Abstract
Background:
The celebrity Jade Goody’s cervical cancer diagnosis was associated with increased UK cervical screening attendance. We wanted to establish if there was an increase in high-grade (HG) cervical neoplasia diagnoses, and if so, what the characteristics of the women with HG disease were.
Methods:
We analysed prospective data on 3233 consecutive colposcopy referrals in North East London, UK, from 01 April 2005 to 30 June 2010. Characteristics and outcomes of pre- and post-Goody cohorts were compared.
Results:
Goody’s diagnosis was associated with an increased incidence of colposcopy referrals in all subsequent annual quarters (incidence rate ratio (IRR) 1.3–1.9, P<0.002–P<0.0005) and increased HG disease diagnoses in the fourth quarter 2008/2009 (IRR 1.3, P=0.05) and first quarter 2009/2010 (IRR 1.3, P=0.07). We observed 1.90-fold (CI: 1.06–3.39), 2.06 (CI: 1.13–3.76) and 2.13-fold (CI: 1.07–4.25) respective increases in the odds of HG disease women being screening-naive in the first and second quarter 2009/2010, and the first quarter 2010/2011 (P<0.04, P<0.02 and P<0.04, respectively). There was a 2.23-fold increase in the odds of screening-naive HG disease women being symptomatic post-Goody’s diagnosis (P=0.023). The age distributions of the pre- and post-Goody cohorts did not differ in any study group.
Conclusion:
Continued publicity about celebrities’ diagnoses might encourage screening in at-risk populations.
Similar content being viewed by others
Main
The effect of celebrities’ diagnoses on cancer screening behaviour is well established (Chapman et al, 2005; Larson et al, 2005). The US Centre for Disease Control and Prevention noted a temporal association in mammography uptake following Nancy Reagan’s breast cancer diagnosis in 1987 (Lane et al, 1989). More recently, Kylie Minogue’s breast cancer diagnosis was associated with an increase in primary-care referrals to breast clinics and screening attendance in the UK and Australia, respectively (Chapman et al, 2005; Twine et al, 2006; Kelahar et al, 2008). Even fictional characters can influence screening uptake; a popular UK soap opera character’s death from cervical cancer in 2001 resulted in a 21% increase in women undergoing cervical screening (Howe et al, 2002).
Whether the increased uptake of screening results in any increase in the diagnosis of significant pathology has been less well studied; Kylie Minogue’s breast cancer diagnosis was associated with a significant increase in referrals to a UK rapid access breast clinic, but no increase in the number of cancers diagnosed (Twine et al, 2006). Public health campaigns to increase awareness of HIV testing have also resulted in an increase in screening uptake, but no increase in diagnoses (Ross and Scott, 1993).
In August 2008, the UK reality TV star Jade Goody was diagnosed with cervical cancer, from which she died in March 2009. Her illness was well covered by all forms of media, bringing cervical cancer into the public consciousness. Dubbed the ‘Jade Goody effect’, subsequent national data reported a 12% increase in the number of cervical cytology samples performed in 2008/2009 (NHS Cervical Screening Programme, 2009) and a 10% increase in referrals to colposcopy (The Health and Social Care Information Centre, 2009) following Goody’s diagnosis and death. A recent UK cancer registry report (Office for National Statistics, 2009) found a 19.2% increase in cervical carcinoma in situ (CIS) between 2008 and 2009, particularly in the 15–19 years and 25–29 years age groups. The report attributed this to the ‘Jade Goody effect’. However, a direct temporal relationship is not available from this report, which provides CIS registrations and age distribution only. Recent data from the NHS cervical screening program (Lancucki et al, 2012) did demonstrate a temporal relationship and increased screening attendance particularly among women under 50 years old and those overdue with routine recall. However, it did not report on final pathological outcome nor on attendance of screening-naive women. More detailed evidence is required to establish a clear link between the ‘Jade Goody effect’ and the increase in cervical CIS registrations. The high-resolution data required to investigate this hypothesis can also provide insights into the characteristics of the women who attend for screening. These may be helpful in informing future public health strategy.
