Abstract
Background:
131I-meta-iodobenzylguanidine (131I-MIBG) has been in therapeutic use since 1980s. Newer treatment modalities are emerging for neuroendocrine tumours (NETs) and chromaffin cell tumours (CCTs), but many of these do not yet have adequate long-term follow-up to determine their longer term efficacy and sequelae.
Methods:
Fifty-eight patients with metastatic NETs and CCTs who had received 131I-MIBG therapy between 2000 and 2011 were analysed. Survival and any long-term haematological or renal sequelae were investigated.
Results:
In the NET group, the overall median survival and median survival following the diagnosis of metastatic disease was 124 months. The median survival following the commencement of 131I-MIBG was 66 months. For the CCT group, median survival had not been reached. The 5-year survival from diagnosis and following the diagnosis of metastatic disease was 67% and 67.5% for NETs and CCTs, respectively. The 5-year survival following the commencement of 131I-MIBG therapy was 68%. Thirty-two patients had long-term haematological sequelae: 5 of these 32 patients developed haematological malignancies. Two patients developed a mild deterioration in renal function.
Conclusion:
Long follow up of 131I-MIBG therapy reveals a noteable rate of bone marrow toxicities and malignancy and long term review of all patients receiving radionuclide therapies is recommended.
Similar content being viewed by others
Main
Neuroendocrine tumours (NETs) are a diverse group of neoplasms that are derived from cells within endocrine organs and the diffuse neuroendocrine system (Barakat et al, 2004). These tumours are highly variable in their location and clinical behaviour, ranging from well-differentiated, slow-growing tumours to poorly differentiated, highly aggressive tumours. In the majority, initial growth tends to be slow and asymptomatic, and patients often have metastatic disease at the time of initial presentation. By this stage, patients are usually incurable by surgery and systemic treatment is used with the aims of control of symptoms arising from excess hormone production from the tumours, together with tumour stabilisation or cytoreduction (Druce et al, 2010).
The options for systemic therapy include medical treatment such as alpha- and beta-adrenoceptor blockade to protect against cardiovascular instability from catecholamine secretion by chromaffin cell tumours (CCTs), and somatostatin analogues to reduce the production of mediators by gastroenteropancreatic NETs (GEP-NETs). Radiotherapy and chemotherapy have also been used with variable success (Moertel et al, 1991; Kaltsas et al, 2001b). Other newer therapies include tyrosine kinase inhibitors (Raymond et al, 2011) and inhibitors of the mammalian target of rapamycin (Yao et al, 2011) for pancreatic NETs, and somatostatin analogues for NETs of mid-gut origin (Rinke et al, 2009). Another treatment option for the control of symptoms and stabilisation of the tumour is radionuclide therapy. Radionuclides are unstable forms of chemical elements that emit nuclear radiation when they undergo radioactive decay. Radionuclide therapy aims to deliver these radionuclides to the target tissue via an appropriate carrier that will deliver the radiation to the target site. Tissue damage is by direct or indirect DNA damage in the affected cells and the ‘bystander effect’ resulting in damage to neighbouring cells. An example of this type of therapy in common usage is 131Iodine therapy for differentiated thyroid cancer. Another such radiolabelled therapy is 131I-meta-iodobenzylguanidine (131I-MIBG). The use of 131I-MIBG within a treatment algorithm is still under debate, though data are being reviewed (Gulenchyn et al, 2012) and new tools being explored (Spetz et al, 2012).
131I-meta-iodobenzylguanidine comprises radioactive iodine coupled with meta-iodo-benzyl-guanidine. Meta-iodo-benzyl-guanidine is an arkyl-guanidine derivative, which is structurally similar to noradrenaline, and is taken up into cells of neural crest origin by active transport. Its similarity to noradrenaline and active uptake by neuroendocrine cells has allowed the use of 131I-MIBG over the past 30 years in identifying and treating tumours of neural crest origin such as phaeochromocytomas, paragangliomas, and neuroblastomas, and occasionally NETs and medullary thyroid cancers that may express MIBG uptake mechanisms (Kaltsas et al, 2001a; Modlin et al, 2006; Jiang et al, 2009). Indications for the use of 131I-MIBG are usually for symptom relief in inoperable patients with slowly progressive metastatic disease. However, in the UK guidelines there is no clear position for its use in the treatment pathway as each patient is considered on a case-by-case basis. 131I-meta-iodobenzylguanidine would be a favourable choice if high radionuclide uptake is demonstrated on 123I-MIBG scanning (Ramage et al, 2012). Studies have shown overall tumour response rates in NETs of 30% (Lewington, 2003) and 58% for CCTs in various reports (Troncone et al, 1991), although the data are limited by their retrospective nature and non-controlled study designs. Response to 131I-MIBG therapy, which is not in the remit of this paper, would be measured hormonally with serum chromogranin A and/or urinary 5-HIAA for NETs. 131I-meta-iodobenzylguanidine would improve the condition in 40–80% of patients (Loh et al, 1997; Mukherjee et al, 2001; Gedik et al, 2008; Nwosu et al, 2008; Bomanji and Papathanasiou, 2012) and radiologically by demonstrating a reduction in size, though this occurs less often (at 20–30%) and by patients’ report of symptoms at 50–89% (Gedik et al, 2008; Nwosu et al, 2008; Shilkrut et al, 2010).
