Abstract
Background:
The host immune reaction is represented by immune/inflammatory cell infiltrates. Here we systematically analysed tumour-infiltrating immune/inflammatory cells in pancreatic ductal carcinoma (PDC) and evaluated their clinicopathological impact.
Methods:
Using immunohistochemistry, we examined tumour-infiltrating CD68+ pan-macrophages, HLA-DR+CD68+ M1 macrophages (M1), CD163+ or CD204+ M2 macrophages (M2), CD66b+ neutrophils (Neu), CD4+ T cells (CD4+T), CD8+ T cells (CD8+T), and FOXP3+CD4+ regulatory T cells (Treg) in 212 cases of PDC, and conducted correlation and survival analyses using the Kaplan–Meier method and Cox proportional hazards model.
Results:
Higher levels of tumour-infiltrating pan-macrophages, M2, Neu, or the ratio of Tregs to CD4+T (%Treg) were significantly associated with shorter survival, whereas higher levels of tumour-infiltrating CD4+T, CD8+T, or the ratio of M1 to pan-macrophages (%M1) were significantly associated with longer survival. Survival analysis of pairs of these variables revealed that some of the resulting patient groups had exclusively longer survival. We then connected the apparently related factors, and two significant variables emerged: tumour-infiltrating CD4+Thigh/CD8+Thigh/%Treglow and tumour-infiltrating %M1high/M2low. Multivariate survival analysis revealed that these variables were significantly correlated with longer survival and had a higher hazard ratio.
Conclusion:
Tumour-infiltrating CD4+Thigh/CD8+Thigh/%Treglow and %M1high/M2low are independent prognosticators useful for evaluating the immune microenvironment of PDC.
Similar content being viewed by others
Main
The tumour microenvironment, comprising multiple cellular and molecular factors, has important roles in the biological behaviour of cancer (Hanahan and Weinberg, 2011). The host immune reaction, as represented by tumour-infiltrating immune/inflammatory cells, is one of the leading players in the tumour microenvironment (Dunn et al, 2004; Sica and Bronte, 2007; Biswas and Mantovani, 2010; Ferrone and Dranoff, 2010; Grivennikov et al, 2010; Hiraoka et al, 2011). Recent extensive studies using animal models have helped to clarify the molecular and cellular mechanisms that define the roles of immune/inflammatory cells in the tumour microenvironment. Such knowledge of the human cancer microenvironment in real terms is important for the development and application of cancer therapy, especially immunotherapy. The microenvironment of human cancer is complex, and often shows different characteristics according to the tissues from which tumours develop, the carcinogenetic pathways involved, and tumour stages. In colorectal and ovarian cancers, a high proportion of CD8+ T cells or CD45RO+ memory T cells infiltrating the cancer tissue can be a favourable prognostic indicator (Zhang et al, 2003; Pages et al, 2005). In contrast, several kinds of tumour-infiltrating immune/inflammatory cells, such as regulatory T cells (Tregs), myeloid-derived suppressor cells (MDSCs), and alternatively activated macrophages, support tumour growth and extension by suppressing host immune responses, and accelerating angiogenesis and tissue remodelling (Dunn et al, 2004; Hiraoka et al, 2006; Sica and Bronte, 2007; Biswas and Mantovani, 2010; Grivennikov et al, 2010). Macrophages are heterogeneous and can be divided into classically activated macrophages (alternatively M1 macrophages, M1) that are activated mainly by Th1 cytokines and alternatively activated macrophages (alternatively M2 macrophages, M2) that are activated mainly by Th2 cytokines (Mantovani et al, 2002; Mosser and Edwards, 2008; Biswas and Mantovani, 2010; Sica and Mantovani, 2012). Thus, it is anticipated that tumour-infiltrating immune/inflammatory cells would be useful hallmarks for evaluating the characteristics of the tumour immune microenvironment and for immune monitoring of tumour tissues in both non-treated and treated patients. In addition to the clinicopathological impact of individual tumour-infiltrating cell types and subsets of immune/inflammatory cells, it is important to observe the interactions among these infiltrating cells to understand the actual conditions within the tumour microenvironment, as the effects of specific cell combinations may also be of clinicopathological significance. Therefore, systematic analysis of several tumour-infiltrating immune/inflammatory cells characteristic of innate or adaptive immune responses in the same type of cancer tissue would appear to be of potential importance. However, very few such studies have yet been performed.