The median cervical screening coverage within Tower Hamlets (the area contributing the highest proportion of our patients and the third most deprived local authority in the country; Tower Hamlets, 2008) was 70.4% pre- and post-Goody’s diagnosis (Public Health England, 2010), compared with a national average of 78.9% in 2008/2009 (The Health and Social Care Information Centre, 2012). This suggests not only that our local cervical screening uptake was lower than in the wider UK population, but also that at first sight, Goody’s diagnosis had no effect on local screening uptake. However, because women of lower socioeconomic status often do not participate in cancer screening (Loerzel and Bushy, 2005), and are more likely to present with a higher stage of disease (Schwartz et al, 2003), it might only take a small increase in attendance of such women to improve the detection of high-grade (HG) disease. In addition, coverage does not necessarily reflect changes in the a priori risk level of the population attending screening during different time periods. Consequently, absence of an obvious increase in screening coverage does not necessarily mean that the rate and proportion of women diagnosed with HG disease will remain unchanged.
We wanted to establish whether the extra burden placed on the cervical screening service resulted in any benefit to the women who underwent screening in Goody’s wake. We examined two questions; first, was the increase in colposcopy referrals temporally associated with an increase in HG disease diagnoses, that is, cervical intra-epithelial neoplasia grades 2 and 3, HG cervical glandular intra-epithelial neoplasia and micro-invasive/invasive cervical cancers? Second, if there was an increase in HG disease diagnoses, what were the characteristics of the women diagnosed?
Materials and methods
Confirmation was obtained from the chair of the local National Research Ethics Service (NRES) committee that the work undertaken in this study did not require formal NRES review. We examined anonymised data extracted from the Barts Health NHS Trust colposcopy departmental database (Chameleon Information Management System, Infoflex, v5, London, UK) containing prospectively collected mandatory information on all 3233 colposcopy referrals from 1 April 2005 to 30 June 2010 from a population of over 220 000 women in North East London served by our department. We chose this time period because it started immediately following introduction of liquid-based cytology as the sole method of assessing cervical cytology in our region. Before this, conventional Papanicolaou smears were still being used, and could have confounded results. We recorded indication for and date of referral, age at referral and final diagnosis following colposcopic evaluation and/or treatment as appropriate. We grouped the data into annual quarters (Q), with Q1 starting 1 April and finishing 30 June and so on. This is the method used by all UK colposcopy departments for mandatory reporting of data for quality control purposes. There was a minimum of 2 years follow-up after referral to allow for any potential delays in diagnosis of HG disease.
Data were split into two cohorts; pre- and post-Goody’s diagnosis in 2008/2009 Q2. Age distributions of the entire pre- and post-Goody diagnosis cohorts were plotted in 5-year age groups and compared using the Mann–Whitney U-test. A similar subgroup analysis was performed for the women diagnosed with HG disease. The number of referrals and HG disease diagnoses for each Q post-Goody’s diagnosis were compared with the pre-Goody diagnosis cohort baseline figure, with incidence rate ratios (IRRs) estimated using Poisson regression, adjusted for length of time. Owing to the issue of multiple testing, the 95% confidence intervals should not be used as indicators of significance but of precision only. Statistical significance may be assessed by comparing the P-value to an adjusted critical value; a conservative Bonferroni correction would give an alpha of 0.00625. The proportion of women referred with a HG cytology result for each Q post-Goody’s diagnosis were compared with the pre-Goody diagnosis cohort baseline proportion, with odds ratios (OR) estimated using logistic regression.
In order to further characterise the women diagnosed with HG disease, screening histories were extracted from Open Exeter, the UK national screening database (Version 20.4; NHS Connecting for Health, Exeter, UK). It was not possible to access complete screening histories for a minority (6.3%) of women with HG disease because: (1) we had no record of their NHS number, (2) they had been screened outside the NHS screening program and (3) their most recent screen had been performed outside our area. These women were excluded from further analyses.