The number of patients diagnosed with NETs and those surviving some forms of neuroendocrine cancer is increasing (Halfdanarson et al, 2008; Tsikitis et al, 2012), and hence it is important to focus on the long-term effects that the cancer itself and the treatments offered may have on the patient (Department of Health, 2010). Cancer survivors’ health and well-being are diminished compared with non-cancer sufferers, and there is a move towards thinking about patients living with (and in some cases beyond) cancer in much the same way as patients with non-malignant chronic diseases (Elliott et al, 2011). Therefore, assessing the benefits and long-term sequelae of therapy is important in patient care, and also helps to inform treatment strategies for future patients. The aim of our study was to review the outcomes and sequelae following 131I-MIBG therapy used in our centre for NETs. Other treatment modalities have been discussed in detail in other publications (Kaltsas et al, 2004; Kwekkeboom et al, 2005; Basu et al, 2010; Druce et al, 2010). The relatively long follow-up of our patients who have received 131I-MIBG has allowed us to audit the overall survival (OS) of our patients, and also to consider persistent toxicities and late effects.
Materials and methods
The institutional, prospectively collated database was available electronically for all patients who underwent 131I-MIBG therapy between the years 2000 and 2011, and their data were reviewed. Patients were split into two groups: NETs and CCTs. The NET group consisted of all patients with NETs of any origin including GEP-NETs and medullary thyroid carcinoma.
Patients selected for 131I-MIBG therapy were those with metastatic disease and adequate 123I-MIBG uptake on diagnostic scanning: these patients tended to fall within the group with low-grade, progressive disease. Patients with rapidly progressive and high mitotic index tumours more usually received systemic chemotherapy.
The protocol for the administration of 131I-MIBG in our institution has been previously described (Mukherjee et al, 2001). In summary, potassium iodide formerly and more recently potassium iodate was given 2 days before and 3 days after 131I-MIBG therapy to prevent uptake of 131I by the thyroid gland. Recent EANM guidelines have suggested a longer length of potassium iodate to be given, so some patients in this cohort received potassium iodate for up to 10 days post 131I-MIBG therapy (Giammarile et al, 2008). 131I-meta-iodobenzylguanidine was administered by slow intravenous infusion with monitoring of vital signs. Following the administration of 131I-MIBG, patients were nursed in a radiation-protected isolation room until their emitting radiation levels were deemed safe. Post-therapy scanning was carried out to confirm persistent uptake of 131I-MIBG. The standard practice was to administer up to 6 doses in total, at 6-monthly intervals, each dose of around 7.2 GBq, with a total cumulative dose of 45 GBq. Patients were followed up 3–6 months following each therapy dose for clinical and biochemical reassessment.
All patients had a full blood count, urea and electrolytes before and after therapy. Patients with GEP-NETs were also assessed using 24 h urinary 5-HIAA and/or chromogranin A levels. Those with CCTs were monitored using 24 h urinary catecholamines or metanephrines. Calcitonin levels were measured in those with medullary thyroid cancer.
Toxicity
We assessed the incidence of persistent haematological and renal toxic effects, at least 6 months following 131I-MIBG therapy by monitoring patients’ full blood count and renal function. Haematological and renal toxicity was graded according to the NCI Common Terminology Criteria for Adverse Events v3.0 (Trotti et al, 2003). We also assessed patients’ thyroid function following 131I-MIBG therapy.
Statistical analysis
Patient data and demographic information were analysed using descriptive statistics. Median values and interquartile ranges (IQRs) were calculated for data that were non-normally distributed. Fisher’s exact test was used to compare groups of discrete data, unpaired t-test for continuous Gaussian distributed data and the Wilcoxon rank-sum test for continuous non-Gaussian distributed data. The Kruskal–Wallis test was used for comparison of more than two groups. Survival analysis was performed using the Kaplan–Meier survival curves. A P-value of <0.05 was deemed to be statistically significant.
Results
Complete data were available for 67 patients with diagnoses of phaeochromocytoma, paraganglioma, and NETs. Patients receiving adjuvant therapy for treatment of an incompletely resected but non-metastatic primary tumour were excluded from the analysis. In total, therefore, data from 58 patients were analysed. Of the 58 patients included, 44 patients had metastatic NETs and 14 had CCTs (Table 1).
The median age was 61.5 (IQR±18.75) years in the NET group and 43 (IQR±17.5) years in the chromaffin cell group. There was equal sex distribution in both groups. For the NET group, the median overall follow-up was 91.5 (IQR±78, range 10–288) months, the median follow-up from first diagnosis of metastatic disease was 79 (IQR±73.75, range 10–265) months and from commencement of first 131I-MIBG therapy was 47.5 (IQR±67.75, range 4–202) months. At the time of analysis, 20 patients in this group were still alive while 24 had died.
For the CCT group, the median follow-up from diagnosis was 57.5 (IQR±98, range 20–338) months, from first diagnosis of metastatic disease was 56.5 (IQR±98, range 8–134) months and from commencement of first 131I-MIBG therapy was 46.5 (IQR±37.5, range 7–122) months. Ten patients were still alive while four had died.