Pancreatic cancer (pancreatic ductal carcinoma (PDC)) is the fourth and fifth leading cause of cancer-related death in the United States and Japan, respectively (Center for Cancer Control and Information Services & National Cancer Center, 2009; Siegel et al, 2011). PDC is one of the most aggressive cancers, with almost equivalent incidence and mortality rates, because of its aggressive growth and early metastatic dissemination (Hruban et al, 2010). PDC has a characteristically desmoplastic stroma and immune/inflammatory infiltrates. The development of predictive biomarkers to assist selection of patient subsets is useful for studies aimed at reducing the mortality of PDC patients, especially clinical studies designed to evaluate various therapeutic approaches (Philip et al, 2009).
The aim of this study was to examine whether tumour-infiltrating immune/inflammatory cells represent actual conditions of the immune microenvironment by analysing their clinicopathological impact. We then performed immunohistochemistry to detect tumour-infiltrating M1 and M2, neutrophils (Neu), CD4+ T cells (CD4+T), CD8+ T cells (CD8+T), and FOXP3+CD4+ Treg using 212 cases of PDC and examined their clinicopathological influences. Furthermore, we investigated the prognostic significance of combinations of these tumour-infiltrating immune/inflammatory cells as indicators of the immune microenvironment.
Materials and Methods
Patients and samples
This study was approved by the Ethics Committee of the National Cancer Center, Japan. Informed consent was obtained from all participants involved in this study and all clinical investigation was conducted according to the principles expressed in the Declaration of Helsinki. Clinical and pathological data were obtained through a detailed retrospective review of the medical records of all 212 patients with PDC who had undergone initial surgical resection between 1990 and 2005 at the National Cancer Center Hospital, Japan. The patients enrolled in the study were those for whom sufficient immunohistochemical analyses were available. None of the patients had received any therapy before surgery. The operative procedures included 149 classical pancreatoduodenectomies or pylorus-preserving pancreatoduodenectomies, 56 distal pancreatectomies, and 7 total pancreatectomies. All the patients included in this study underwent macroscopic curative resection. All of the cases were conventional ductal carcinomas and intraductal papillary-mucinous neoplasm-related cancers, secondary tumours, and post-neoadjuvant cases were excluded. The clinicopathological characteristics of the patients are summarised in Supplementary Table 1. All M1 patients had nodal metastasis around the abdominal aorta, without any other form of metastasis. The median follow-up period after surgery for the patients as a whole and for the living patients were 18.8 (2.6–201) and 54.5 (2.6–201) months, respectively. Every patient was followed up in the outpatient clinic every 1–3 months during the first postoperative year, and every 6–12 months thereafter. Patients underwent physical examination, laboratory tests, chest radiography, abdominal computed tomography, and/or ultrasonography, unless there was a confirmed relapse. The tumour markers carcinoembryonic antigen and carbohydrate antigen 19–9 were also measured until relapse. Recurrence was suspected when a new local or distant metastatic lesion was found on serial images and an increase in tumour marker levels was recognised. When progression of the disease was confirmed by repeated imaging studies, the date of the first suspicious radiologic finding was used as the date of initial disease recurrence. At the census date (June 2009), we checked whether all our patients were dead or alive from our medical records and family registers administered by the Japanese government, 49 patients (23.1%) were alive, 141 (66.5%) had died of pancreatic cancer, and 22 (10.3%) had died of other causes. Information on post-resection adjuvant therapy was available for 206 patients, of whom 8 received chemotherapy and radiotherapy, 84 chemotherapy only, and 2 radiotherapy only; 112 patients did not receive any post-resection therapy.
Pathological examination
All of the cases were pathologically reexamined and classified according to the World Health Organization classification (Hruban et al, 2010). the International Union Against Cancer tumour-node-metastasis classification (Sobin et al, 2009), and the Classification of Pancreatic Carcinoma of the Japan Pancreas Society (Japan Pancreas Society, 2011). Tumour necrosis was judged according to the definition reported previously (Hiraoka et al, 2010).
Immunohistochemistry
Immunohistochemistry was performed on the formalin-fixed, paraffin-embedded tissue sections using the avidin–biotin complex method as described previously (Hiraoka et al, 2006). We used 4-μm-thick sections of representative blocks with antibodies listed in Supplementary Table 2.