‘Screening-naive’ women were defined as those who had not undergone cervical cytology sampling before the assessment (cytological or clinical) resulting in referral to colposcopy. All other women were defined as ‘previously screened’. In the ‘previously screened’ group, the interval between any referral cytology sample and the sample preceding the referral sample was calculated, and mean sample intervals in the pre- and post-Goody diagnosis groups were compared using a two sample t-test. No adjustment was required for multiple testing, as this analysis did not involve multiple comparisons.
Odds ratios were calculated, comparing the proportion of women with HG disease who were screening-naive post-Goody’s diagnosis with the baseline proportion pre-Goody’s diagnosis, using logistic regression. The symptom histories (postcoital, intermenstrual or postmenopausal bleeding) of screening-naive women with HG disease were extracted from the departmental database, and proportions of women who were symptomatic pre- and post-Goody’s diagnosis were calculated using the χ2 test. As the number of women fitting this description was too small to permit meaningful quarterly comparisons, pre- and post-Goody quarterly data were pooled. Therefore, there were no multiple comparisons, so no adjustments to the significance level alpha were required.
Results
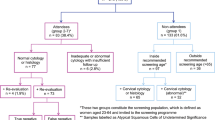
There were 3233 referrals to colposcopy during the study period. The median pre-Goody diagnosis quarterly referral rate was 127. We observed increases in the quarterly incidence of colposcopy referrals in all quarters post-Goody’s diagnosis throughout the duration of the study (IRR 1.3–1.9, P<0.002–P<0.0005; Table 1A; Figure 1A). These differences reached the predetermined significance level of P<0.000625 for all but one of the quarters of the study.
Post-Goody quarterly incident rate ratios for ( A ) referrals to colposcopy and ( B ) HG disease diagnosis and ORs for ( C ) proportion of referrals with HG diagnosis and ( D ) proportion of women with HG disease who were screening-naive. X axis units=annual quarters. Error bars=95% confidence intervals.
The mean pre-Goody diagnosis quarterly incidence of HG disease was 46 (range 28–61). We observed increases in the quarterly incidence of HG disease diagnoses in 2008/2009 Q4 (IRR 1.3, P=0.05) and 2009/2010 Q1 (IRR 1.3, P=0.07) after Goody’s diagnosis. Subsequent Qs were generally lower than baseline, most prominently in 2009/2010 Q4 (IRR 0.65, P=0.02; Table 1B; Figure 1B). None of these differences reached the predetermined significance level of 0.00625 (taking multiple testing into account). We observed decreases in the odds of referred women being diagnosed with HG disease in all post-Goody quarters except 2008/2009 Q4 compared with the baseline odds (OR 0.36–0.63, P<0.02–P<0.0005). These differences reached the predetermined significance level of P<0.00625 for the last four quarters of the study (Table 1C; Figure 1C). There were 25 cases of invasive cancer pre-Goody’s diagnosis compared with 26 cases post-Goody’s diagnosis (mean 1.92 vs 3.25 cases per Q, respectively, P=0.061).
There were 600 women diagnosed with HG disease. The proportion of women with HG disease who were screening-naive pre-Goody’s diagnosis was 25.1%. We observed 1.90-fold (CI: 1.06–3.39), 2.06 (CI: 1.13–3.76) and 2.13-fold (CI: 1.07–4.25) respective increases in the odds of women with HG disease being screening-naive in 2009/10 Q1, 2009/2010 Q2 and 2010/2011 Q1 after Goody’s diagnosis (P<0.04, P<0.02 and P<0.04, respectively; Table 1D; Figure 1D). None of these differences reached the predetermined significance level of P<0.00625.
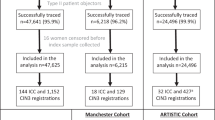
There was no difference in screening interval between pre- and post-Goody’s diagnosis HG disease cohorts, with a mean time between referral cytology and the preceding sample of 3.2 years in both groups. None of the screening-naive women with HG disease post-Goody’s diagnosis were aged over 45 years, whereas 4% of those pre-Goody’s diagnosis were aged >45 years. The age distributions of the pre- and post-Goody diagnosis cohorts did not differ significantly in any of the study groups (Figure 2).