The tumour origin within the neuroendocrine group consisted of 19 tumours of GI tract origin, 8 pancreatic, 2 lung, 2 ovarian, 1 medullary thyroid cancer, and 12 with unknown primary (Figure 1). For the CCT group, seven patients had phaeochromocytomas and seven had paragangliomas. Liver metastases were prominent in patients with NETs, present in 41 of the patients: 13 had bone metastases, 15 had lymph-node involvement, 8 abdominal (peritoneal and mesentery involvement), 6 lung, and 2 mediastinal. In the CCT group, there were six patients with liver metastases, eight with spread to bone, four lung, four lymph node, three peritoneal and one with mediastinal metastases.
Treatment
A total of 157 doses of 131I-MBG were given. The median number of therapies given per patient was 2.5 (IQR±3) and 2 (IQR±1) therapy doses given to the NET and CCT patients, respectively. Twelve patients in the NET group and three in the CCT group had just a single dose of 131I-MIBG. The median total cumulative doses given were 20.5 GBq (IQR±21.56) and 21.3 GBq (IQR±12.78).
Thirty three patients received treatments other than 131I-MIBG during the course of their treatment. Of the NET patients, 41% had 131I-MIBG therapy alone (excluding surgery), while 59% had therapies additional to 131I-MIBG including chemotherapy (25%), external beam radiotherapy to painful metastases (16%), hepatic embolisation (5%), alpha-interferon (7%), or somatostatin analogues (25%) (Table 2).
Half of the CCT group had MIBG as sole therapy (excluding surgery) while the other half also received additional therapy including chemotherapy (29%) or external beam radiotherapy (36%) (Table 2).
Survival
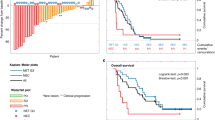
Survival, expressed as a median value in months and 50% survival rate, was calculated from three different time points: OS from diagnosis, survival following the diagnosis of metastatic disease, and third survival rate after the commencement of 131I-MIBG therapy (Figure 2). For the NET group, the overall median survival from diagnosis was 124 months, with a 5-year survival of 53%. From the diagnosis of metastatic disease, the median survival remained at 124 months, with a 5-year survival of 50%. Following 131I-MIBG therapy, median survival was 66 months and the 5-year survival was 46%. For the CCT group, median survival is not reported because, within our timeframe, over 50% of the patients were still alive. The 5-year survival from first diagnosis was 67%. Following the diagnosis of metastatic disease, the 5-year survival was 67.5% and following the commencement of treatment with 131I-MIBG therapy, the 5-year survival was 68%.
Sequelae
There were 15 patients in total with grade 1 or 2 renal impairment and 1 patient with grade 3 impairment before receiving 131I-MIBG therapy. These patients had comorbidities that affected renal function. Of these patients, 10 had hypertension, 4 had diabetes mellitus, 1 hydronephrosis, 1 renal cell carcinoma, 1 nephrectomy for tuberculosis, 2 were on a combination of diuretics for tricuspid and pulmonary valve regurgitation, 1 on diuretics for oedema and ascites, 1 had paraproteinaemia, and 1 unknown. Within this group, two showed a deterioration of their eGFR from 82 to 63 ml min−1 1.73 m2 and 80 to 66 ml min−1 1.73 m2 (normal to grade 1). Three patients also showed improvement in their eGFR (40–60 ml min−1 1.73 m2, 54–80 ml min−1 1.73 m2, and 67–69 ml min−1 1.73 m2) (Table 3).
Overall, 32 patients developed new and/or sustained haematological effects. The majority of the haematological effects were mild at grades 1–2, but grades 3–4 were also present. For grades 1–2 within the NET group, thrombocytopaenia was seen in 27% of patients, neutropaenia in 9%, and anaemia in 39%. For grades 3–4, thrombocytopaenia was found in 7%, neutropaenia in 2%, and anaemia in 2%. Grade 1–2 haematological events in the CCT group showed thrombocytopaenia in 14% of patients, neutropaenia in 14%, and anaemia in 36%. A grade 3–4 haematological effect in the CCT group was 7% with thrombocytopaenia, 14% with neutropaenia, and 7% with anaemia (Table 4). The Kruskal–Wallis test was performed to compare whether there was a difference in cumulative doses received between those who developed different grades of haematological adverse events (normal vs grade 1–2 vs grade3–4 vs haematological malignancy): this did not reach formal significance (P=0.067).
Comparing patients with and without haematological sequelae, the factors investigated were age, sex, renal function, prior chemotherapy, presence of bone metastases, number of cycles of therapy, and cumulative radiation doses. None of these factors significantly increased haematological adverse events (Table 5).