Quantitative evaluation of tumour-infiltrating immune/inflammatory cells
After immunohistochemistry, the microscopic images were imported as digital photo files using a NanoZoomer Digital Pathology (NDP) system (Hamamatsu Photonics, Hamamatsu, Japan), and we selected three areas at low magnification in which the immunolabeled cells had infiltrated into the tumour most densely (Supplementary Figure 1). The selected areas were those in which it had been confirmed at high magnification that invasive proliferation of cancer cells was present. We did not select areas into which infiltrated immune/inflammatory cells had been recruited as a result of secondary tumour effects, such as pancreatitis, necrosis, ulceration, or mucus flooding of the tissue. Using NDP view at a magnification of × 200, immunolabeled lymphocytes, neutrophils (except intravascular neutrophils), or macrophages were then counted by two independent investigators (YI and NH). These observers were blinded to each other and also not provided with any clinical information on the outcome of the patients. The average counts for each of the three areas made by the two observers were then compared, and when the difference between their counts was <20% of the maximum value, the average of the two was used as the final count; if the difference exceeded 20%, the observers discussed the reasons for the difference and performed recounts until the difference became <20%. For the survival and correlation analyses, patients were divided into two groups showing high and low cell infiltration, representing values higher and lower than the median for tumour-infiltrating immune/inflammatory cells.
Statistical analysis
Comparisons of variables were performed using Fisher’s exact test based on their categorical data (Table 1). The postoperative proportion of overall survival (OS) and disease-free survival (DFS) was calculated by the Kaplan–Meier method. Univariate analysis was performed for prognostic factors using the log-rank test. The factors found to be significant by univariate analysis were subjected to multivariate analysis using the Cox proportional hazards model (backward elimination method). For examining combinations of variables and performing Kaplan–Meier analysis, patients were divided into four groups based on combinations of two groups of two factors (i.e., XhighYhigh, XhighYlow, XlowYhigh, and XlowYlow). The profiles of the resulting Kaplan–Meier curves were divisible into two types, which we termed type A and type B; type A was the pattern associated with the longest surviving group with a combination of both conditions for whom longer survival was expected from their individual factors, one shortest survival group with a combination of both conditions for whom shorter survival was expected from their individual factors, and an intermediate survival group with combinations of conditions other than the previous two groups; in type B, there was one longest (or shortest) survival group, and the other three groups showed similar survival curves. Differences at P<0.05 were considered statistically significant. Statistical analyses were performed with StatView-J 5.0 software (Abacus Concepts, Berkeley, CA, USA).
Results
Tumour-infiltrating immune/inflammatory cells
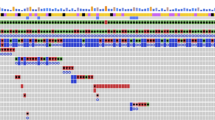
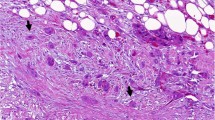
We used the following antigens as markers for detecting each of the cell types: CD68 for pan-macrophages, CD163 or CD204 for M2, CD66b for Neu, CD4, CD8, and FOXP3+CD4+ (Treg) for subsets of T cells. M1 were detected as HLA-DR+CD68+ cells (Figure 1). In 78% of the cases, M2 were predominant among tumour-infiltrating macrophages. In contrast, M1 infiltrated chronic pancreatitis (non-cancerous pancreas) predominantly. The majority of the macrophages that had infiltrated into areas of necrosis were M2. The density of tumour-infiltrating macrophages, CD4+T, and CD8+T was higher near the invasive front of the tumour, and that of T cells was lower at the centre of the tumour. Preliminary tests revealed that rather than the absolute numbers of infiltrating cells, it would be better if we used the ratio of FOXP3+CD4+ T cells to CD4+T (%Treg) and the ratio of M1 to pan-macrophages (%M1) as variables, as they were more representative of the biological characteristics of the respective infiltrating cells. Comparison of immune/inflammatory cells infiltrating into normal pancreas, chronic pancreatitis (non-cancerous pancreas), and PDC is shown in Figure 1I.
Immunohistochemical features of tumour-infiltrating immune/inflammatory cells. The representative photos are shown: (A) CD8+ T cells, (B) CD4+ T cells, (C) FOXP3+ T cells, (D) CD68+ pan-macrophages, (E) CD163+ M2 macrophages, (F) CD204+ M2 macrophages, (G) CD66b+ neutrophils, and (H) CD68+HLA-DR+ M1 macrophages (CD68 in brown and HLA-DR in purple). Scale bars show 10 μm in length. A comparison of infiltrating immune/inflammatory cells into normal pancreas, chronic pancreatitis (non-cancerous pancreas, and PDC is shown in I. Columns and bars show mean (n=20) and standard error, respectively. Significance values were *P<0.05 and **P<0.01.