Age distribution of the study groups. There were no significant differences between the pre-Goody and post-Goody cohorts in any of these groups. (A) Age distribution of the study population (n=3233). (B) Age distribution of women with HG disease (n=600). (C) Age distribution of women with HG disease who were screening-naive (n=141). Abbreviation: JG=Jade Goody.
Among screening-naive women with HG disease, the proportions with symptoms pre- and post-Goody’s diagnosis were 11.3% and 22.2%, respectively. This was a significant 2.23-fold (95% CI: 1.05–4.79) increase in the odds of screening-naive women with HG disease being symptomatic post-Goody’s diagnosis (χ2 P=0.023. No adjustment was required for multiple testing, as this analysis did not involve multiple comparisons).
Discussion
In our population, the time period following Goody’s diagnosis and her subsequent death was associated with significant increases in referrals to colposcopy and nonsignificant (when accounting for multiple testing) increases in HG disease diagnoses. These results mirror those seen in the UK national data (Office for National Statistics, 2009; The Health and Social Care Information Centre, 2009). In our cohort, referrals increased immediately after Goody’s diagnosis and had still not returned to baseline 2 years later. In contrast, the increase in HG diagnosis did not become apparent until approximately 9 months after Goody’s diagnosis, but fell below baseline after three further Qs and returned to baseline 15 months post-Goody’s diagnosis. As a result, there was no difference in the number of HG diagnoses per quarter in the post-Goody period overall compared with the pre-Goody period. The proportion of referred women diagnosed with HG disease fell in the months following Goody’s diagnosis and had not returned to baseline 2 years later. Women diagnosed with HG disease after Goody’s diagnosis were more likely to be screening-naive, symptomatic women compared with those referred before Goody’s diagnosis. However, they did not differ significantly in age from those diagnosed pre-Goody’s diagnosis, nor were they more likely to have had a longer cytology interval before their diagnosis if they were not screening-naive.
As far as we are aware, this is the first time that an increase in celebrity-triggered screening has been associated in a temporary increase in detection of significant pathology. The high-resolution study design allowed us to explore the characteristics of the women with HG disease in detail so that inferences could be drawn, which may be helpful in focussing targeted promotion of screening to at-risk populations.
The limitations of this study are that it was done in just one colposcopy centre located close to where Goody lived during her illness (Upshire, Essex). It is therefore possible that our findings were a ‘local’ phenomenon, not applicable to other settings. In addition, the size of the study limited statistical power and this is the likely explanation for observing nonsignificant (after adjustment for multiple testing) increases in the number of HG diagnoses in the earlier post-Goody quarters. The study did not examine the patient characteristics of the entire colposcopy population, because we wanted to focus our resources on the women diagnosed with HG disease. This is the group in which screening uptake is key to avoiding cancer-related morbidity and mortality. It is information about this group, rather than those attending screening without significant pathology, which should inform targeted publicity to encourage screening uptake. Our method of assessing the proportion of women who were screening-naive may have underestimated the effect of Goody’s diagnosis on prompting women to attend for screening, as it did not take into account women who required one or more cytology samples to trigger referral to colposcopy (e.g., those with multiple sequential inadequate samples). However, even with this potential underestimate, we still observed an increased proportion of screening-naive women among those with HG disease post-Goody’s diagnosis.
The increase in observed colposcopy referrals after Goody’s diagnosis mirrors the increase in referrals for breast cancer screening in the UK and Australia following Kylie Minogue’s diagnosis (Chapman et al, 2005; Twine et al, 2006; Kelahar et al, 2008). In Australia, Kelahar et al reported there was a 101% increase in non-screened women attending (similar to the proportional increase we observed). However, the increase in referrals and mammograms performed in these women did not result in an increase in breast cancer diagnoses in Australia (Kelahar et al, 2008) nor the United Kingdom (Twine et al, 2006). This may be because the increase in screening following Kylie Minogue’s diagnosis was predominantly among younger women at low risk of having breast cancer who are not normally offered screening, whereas our data indicate that the increase in referrals to colposcopy following Goody’s diagnosis occurred across all age groups. The very close temporal association between Goody’s diagnosis, increased colposcopy referrals and increased numbers of HG diagnoses implies probable causality, suggesting that the ‘Jade Goody effect’ was responsible for the increased numbers of HG diagnoses in the UK in 2009–2010 (Office for National Statistics, 2009).