Of the patients with haematological sequelae, five patients were noted to have more significant consequences, including the development of myelodysplasia, chronic myeloid leukaemia (CML), or acute myeloid leukaemia (AML) (Table 6). Two of the five patients have died as a direct result of their haematological malignancy; in one instance this developed some time after the treatment, and the initial prognosis for the NET had already been markedly exceeded, while in the other, additional risk factors for haematological abnormality had also been present (namely, the use of methotrexate for rheumatoid arthritis). On analysing this group of patients in particular, age, sex, months from follow-up, renal function before commencement of 131I-MIBG therapy, and previous exposure were not statistically significant factors in those who developed haematological malignancy. However, both number of cycles received (P=0.01) and cumulative dose (P=0.01) were significantly higher in this subgroup compared with those who did not develop haematological malignancy in this cohort. The cumulative incidence of haematological malignancy was 8.6% (95%CI 1.38–15.82%). The calculated person-years at risk for this cohort is 1099 per 100 000 person-years.
Thyroid function tests (TFTs) before and subsequently after 131I-MIBG were complete in 30 patients. Within the 30 complete data, 2 developed hypothyroidism (6.25%) after therapy and 1 patient already had a TSH of 7.6 mIU l−1 before the commencement of therapy which rose to 23 mIU l−1. The cumulative doses received in patients with normal thyroid function compared with those who developed hypothyroidism were not statistically significant (P=0.29). There were no cases of thyroid nodules or thyroid malignancy reported. From the remaining 28 patients with incomplete data, 1 patient had medullary thyroid cancer, 9 normal pre treatment, 8 had normal TFTs during treatment, 3 had normal TFTs after treatment, 2 were hypothyroid on blood tests after therapy but there were no TFTs before treatment, 1 had a raised TSH of 5.1 mIU l−1 pretreatment and 4 did not have any TFTs done.
Discussion
We have described a sizeable cohort of patients who have received 131I-MIBG therapy with a long duration of follow-up and survival. We have shown that patients with low-grade metastatic NETs and CCTs have a long survival period in the majority of cases, with median OS from diagnosis of 124 months in NETs. However, the rapidity of disease progression is hard to predict, as shown by some patients whose disease did not stabilise after 131I-MIBG therapy and required chemotherapy treatment shortly after. Yao et al (2008) reported on the survival of NET of over 35 000 patients, including both high- and low-grade tumours using information from the SEER database. This study showed a median OS of the whole cohort of 75 months. Further analysis involved separating the NETs into histological groups: patients with well-differentiated NETs (G1) had an OS of 124 months and those with moderately differentiated tumours (G2) 64 months. However, combining G1 and G2 groups, those with localised, regional, or distant disease had a median survival of 223, 111, and 33 months, respectively. The group most similar to our cohort for comparison would be the G1/G2 group with distant metastases, with a median survival of 33 months. However, this study was only based on histological diagnoses and survival and did not take into account which therapies were administered. Jarufe et al (2005) reviewed 44 patients following the surgical resection over a period of 14 years with a median survival of 81 months.
Published data other than from the SEER database include a series of over 900 patients in whom the median OS was 7.9 years (94 months) for advanced small bowel NET and 3.9 years (46.8 months) for advanced panNET (Ter-Minassian et al, 2013), while another of 399 patients (Pape et al, 2008) showed a median OS of metastatic patients of estimated median survival for NET-related death according to the Kaplan–Meier analysis was 169 months. However, a number of such studies review prognostic factors related to the patient and tumour but do not report the variety of treatment modalities employed or provide any comparisons. It is difficult therefore to identify with certainty pure series of patients with similar characteristics treated with and without radionuclide therapy, particularly as some physicians in countries without access to the treatment still send their patients abroad to receive it.
Although relatively small in number, our cohort demonstrates a median survival from demonstration of metastases in the NET group of longer than the SEER database at 124 months but not as long as the Pape et al series. The heterogeneity of our cohort and the non-randomised nature of the sample means that bias cannot be excluded, and therefore comparison of survival compared with all the other cohorts cannot simply be attributed to the 131I-MIBG therapy. However, our cohort does provide us with a good opportunity to review the long-term sequelae of disease and therapy.
Within the CCT group, our 5-year survival rate was comparable to other studies with a 5-year survival of 78%. Other studies have shown 5-year survival of between 30% and 80% (Sclafani et al, 1990; Vassilopoulou-Sellin, 1998). Sclafani et al (1990) reported a 5-year survival of 36%. Vassilopoulou-Sellin’s (1998) study had a very long follow-up of 50 patients and showed a 5-year survival of paragangliomas of 30% and phaeochromocytoma of 80%. The advances in the genetics of CCTs being identified may explain the difference between Sclafani’s study and ours, with patients identified much earlier and treated, hence showing a better survival. However, this is not necessarily borne out by the data−indeed, within our cohort, only four patients have had positive genetic studies to date: one VHL and three SDH-B mutations. Following 131I-MIBG therapy, the OS of our cohort may be compared with other, similar patient groups. Safford et al (2003) described a cohort with the same median follow-up as our group at about 50 months, and a median survival of 28 months, while our cohort had a median survival of 78 months. There were differences between the two studies, for example; where patients in the Safford study received single higher doses of 131I-MIBG of about 15 GBq, our patients received one or multiple smaller doses of about 7 GBq per dose.