Interrelationships between clinicopathological variables
We analysed the interrelationships among clinicopathological variables of PDC containing tumour-infiltrating immune/inflammatory cells (Table 1). Tumour-infiltrating pan-macrophages, CD163+ M2, CD204+ M2, and Neu, showed close correlations with each other. All of them showed significant and negative correlations with %M1. Tumour-infiltrating CD4+T and CD8+T showed a significant positive correlation with each other, but no significant correlation was evident between tumour-infiltrating myeloid cells and tumour-infiltrating CD4+T or CD8+T. In contrast, tumour-infiltrating %Treg were closely correlated with tumour-infiltrating macrophages, Neu, and CD4+T. Most of the conventional clinicopathological variables did not demonstrate a close correlation with tumour-infiltrating immune/inflammatory cells. The presence of tumour necrosis was significantly correlated with all types of tumour-infiltrating immune/inflammatory cells. The presence of venous invasion was closely correlated with tumour-infiltrating pan-macrophages, CD204+ M2, and %Treg.
Prognostic impact of individual tumour-infiltrating immune/inflammatory cells
Kaplan–Meier survival analyses revealed that higher numbers of tumour-infiltrating pan-macrophages, CD163+ or CD204+ M2, and Neu, and lower %M1 were significantly associated with both shorter OS and DFS in PDC patients (Figure 2 and Supplementary Figure 2). More marked infiltration of CD4+T or CD8+T into tumour tissues was significantly associated with both longer OS and DFS, whereas higher %Treg was closely associated with both shorter OS and DFS (Figure 2 and Supplementary Figure 2).
Kaplan–Meier survival curves showing comparison of overall survival between high (orange) and low (blue) infiltration (inf.) of immune/inflammatory cells. P-values obtained from log-rank test. The ‘x’ and ‘+’ represent censoring and failure, respectively. The proportions of 5-year survival with 95% confidence intervals (in parentheses) are shown. *Ratio of CD68+HLA-DR+ M1 macrophages to CD68+ pan-macrophages, **ratio of FOXP3+CD4+ Tregs to CD4+ T cells.
When each of the parameters of tumour-infiltrating immune/inflammatory cells was subjected to Cox regression multivariate analysis, together with the conventional clinicopathological variables that had been found to be significant by univariate analysis (Supplementary Tables 3 and 4), all of the tumour-infiltrating immune/inflammatory cells were found to be independent predictors of OS and DFS (data not shown). Tumour-infiltrating CD163+ and CD204+ M2 showed comparable results, and we adopted CD163+ macrophages as M2 thereafter.
Prognostic impact of combinations of tumour-infiltrating immune/inflammatory cells
To clarify more precisely the characteristics of tumour-infiltrating immune/inflammatory cells in the immune microenvironment, we then examined various combinations of tumour-infiltrating immune/inflammatory cells and performed Kaplan–Meier analysis (see Materials and Methods, Figure 3). Most of the combinations were found to be type A, as expected. However, four combinations (tumour-infiltrating CD4+T and CD8+T, tumour-infiltrating CD4+T and %Treg, tumour-infiltrating CD8+T and %Treg, and tumour-infiltrating %M1 and M2) showed type B. For the combination of tumour-infiltrating CD4+T and CD8+T, only the group with higher numbers of tumour-infiltrating CD4+T (CD4+Thigh) and higher numbers of tumour-infiltrating CD8+T (CD8+Thigh) showed long survival, and the other three groups showed similar degrees of shorter survival even if the number of either CD4+T or CD8+T was higher. Similarly, the group with CD4+Thigh and lower numbers of tumour-infiltrating %Treg (%Treglow) in the combination of tumour-infiltrating CD4+T and %Treg, the group with CD8+Thigh and %Treglow in the combination of tumour-infiltrating CD8+T and %Treg, and the group with higher numbers of tumour-infiltrating %M1 (%M1high) and lower numbers of tumour-infiltrating M2 (M2low) in the combination of tumour-infiltrating %M1 and M2 were the only group that showed long survival, whereas the other three groups in each of the combinations showed similar degrees of shorter survival. These results indicated that specific groups with long survival could be detected more precisely by combination of variables. In addition to the combination of CD4+Thigh and CD8+Thigh, a lower tumour-infiltrating %Treg (%Treglow) was important for a close association with longer survival. In fact, one group with CD4+Thigh, CD8+Thigh, and %Treglow showed exclusively long survival (Supplementary Figure 3).
