda T, Kitai S, Ishikawa E, Yada N, Inoue T, Hagiwara S, Minami Y, Chung H (2010) Hepatic arterial infusion chemotherapy using low-dose 5-fluorouracil and cisplatin for advanced hepatocellular carcinoma. Oncology 78 (Suppl 1): 148–153.
Yamashita T, Arai K, Sunagozaka H, Ueda T, Terashima T, Yamashita T, Mizukoshi E, Sakai A, Nakamoto Y, Honda M, Kaneko S (2011) Randomized, phase II study comparing interferon combined with hepatic arterial infusion of fluorouracil plus cisplatin and fluorouracil alone in patients with advanced hepatocellular carcinoma. Oncology 81 (5-6): 281–290.
Acknowledgements
This work was supported in part by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Nouso, K., Miyahara, K., Uchida, D. et al. Effect of hepatic arterial infusion chemotherapy of 5-fluorouracil and cisplatin for advanced hepatocellular carcinoma in the Nationwide Survey of Primary Liver Cancer in Japan. Br J Cancer 109, 1904–1907 (2013). https://doi.org/10.1038/bjc.2013.542
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.542
Keywords
This article is cited by
-
Advanced therapeutics avenues in hepatocellular carcinoma: a novel paradigm
Medical Oncology (2023)
-
Hepatobiliary-phase gadolinium ethoxybenzyl-diethylenetriaminepentaacetic acid MRI for pretreatment prediction of efficacy-to-standard-therapies based on Barcelona Clinic Liver Cancer algorithm: an up-to-date review
European Radiology (2023)
-
Comparison of Arterial Infusion Chemotherapy and Chemoembolization for Locally Advanced Hepatocellular Carcinoma: a Multicenter Retrospective Study
Journal of Gastrointestinal Surgery (2022)
-
Pembrolizumab plus lenvatinib with or without hepatic arterial infusion chemotherapy in selected populations of patients with treatment-naive unresectable hepatocellular carcinoma exhibiting PD-L1 staining: a multicenter retrospective study
BMC Cancer (2021)
-
Impact of the extent of axillary surgery in patients with N2–3 disease in the de-escalation era: a propensity score-matched study
Clinical and Translational Oncology (2021)