The long survival of our patients has provided an opportunity to investigate the long-term sequelae of the treatment received. Most importantly, with the benefit of the long-term follow-up, we have noted a substantial increase in the number of haematological events, including haematological malignancies. The five patients involved had diagnoses including CML, AML, and myelodysplastic syndrome, none of which has been extensively described in previous publications of 131I-MIBG therapy in NETs or CCTs. Nwosu et al (2008) using 131I-MIBG at the same doses per treatment cycle as our cohort for their NET patients did not have any haematological malignancies in their cohort of 48 patients, though their follow-up was shorter with a median of 31 months and lower cumulative doses received at 13.3 GBq. In contrast, Gonias et al (2009), who treated 50 patients with metastatic phaeochromcytomas, had 2 patients who developed haematological malignancies, though these patients received much higher cumulative doses of 63 and 68 GBq. Cumulative doses in our cohort lie in between the two, with the lowest cumulative dose in this subgroup being 28.05 GBq while the highest was 43.9 GBq. Cumulative doses received are likely to influence the risk of haematological malignancies as shown in our cohort, and the higher doses in Gonias et al series may also explain why none was seen in the Nwosu et al series as they received much lower cumulative doses.
It is important to consider whether malignancies are more common in this group because of the treatment directly (higher cumulative doses) rather than that the patients are surviving longer, reaching an age where haematological malignancies more commonly occur. Comparing our data with the available statistics, the occurrence is much higher in our cohort than that of the age-matched general population. Our incidence was high at 1099 per 100 000 person-years, which is much higher than in comparison with UK national statistics of age-matched incidences: 1.9 per 100 000 population aged between 60 and 74 years with CML; 6.4 per 100 000 population aged between 60 and 74 and 0.6 per 100 000 population if aged 15–59 years for myelodysplasia; and 21.6 per 100 000 population aged 75+years and 1.9 per 100 000 if aged 15–59 years (HMRN, 2012). Whether this increase in incidence is a genuine risk from 131I-MIBG therapy cannot be answered fully in this non-randomised, non-placebo-controlled cohort study, and would be better answered in the future by comparing with other treatments that individualise to patient’s disease. It is crucial to note that many of these patients have had several modalities of treatment prior or after 131I-MIBG therapy, which could also increase the risk of haematological malignancies, but they were not shown to be significant factors during analysis of this subgroup of patients to predict the increased risk of the development of haematological malignancy. A larger cohort of patients and prospective data would be helpful in this regard. Of critical importance are the comparative side-effect profiles of the different therapies available. Prospective and longer duration follow-up of the newer therapies, especially somatostatin peptide receptor radionuclide therapy (PRRT), will be really important to fully judge the long-term benefits and risks of these treatments and their place in comparison with conventional and targeted chemotherapies. It is possible that the increased survival associated with PRRT will allow such haematological malignancies to appear over time.
Other haematological sequelae, in the form of myelosuppression, have been previously described with all forms of treatment of NETs and CCTs. With radionuclide therapy, haematological side effects have been reported in the region of 2–21% (Gedik et al, 2008; Nwosu et al, 2008; Kunikowska et al, 2011; Bomanji and Papathanasiou, 2012; Gulenchyn et al, 2012). Different chemotherapies have a different toxicity profile. Hatton and Reed (1997) used a combination of dacarbazine, vincristine, and cyclophosphamide for a heterogeneous group of patients including NETs and CCTs and reported grade 3–4 haematological toxicity in 12 of their 18 patients. In our institution, lomustine and 5-FU is more commonly used for NETs (Kaltsas et al, 2001b), and transient bone marrow suppression is seen in many, but permanent bone marrow suppression was seen in only 2 out of 18 patients. The newer treatments available, everolimus and sunitinib, showed anaemia, thrombocytopaenia, and neutropaenia rates of between 13% and 29% (Raymond et al, 2011; Yao et al, 2011). None of these studies reported haematological malignancies, but the follow-up period remains in the early stages. Some studies on PRRT have described a few cases of haematological malignancies (Valkema et al, 2006; Iten et al, 2007). However, the completeness of very long-term follow-up on these cohorts of patients is uncertain. It is also important to bear in mind that many of these patients have metastatic bone disease and bone marrow infiltration−thus, the bone marrow suppression may in some instances result from the disease rather than the treatment itself. In such cases, management may differ and treatment of the tumour may improve the bone marrow suppression. However, in our study, we had not looked at the actual number and size of the bone metastases at the time of haematological toxicity and cannot draw any conclusions as to whether a considerable load on haematopoietic potential was present. We have just presented the observation of the presence of bone metastases in our cohort. The nature of our cohort being heterogenous and retrospective also makes comparison of the haematological safety of 131I-MIBG with other therapies more difficult due to different biological behaviours and different combination of therapies applied to each patient. Large prospective studies in the future would be needed to compare different treatments for patients with the same biological behaviour.
In terms of comparative effects on renal function, of all the modalities, only PRRT has been documented to permanently and adversely affect renal function. This was reported in about 10% of patients being treated by Kunikowska et al (2011) in a cohort of 50 patients. Modern PRRT incorporates renal protection using an amino-acid infusion before therapy with PRRT. Our cohort had 16 patients who already had renal impairment due to pre-existing comorbidities, but following 131I-MIBG 2 patients had mild deterioration in renal function, which then stabilised.