Kaplan–Meier survival curves showing comparison of overall survival among four groups of patients divided on the basis of combinations of two variables with high and low infiltration of immune/inflammatory cells. A and B are representative profiles. The four groups are 1st variablehigh and 2nd variablehigh in blue, 1st variablehigh and 2nd variablelow in pink, 1st variablelow and 2nd variablehigh in red, and 1st variablelow and 2nd variablelow in green. The ‘x’ and ‘circle’ represent censoring and failure, respectively.
To represent the effects of tumour-infiltrating immune/inflammatory cells more precisely, we then connected these factors to make two new variables: tumour-infiltrating CD4+Thigh/CD8+Thigh/%Treglow and tumour-infiltrating %M1high/M2low. Multivariate analysis together with conventional clinicopathological variables that had been found to be significant by univariate analysis revealed that these two variables were independently prognostic for OS and DFS with higher hazard ratio values (Table 2 and Supplementary Table 4).
Discussion
Host immune responses to tumour cells are represented by the features of tumour-infiltrating immune/inflammatory cells (Dunn et al, 2004; Sica and Bronte, 2007; Biswas and Mantovani, 2010; Ferrone and Dranoff, 2010; Grivennikov et al, 2010; Hiraoka et al, 2011). We investigated the profiles of tumour-infiltrating immune/inflammatory cells using over 200 cases of PDC that had been surgically resected in one hospital. We found that tumour-infiltrating pan-macrophages, CD163+ or CD204+ M2, and Neu had positive correlations with each other, and that all of them were negatively correlated with tumour-infiltrating %M1 (Table 1). Tumour-infiltrating CD4+T and CD8+T showed a positive correlation with tumour-infiltrating CD8+T and a negative correlation with tumour-infiltrating %Treg (Table 1). No significant correlation was found between tumour-infiltrating myeloid cells and T cells, except for the close correlation between tumour-infiltrating myeloid cells and %Treg. These findings suggest that tumour-infiltrating myeloid cells and T cells are regulated independently, and that infiltration by each subset of myeloid cells or Treg is closely interrelated. Univariate and multivariate survival analyses revealed that tumour-infiltrating CD4+T, CD8+T, and %M1 were independently prognostic of OS and DFS and that tumour-infiltrating pan-macrophages, M2, Neu, and %Treg were independent prognosticators of poor OS and DFS. When pairs of these six variables (%M1, M2, Neu, CD4+T, CD8+T, and %Treg) were combined and subjected to survival analyses, the four combinations (CD4+T and CD8+T, CD4+T and %Treg, CD8+T and %Treg, and %M1 and M2) showed that only one specific patient group (CD4+Thigh and CD8+Thigh, CD4+Thigh and %Treglow, CD8+Thigh and %Treglow, and %M1high and M2low) had longer survival, whereas the other three groups had shorter survival with similar degrees. These results suggest that systematic analysis of several tumour-infiltrating immune/inflammatory cells is important for providing the findings of effects of specific cell combination in immune microenvironment more precisely. The factors involved in these combinations were then connected, and two new variables emerged: tumour-infiltrating CD4+Thigh/CD8+Thigh/%Treglow and %M1high/M2low. These corrected for the unbalanced patient distribution, and represented the effects of the immune-related factors more precisely. In fact, multivariate survival analyses showed that these two variables were independent prognosticators of OS and DFS with higher hazard ratio values than those of individual sets of tumour-infiltrating cells (Table 2). Therefore, tumour-infiltrating CD4+Thigh/CD8+Thigh/%Treglow and tumour-infiltrating %M1high/M2low are suitable variables for evaluating the immune microenvironment of PDC.
Various types of myeloid cells affect the immune microenvironment. Though some studies have obtained opposite results (Forssell et al, 2007), several studies have reported that a high amount of tumour-infiltrating macrophages is correlated with a poor outcome in various cancers (Komohara et al, 2008; Shabo et al, 2008) containing pancreas cancer (Kurahara et al, 2011). We speculated that this discrepancy in previous results might have been attributable to the fact that most of these studies had measured tumour-infiltrating macrophages as pan-macrophages and/or M2, and not M1 independently. M1 have strong tumoricidal activity, being opposite to the effect of M2. Tumour-infiltrating macrophages were predominantly M2, whereas M1 was predominant macrophage in the non-cancerous inflammatory region surrounding the area of cancer cell infiltrates. Therefore, analysis of tumour-infiltrating M1 and M2, as well as their locations, separately is important for assessing the infiltration of macrophages.