This study confirms that celebrity-prompted increases in disease awareness are potentially powerful influences on screening uptake. In addition, in contrast to the data on breast screening, this increase in screening uptake can result in an increase in disease diagnosis. This could be due to increases in awareness of the symptoms of the disease or awareness of the importance of screening (Loerzal and Bushy, 2005). In addition, identification with the celebrity may prompt women to attend screening (Kalichman et al, 1993), and a national survey found that younger women from poorer socioeconomic backgrounds were those most likely to report their decisions about cervical screening as having been influenced by Goody’s diagnosis (Marlow et al, 2012). Given the higher risk characteristics of the post-Goody HG disease cohort in our area (more screening-naive, symptomatic women), we speculate that the ‘Jade-Goody effect’ resulted in the diagnosis of significant pathology in a group of women who might otherwise never have attended screening, and may therefore have prevented disease-related deaths. However, the absolute increase in HG diagnoses was coupled with a reduced proportion of referred women being diagnosed with HG disease. This implies that many more ‘worried well’ attended for screening in addition to those finally diagnosed with HG disease. In addition, although there was a temporary increase in the absolute numbers of women diagnosed with HG disease, this fell below baseline within 9 months, returning to baseline by 2 years post-Goody’s diagnosis. This meant that there was no difference in the mean quarterly number of HG diagnoses in the post-Goody period compared with the pre-Goody period, suggesting that the effect may have ‘pulled forward’ date of diagnosis in the at-risk population. It will, therefore, be crucial to establish whether the national data indicate a reduced number of cases of CIS in 2010/2011 compared with the years before Goody’s diagnosis, commensurate with a ‘pull forward’ effect.
This study demonstrates that clinicians and policymakers should consider the potential impact on screening-uptake when a celebrity openly discusses their disease. Although such events are uncommon, their impact may be great and hence development of contingency plans for dealing with any increase in demand for screening should be considered. In addition, they should also consider the opportunities for providing public health information, as the majority of newspaper articles did not use Goody’s diagnosis as a means of imparting potentially helpful knowledge about cervical cancer (Hilton and Hunt, 2010).
It is entirely possible that the 6-month lag before HG diagnosis rates increased after Goody’s diagnosis reflects not only a snowballing ‘Jade Goody effect’, but also the difficulty the screening and colposcopy service had in accommodating the huge increase in referrals. The observation that the effect on quarterly HG diagnosis numbers appeared to have ‘worn off’ in our cohort just 12 months after Goody’s diagnosis reinforces the need for regular targeted screening promotion. It may be prudent for the screening service to continue to publicise Goody’s story, perhaps on an annual basis, on the anniversary of her death.
In order to investigate whether the ‘Jade Goody effect’ had a national impact on HG disease diagnoses, and whether this was sustained, or merely a ‘pull forward’ effect, we recommend this study is repeated using national data. Such information could prove valuable in designing future public health campaigns to target the women at highest risk of cervical cancer and improve their uptake of screening.
Change history
03 September 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Chapman S, McLeod K, Wakefield M, Holding S (2005) Impact of celebrity illness of breast cancer screening: Kylie Minogue’s breast cancer diagnosis. Med J Aust 183: 247–250.
Hilton S, Hunt K (2010) Coverage of Jade Goody’s cervical cancer in UK newspapers: a missed opportunity for health promotion? BMC Public Health 10: 368.
Howe A, Owen-Smith V, Richardson J (2002) The impact of a television soap opera on the NHS Cervical Screening Programme in the North West of England. J Public Health Med 24: 299–304.
Kalichman SC, Russell RL, Hunter TL, Sarwer DB (1993) Earvin ‘Magic’ Johnson’s HIV serostatus disclosure: effects on men’s perceptions of AIDS. J Consult Clin Psychol 61: 887–891.