Our cohort showed a hypothyroid rate of 6.25% but as our data were retrospective, the data were incomplete for many of our patients and this will need to be addressed prospectively as hypothyroidism, thyroid nodules and thyroid cancers have all been described after 131I-MIBG administration in children (van Santen et al, 2012; Teszler, 2013). There were no thyroid nodules or cancers reported in our cohort. The rate of hypothyroidism is comparable to the Nwosu et al’s NET series at 6.3% though they had a lower mean cumulative dose of 13.3 GBq. Other series had higher hypothyroid rates at 16.7% with a median cumulative dose of 39.6 GBq (Castellani et al, 2010) and 20% with a mean cumulative dose of 11.6 GBq (Shilkrut et al, 2010). None of these series had a similar median cumulative rate as our cohort (median 20.5 GBq for NETs and 21.3 GBq for CCTs).
Overall, 131I-MIBG therapy in patients with low-grade metastatic disease showed similar survival and toxicity to other therapies. The 131I-MIBG therapy appears to be safe, even in those with a low glomerular filtration rate as it did not cause further deterioration in renal function after therapy. The haematological sequelae we have highlighted here in patients suggest that clinicians must be aware of potential adverse events that may only become evident in patients under prolonged follow-up, especially in those who have received higher cumulative doses. Individual patients should be monitored and followed up closely. The factors identified that could potentially influence the risk of the development of haematological malignancy were the number of cycles and the cumulative radiation received. Others factors which we would predict to influence the development of haematological sequelae, such as bone metastases and previous exposures (such as chemotherapy) did not reach statistical significance. This may reflect the small sample size of our cohort to investigate these factors, hence not providing sufficient power for evaluation and the heterogenous nature of the cohort may also have a role. It is also important to consider the development of national registries for patients undergoing therapies of this type so that patterns of rare or very late sequelae can be detected in patients with this rare group of tumours.
We acknowledge that the limitation to this paper is the use of a cohort with a mixed group of tumour types with different disease burdens. This makes comparison with other studies difficult but the aim of this paper was to highlight possible long-term sequelae following the 131I-MIBG therapy rather than comparison of treatment outcomes. Multi-centre studies would be desirable for prospective studies of a single tumour type to fully assess the efficacy and side effects of 131-I-MIBG therapy in each tumour type.
In summary, our study has shown that patients with low-grade, metastatic NET and CCT have good OS. As a consequence of longer survival and a long duration of follow-up, we were able to elicit the development of occasional clinically significant haematological consequences in the form of leukaemias and the myelodysplastic syndrome. While not possible to demonstrate that this was the direct effect of 131I-MIBG therapy, it is an important potential consideration. Long-term registries of patients receiving all types of radionuclide therapy should be considered to monitor possible long-term consequences of therapy as well as efficacy so that protocols suggesting best sequencing of therapy can be evaluated.
Change history
06 August 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Barakat MT, Meeran K, Bloom SR (2004) Neuroendocrine tumours. Endocr Relat Cancer 11: 1–18.
Basu B, Sirohi B, Corrie P (2010) Systemic therapy for neuroendocrine tumours of gastroenteropancreatic origin. Endocr Relat Cancer 17: R75–R90.
Bomanji JB, Papathanasiou ND (2012) (1)(1)(1)In-DTPA(0)-octreotide (Octreoscan), (1)(3)(1)I-MIBG and other agents for radionuclide therapy of NETs. Eur J Nucl Med Mol Imaging 39 (Suppl 1): S113–S125.
Castellani MR, Seghezzi S, Chiesa C, Aliberti GL, Maccauro M, Seregni E, Orunesu E, Luksch R, Bombardieri E (2010) (131)I-MIBG treatment of pheochromocytoma: low versus intermediate activity regimens of therapy. Q J Nucl Med Mol Imaging 54: 100–113.
Department of Health MCSNi (2010) The National Cancer Survivorship Initiative Vision: Department of Health publications. www.dh.gov.uk/publications.
Druce MR, Lewington V, Grossman AB (2010) Targeted radionuclide therapy for neuroendocrine tumours: principles and application. Neuroendocrinology 91: 1–15.
Elliott J, Fallows A, Staetsky L, Smith PW, Foster CL, Maher EJ, Corner J (2011) The health and well-being of cancer survivors in the UK: findings from a population-based survey. Br J Cancer 105 (Suppl 1): S11–S20.
Gedik GK, Hoefnagel CA, Bais E, Olmos RA (2008) 131I-MIBG therapy in metastatic phaeochromocytoma and paraganglioma. Eur J Nucl Med Mol Imaging 35: 725–733.
Giammarile F, Chiti A, Lassmann M, Brans B, Flux G (2008) EANM procedure guidelines for 131I-meta-iodobenzylguanidine (131I-mIBG) therapy. Eur J Nucl Med Mol Imaging 35: 1039–1047.
Gonias S, Goldsby R, Matthay KK, Hawkins R, Price D, Huberty J, Damon L, Linker C, Sznewajs A, Shiboski S, Fitzgerald P (2009) Phase II study of high-dose [131I]metaiodobenzylguanidine therapy for patients with metastatic pheochromocytoma and paraganglioma. J Clin Oncol 27: 4162–4168.