Recently, a study using mice demonstrated that tumour-associated Neu were polarised into two types: the N1 antitumour phenotype and the N2 protumour phenotype, similar to the M1 and M2 macrophages (Fridlender et al, 2009). In humans, tumour-infiltrating Neu were significantly correlated with shorter survival in renal cell carcinoma (Wislez et al, 2003; Jensen et al, 2009) and significantly correlated with longer survival in gastric carcinoma (Caruso et al, 2002). We have found that almost all tumour-infiltrating Neu in PDC express arginase 1 (Ino and Hiraoka, unpublished data), which hydrolyses arginine to ornithine and urea, resulting in a reduction of arginine in the tumour microenvironment. It has been reported that adequate levels of arginine in the extracellular milieu are crucial for T-cell proliferation and activity, and that reduction of arginine suppresses T-cell responses (Rodriguez et al, 2004; Rodriguez and Ochoa, 2008). These results, combined with findings that higher levels of tumour-infiltrating Neu are significantly correlated with shorter survival of patients, suggest that tumour-infiltrating Neu act as a pro-tumour factor. Therefore, it is suggested that N2 cells are the predominant infiltrating type in PDC, although currently there are no markers for distinguishing the two human Neu phenotypes, N1 and N2.
MDSCs represent a heterogeneous population of cells that comprise myeloid progenitor cells and immature myeloid cells and have immune suppressor function (Gabrilovich and Nagaraj, 2009). In contrast to extensive studies of murine MDSCs, the corresponding cells in humans have been inadequately characterised because of the lack of uniform markers. Human MDSCs have a common Lin−/lowHLA-DR−/lowCD11b+CD33+ phenotype and comprise two subsets: a CD14+ monocytic subpopulation (Mo-MDSCs) and a CD15+ granulocytic subpopulation (G-MDSCs) (Filipazzi et al, 2012). G-MDSCs have a Neu-like polymorphonuclear morphology and also express CD66b. G-MDSCs may have been included in the Neu counts in our present study. Although MDSCs were not identified directly in our study, tumour-infiltrating myeloid cells were closely correlated both with each other, and also with %Treg. These findings, together with a recent report by Corzo et al (2010) indicating that hypoxia causes MDSCs to differentiate rapidly into tumour-associated macrophages, suggest that tumour-infiltrating MDSCs have a positive correlation with tumour-infiltrating M2 and Neu, and a negative correlation with %M1. Thus, our evaluation system using %M1high/M2low might also cover tumour-infiltrating MDSCs.
In our study both tumour-infiltrating CD4+T and CD8+T were independent prognostic factors, however, the detailed analysis indicated that infiltration of the tumour by CD4+T or CD8+T alone was not sufficiently associated with longer survival, and that infiltration by higher numbers of both CD4+T and CD8+T was prerequisite for longer survival. This result was similar to that of a previous study that included a smaller number of cases (Fukunaga et al, 2004). It was also reported that De Monte et al (2011) found that Th2 rather than Th1 cells predominantly infiltrated in PDC, and that the ratio of tumour-infiltrating Th2/Th1 cells was independently predictive of patient survival. These findings together with our present results suggest that CD4+Thigh/CD8+Thigh is the hallmark of an immune microenvironment where a strong Th1 response might be present.
In conclusion, tumour-infiltrating CD4+Thigh/CD8+Thigh/%Treglow and tumour-infiltrating %M1high/M2low were independent prognosticators with a higher hazard ratio. Therefore, these variables appear to be suitable for monitoring the immune microenvironment of PDC, and we are now planning to use them for this purpose, with a view to devising some more effective form of immunotherapy.