Kelaher M, Cawson J, Miller J, Kavanagh A, Dunt D, Studdert DM (2008) Use of breast cancer screening and treatment services by Australian women aged 25-44 years following Kylie Minogue’s breast cancer diagnosis. Int J Epidemiol 37: 1326–1332.
Lancucki L, Sasieni P, Patnick J, Day TJ, Vessey MP (2012) The impact of Jade Goody’s diagnosis and death on the NHS Cervical Screening Programme. J Med Screen 19: 89–93.
Lane DS, Polednak AP, Burg MA (1989) The impact of media coverage of Nancy Reagan’s experience on breast cancer screening. Am J Public Health 79: 1551–1552.
Larson RJ, Woolshin S, Schwartz LM, Welch HG (2005) Celebrity endorsements of cancer screening. J Natl Cancer Inst 97: 693–695.
Loerzel VW, Bushy A (2005) Interventions that address cancer health disparities in women. Fam Community Health 28: 79–89.
Marlow LA, Sangha A, Patnick J, Waller J (2012) The Jade Goody effect: whose cervical screening decisions were influenced by her story? J Med Screen 19: 184–188.
NHS Cervical Screening Programme (2009) Knowledge Drives Our Programme, Annual Review 2009. NHS Cervical Screening Programme: Sheffield.
Office for National Statistics (2009) Cancer Statistics Registrations [online]. Available at http://www.ons.gov.uk/ons/rel/vsob1/cancer-statistics-registrations--england--series-mb1-/no--40--2009/index.html. Accessed 19 November 2012.
Public Health England (2010) Cervical Screening Coverage: 2007-2008 [online]. Available at http://www.londonqarc.nhs.uk/section.php?id=301. Accessed 19 Nov 2012.
Ross JD, Scott GR (1993) The association between HIV media campaigns and number of patients coming forward for HIV antibody testing. Genitourin Med 69: 193–195.
Schwartz KL, Crossley-May H, Vigneau FD, Brown K, Banerjee M (2003) Race, socioeconomic status and stage at diagnosis for five common malignancies. Cancer Causes Control 14: 761–766.
The Health and Social Care Information Centre (2009) Cervical Screening Programme England 2008–2009. The Health and Social Care Information Centre: London.
The Health and Social Care Information Centre (2012) Cervical Screening Programme 2008/09. [online] Available at http://www.ic.nhs.uk/statistics-and-data-collections/screening/cervical-screening/cervical-screening-programme-england-2008-09. Accessed 19 November 2012.
Tower Hamlets (2008) Local Development Framework – Setting the Scene. [online] (Updated July 2008). Available at www.towerhamlets.gov.uk/idoc.ashx?docid=82f88ae7-a8b2. Accessed 26 November 2012. http://www.towerhamlets.gov.uk/lgsl/851-900/855_planning_consultation/core_strategy.aspx.
Twine C, Barthelmes L, Gateley CA (2006) Kylie Minogue’s breast cancer: effects on referrals to a rapid access breast clinic in the UK. Breast 15: 667–669.
Acknowledgements
We thank all the staff who dealt with the huge increase in workload caused by the ‘Jade Goody effect’, including entering data onto the relevant databases.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Casey, G., Morris, B., Burnell, M. et al. Celebrities and screening: a measurable impact on high-grade cervical neoplasia diagnosis from the ‘Jade Goody effect’ in the UK. Br J Cancer 109, 1192–1197 (2013). https://doi.org/10.1038/bjc.2013.444
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.444
Keywords
This article is cited by
-
FANatics: Systematic literature review of factors associated with celebrity worship, and suggested directions for future research
Current Psychology (2021)
-
Raising awareness of oral cancer from a public and health professional perspective
British Dental Journal (2018)
-
Changes of Socio-demographic data of clients seeking genetic counseling for hereditary breast and ovarian cancer due to the “Angelina Jolie Effect”
BMC Cancer (2016)
-
Oral cancer: exploring the stories in United Kingdom newspaper articles
British Dental Journal (2016)
-
Angelina and Brad effect
Familial Cancer (2016)