Gulenchyn KY, Yao X, Asa SL, Singh S, Law C (2012) Radionuclide therapy in neuroendocrine tumours: a systematic review. Clin Oncol (R Coll Radiol) 24: 294–308.
Halfdanarson TR, Rabe KG, Rubin J, Petersen GM (2008) Pancreatic neuroendocrine tumors (PNETs): incidence, prognosis and recent trend toward improved survival. Ann Oncol 19: 1727–1733.
Hatton MQ, Reed NS (1997) Chemotherapy for neuroendocrine tumors: the Beatson Oncology Centre experience. Clin Oncol (R Coll Radiol) 9: 385–389.
HMRN (2012) http://www.hmrn.org/Statistics/Incidence.aspx/.
Iten F, Muller B, Schindler C, Rochlitz C, Oertli D, Macke HR, Muller-Brand J, Walter MA (2007) Response to [90Yttrium-DOTA]-TOC treatment is associated with long-term survival benefit in metastasized medullary thyroid cancer: a phase II clinical trial. Clin Cancer Res 13: 6696–6702.
Jarufe N, McMaster P, Mayer AD, Mirza DF, Buckels JA, Orug T, Tekin K, Bramhall SR (2005) Surgical treatment of metastases to the pancreas. Surgeon 3: 79–83.
Jiang L, Schipper ML, Li P, Cheng Z (2009) 123I-labeled metaiodobenzylguanidine for diagnosis of neuroendocrine tumors. Rep Med Imaging 2: 79–89.
Kaltsas G, Korbonits M, Heintz E, Mukherjee JJ, Jenkins PJ, Chew SL, Reznek R, Monson JP, Besser GM, Foley R, Britton KE, Grossman AB (2001a) Comparison of somatostatin analog and meta-iodobenzylguanidine radionuclides in the diagnosis and localization of advanced neuroendocrine tumors. J Clin Endocrinol Metab 86: 895–902.
Kaltsas G, Mukherjee JJ, Plowman PN, Grossman AB (2001b) The role of chemotherapy in the nonsurgical management of malignant neuroendocrine tumours. Clin Endocrinol (Oxf) 55: 575–587.
Kaltsas GA, Besser GM, Grossman AB (2004) The diagnosis and medical management of advanced neuroendocrine tumors. Endocr Rev 25: 458–511.
Kunikowska J, Krolicki L, Hubalewska-Dydejczyk A, Mikolajczak R, Sowa-Staszczak A, Pawlak D (2011) Clinical results of radionuclide therapy of neuroendocrine tumours with 90Y-DOTATATE and tandem 90Y/177Lu-DOTATATE: which is a better therapy option? Eur J Nucl Med Mol Imaging 38: 1788–1797.
Kwekkeboom DJ, Teunissen JJ, Bakker WH, Kooij PP, de Herder WW, Feelders RA, van Eijck CH, Esser JP, Kam BL, Krenning EP (2005) Radiolabeled somatostatin analog [177Lu-DOTA0,Tyr3]octreotate in patients with endocrine gastroenteropancreatic tumors. J Clin Oncol 23: 2754–2762.
Lewington VJ (2003) Targeted radionuclide therapy for neuroendocrine tumours. Endocr Relat Cancer 10: 497–501.
Loh KC, Fitzgerald PA, Matthay KK, Yeo PP, Price DC (1997) The treatment of malignant pheochromocytoma with iodine-131 metaiodobenzylguanidine (131I-MIBG): a comprehensive review of 116 reported patients. J Endocrinol Invest 20: 648–658.
Modlin IM, Latich I, Zikusoka M, Kidd M, Eick G, Chan AK (2006) Gastrointestinal carcinoids: the evolution of diagnostic strategies. J Clin Gastroenterol 40: 572–582.
Moertel CG, Kvols LK, O’Connell MJ, Rubin J (1991) Treatment of neuroendocrine carcinomas with combined etoposide and cisplatin. Evidence of major therapeutic activity in the anaplastic variants of these neoplasms. Cancer 68: 227–232.
Mukherjee JJ, Kaltsas GA, Islam N, Plowman PN, Foley R, Hikmat J, Britton KE, Jenkins PJ, Chew SL, Monson JP, Besser GM, Grossman AB (2001) Treatment of metastatic carcinoid tumours, phaeochromocytoma, paraganglioma and medullary carcinoma of the thyroid with (131)I-meta-iodobenzylguanidine [(131)I-mIBG]. Clin Endocrinol (Oxf) 55: 47–60.
Nwosu AC, Jones L, Vora J, Poston GJ, Vinjamuri S, Pritchard DM (2008) Assessment of the efficacy and toxicity of (131)I-metaiodobenzylguanidine therapy for metastatic neuroendocrine tumours. Br J Cancer 98: 1053–1058.
Pape UF, Berndt U, Muller-Nordhorn J, Bohmig M, Roll S, Koch M, Willich SN, Wiedenmann B (2008) Prognostic factors of long-term outcome in gastroenteropancreatic neuroendocrine tumours. Endocr Relat Cancer 15: 1083–1097.