Change history
05 March 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Biswas SK, Mantovani A (2010) Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat Immunol 11: 889–896
Caruso RA, Bellocco R, Pagano M, Bertoli G, Rigoli L, Inferrera C (2002) Prognostic value of intratumoral neutrophils in advanced gastric carcinoma in a high-risk area in northern Italy. Mod Pathol 15: 831–837
Center for Cancer Control and Information Services, National Cancer Center (2009) Cancer Statistics in Japan. Center for Cancer Control and Information Services, National Cancer Center, Tokyo, Japan
Corzo CA, Condamine T, Lu L, Cotter MJ, Youn JI, Cheng P, Cho HI, Celis E, Quiceno DG, Padhya T, McCaffrey TV, McCaffrey JC, Gabrilovich DI (2010) HIF-1alpha regulates function and differentiation of myeloid-derived suppressor cells in the tumor microenvironment. J Exp Med 207: 2439–2453
De Monte L, Reni M, Tassi E, Clavenna D, Papa I, Recalde H, Braga M, Di Carlo V, Doglioni C, Protti MP (2011) Intratumor T helper type 2 cell infiltrate correlates with cancer-associated fibroblast thymic stromal lymphopoietin production and reduced survival in pancreatic cancer. J Exp Med 208: 469–478
Dunn GP, Old LJ, Schreiber RD (2004) The three Es of cancer immunoediting. Annu Rev Immunol 22: 329–360
Ferrone C, Dranoff G (2010) Dual roles for immunity in gastrointestinal cancers. J Clin Oncol 28: 4045–4051
Filipazzi P, Huber V, Rivoltini L (2012) Phenotype, function and clinical implications of myeloid-derived suppressor cells in cancer patients. Cancer Immunol Immunother 61: 255–263
Forssell J, Oberg A, Henriksson ML, Stenling R, Jung A, Palmqvist R (2007) High macrophage infiltration along the tumor front correlates with improved survival in colon cancer. Clin Cancer Res 13: 1472–1479
Fridlender ZG, Sun J, Kim S, Kapoor V, Cheng G, Ling L, Worthen GS, Albelda SM (2009) Polarization of tumor-associated neutrophil phenotype by TGF-beta: ‘N1’ vs ‘N2’ TAN. Cancer Cell 16: 183–194
Fukunaga A, Miyamoto M, Cho Y, Murakami S, Kawarada Y, Oshikiri T, Kato K, Kurokawa T, Suzuoki M, Nakakubo Y, Hiraoka K, Itoh T, Morikawa T, Okushiba S, Kondo S, Katoh H (2004) CD8+ tumor-infiltrating lymphocytes together with CD4+ tumor-infiltrating lymphocytes and dendritic cells improve the prognosis of patients with pancreatic adenocarcinoma. Pancreas 28: e26–e31
Gabrilovich DI, Nagaraj S (2009) Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol 9: 162–174
Grivennikov SI, Greten FR, Karin M (2010) Immunity, inflammation, and cancer. Cell 140: 883–899
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144: 646–674
Hiraoka N, Ino Y, Sekine S, Tsuda H, Shimada K, Kosuge T, Zavada J, Yoshida M, Yamada K, Koyama T, Kanai Y (2010) Tumour necrosis is a postoperative prognostic marker for pancreatic cancer patients with a high interobserver reproducibility in histological evaluation. Br J Cancer 103: 1057–1065
Hiraoka N, Onozato K, Kosuge T, Hirohashi S, Hiraoka N, Onozato K, Kosuge T, Hirohashi S (2006) Prevalence of FOXP3+ regulatory T cells increases during the progression of pancreatic ductal adenocarcinoma and its premalignant lesions. Clin Cancer Res 12: 5423–5434
Hiraoka N, Yamazaki-Itoh R, Ino Y, Mizuguchi Y, Yamada T, Hirohashi S, Kanai Y (2011) CXCL17 and ICAM2 are associated with a potential anti-tumor immune response in early intraepithelial stages of human pancreatic carcinogenesis. Gastroenterology 140: 310–321
Hruban RH, Boffetta P, Hiraoka N, Iacobuzio-Donahue C, Kato Y, Kern SE, Klimstra DS, Kloppel G, Maitra A, Offerhaus GJA, Pitman MB (2010) Ductal adenocarcinoma of the pancreas. In World Health Organization Classification of Tumours. Pathology & Genetics. Tumours of the Digestive System Bosman FT, Carneiro F, Hruban RH, Theise ND, (eds) 4th edn pp 281–291. IARC Press: Lyon, France
Japan Pancreas Society (2011) Classification of Pancreatic Cancer 3rd English edn, Kanehara: Tokyo, Japan
Jensen HK, Donskov F, Marcussen N, Nordsmark M, Lundbeck F, von der Maase H (2009) Presence of intratumoral neutrophils is an independent prognostic factor in localized renal cell carcinoma. J Clin Oncol 27: 4709–4717