Ramage JK, Ahmed A, Ardill J, Bax N, Breen DJ, Caplin ME, Corrie P, Davar J, Davies AH, Lewington V, Meyer T, Newell-Price J, Poston G, Reed N, Rockall A, Steward W, Thakker RV, Toubanakis C, Valle J, Verbeke C, Grossman AB (2012) Guidelines for the management of gastroenteropancreatic neuroendocrine (including carcinoid) tumours (NETs). Gut 61: 6–32.
Raymond E, Dahan L, Raoul JL, Bang YJ, Borbath I, Lombard-Bohas C, Valle J, Metrakos P, Smith D, Vinik A, Chen JS, Horsch D, Hammel P, Wiedenmann B, Van Cutsem E, Patyna S, Lu DR, Blanckmeister C, Chao R, Ruszniewski P (2011) Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med 364: 501–513.
Rinke A, Muller HH, Schade-Brittinger C, Klose KJ, Barth P, Wied M, Mayer C, Aminossadati B, Pape UF, Blaker M, Harder J, Arnold C, Gress T, Arnold R (2009) Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol 27: 4656–4663.
Safford SD, Coleman RE, Gockerman JP, Moore J, Feldman JM, Leight GS Jr, Tyler DS, Olson JA Jr. (2003) Iodine -131 metaiodobenzylguanidine is an effective treatment for malignant pheochromocytoma and paraganglioma. Surgery 134: 956–962, discussion 962-3.
Sclafani LM, Woodruff JM, Brennan MF (1990) Extraadrenal retroperitoneal paragangliomas: natural history and response to treatment. Surgery 108: 1124–1129, discussion 1129-30.
Shilkrut M, Bar-Deroma R, Bar-Sela G, Berniger A, Kuten A (2010) Low-dose iodine-131 metaiodobenzylguanidine therapy for patients with malignant pheochromocytoma and paraganglioma: single center experience. Am J Clin Oncol 33: 79–82.
Spetz J, Dalmo J, Nilsson O, Wangberg B, Ahlman H, Forssell-Aronsson E (2012) Specific binding and uptake of 131I-MIBG and 111In-octreotide in metastatic paraganglioma--tools for choice of radionuclide therapy. Horm Metab Res 44: 400–404.
Ter-Minassian M, Chan JA, Hooshmand SM, Brais LK, Daskalova A, Heafield R, Buchanan L, Qian ZR, Fuchs CS, Lin X, Christiani DC, Kulke MH (2013) Clinical presentation, recurrence, and survival in patients with neuroendocrine tumors: results from a prospective institutional database. Endocr Relat Cancer 20: 187–196.
Teszler CB (2013) Differentiated thyroid carcinoma after iodine-131 metaiodobenzylguanidine treatment for neuroblastoma: assessment of causality. Thyroid 23: 248–249.
Troncone L, Rufini V, Daidone MS, De Santis M, Luzi S (1991) [131I]metaiodobenzylguanidine treatment of malignant pheochromocytoma: experience of the Rome group. J Nucl Biol Med 35: 295–299.
Trotti A, Colevas AD, Setser A, Rusch V, Jaques D, Budach V, Langer C, Murphy B, Cumberlin R, Coleman CN, Rubin P (2003) CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol 13: 176–181.
Tsikitis VL, Wertheim BC, Guerrero MA (2012) Trends of incidence and survival of gastrointestinal neuroendocrine tumors in the United States: a seer analysis. J Cancer 3: 292–302.
Valkema R, Pauwels S, Kvols LK, Barone R, Jamar F, Bakker WH, Kwekkeboom DJ, Bouterfa H, Krenning EP (2006) Survival and response after peptide receptor radionuclide therapy with [90Y-DOTA0,Tyr3]octreotide in patients with advanced gastroenteropancreatic neuroendocrine tumors. Semin Nucl Med 36: 147–156.
van Santen HM, Tytgat GA, van de Wetering MD, van Eck-Smit BL, Hopman SM, van der Steeg AF, Nieveen van Dijkum EJ, van Trotsenburg AS (2012) Differentiated thyroid carcinoma after 131I-MIBG treatment for neuroblastoma during childhood: description of the first two cases. Thyroid 22: 643–646.
Vassilopoulou-Sellin R (1998) Clinical outcome of 50 patients with malignant abdominal paragangliomas and malignant pheochromocytomas. Endocr Relat Cancer 5: 59–68.
Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, Abdalla EK, Fleming JB, Vauthey JN, Rashid A, Evans DB (2008) One hundred years after ‘carcinoid’: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 26: 3063–3072.
Yao JC, Shah MH, Ito T, Bohas CL, Wolin EM, Van Cutsem E, Hobday TJ, Okusaka T, Capdevila J, de Vries EG, Tomassetti P, Pavel ME, Hoosen S, Haas T, Lincy J, Lebwohl D, Oberg K (2011) Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med 364: 514–523.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Sze, W., Grossman, A., Goddard, I. et al. Sequelae and survivorship in patients treated with 131I-MIBG therapy. Br J Cancer 109, 565–572 (2013). https://doi.org/10.1038/bjc.2013.365
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.365
Keywords
This article is cited by
-
Management and outcome of metastatic pheochromocytomas/paragangliomas: an overview
Journal of Endocrinological Investigation (2021)