Komohara Y, Ohnishi K, Kuratsu J, Takeya M (2008) Possible involvement of the M2 anti-inflammatory macrophage phenotype in growth of human gliomas. J Pathol 216: 15–24
Kurahara H, Shinchi H, Mataki Y, Maemura K, Noma H, Kubo F, Sakoda M, Ueno S, Natsugoe S, Takao S (2011) Significance of M2-polarized tumor-associated macrophage in pancreatic cancer. J Surg Res 167: e211–e219
Mantovani A, Sozzani S, Locati M, Allavena P, Sica A (2002) Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol 23: 549–555
Mosser DM, Edwards JP (2008) Exploring the full spectrum of macrophage activation. Nat Rev Immunol 8: 958–969
Pages F, Berger A, Camus M, Sanchez-Cabo F, Costes A, Molidor R, Mlecnik B, Kirilovsky A, Nilsson M, Damotte D, Meatchi T, Bruneval P, Cugnenc PH, Trajanoski Z, Fridman WH, Galon J (2005) Effector memory T cells, early metastasis, and survival in colorectal cancer. N Engl J Med 353: 2654–2666
Philip PA, Mooney M, Jaffe D, Eckhardt G, Moore M, Meropol N, Emens L, O'Reilly E, Korc M, Ellis L, Benedetti J, Rothenberg M, Willett C, Tempero M, Lowy A, Abbruzzese J, Simeone D, Hingorani S, Berlin J, Tepper J (2009) Consensus report of the national cancer institute clinical trials planning meeting on pancreas cancer treatment. J Clin Oncol 27: 5660–5669
Rodriguez PC, Ochoa AC (2008) Arginine regulation by myeloid derived suppressor cells and tolerance in cancer: mechanisms and therapeutic perspectives. Immunol Rev 222: 180–191
Rodriguez PC, Quiceno DG, Zabaleta J, Ortiz B, Zea AH, Piazuelo MB, Delgado A, Correa P, Brayer J, Sotomayor EM, Antonia S, Ochoa JB, Ochoa AC (2004) Arginase I production in the tumor microenvironment by mature myeloid cells inhibits T-cell receptor expression and antigen-specific T-cell responses. Cancer Res 64: 5839–5849
Shabo I, Stal O, Olsson H, Dore S, Svanvik J (2008) Breast cancer expression of CD163, a macrophage scavenger receptor, is related to early distant recurrence and reduced patient survival. Int J Cancer 123: 780–786
Sica A, Bronte V (2007) Altered macrophage differentiation and immune dysfunction in tumor development. J Clin Invest 117: 1155–1166
Sica A, Mantovani A (2012) Macrophage plasticity and polarization: in vivo veritas. J Clin Invest 122: 787–795
Siegel R, Ward E, Brawley O, Jemal A (2011) Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin 61: 212–236
Sobin LH, Gospodarowicz MK, Wittekind C (2009) UICC TNM Atlas 7th edn, Wiley-Blackwell: Hoboken, NJ, USA
Wislez M, Rabbe N, Marchal J, Milleron B, Crestani B, Mayaud C, Antoine M, Soler P, Cadranel J (2003) Hepatocyte growth factor production by neutrophils infiltrating bronchioloalveolar subtype pulmonary adenocarcinoma: role in tumour progression and death. Cancer Res 63: 1405–1412
Zhang L, Conejo-Garcia JR, Katsaros D, Gimotty PA, Massobrio M, Regnani G, Makrigiannakis A, Gray H, Schlienger K, Liebman MN, Rubin SC, Coukos G (2003) Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. N Engl J Med 348: 203–213
Acknowledgements
This work was supported by a Grant-in-Aid for Third Term Comprehensive 10-year Strategy for Cancer Control from the Ministry of Health, Labor and Welfare of Japan (NH), Princess Takamatsu Cancer Research Fund (10-24216) (NH), Pancreas Research Foundation of Japan (NH), and the National Cancer Center Research and Development Fund (NH). We thank Drs Kazufumi Honda, Tomohiro Sakuma, and Kimio Yoshimura for kindly advising statistical analyses and Drs Hidenori Ojima, Minoru Esaki, Satoshi Nara, and Yoji Kishi for useful discussion.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Ino, Y., Yamazaki-Itoh, R., Shimada, K. et al. Immune cell infiltration as an indicator of the immune microenvironment of pancreatic cancer. Br J Cancer 108, 914–923 (2013). https://doi.org/10.1038/bjc.2013.32
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.32
Keywords
This article is cited by
-
Identification and verification of PTPN3 as a novel biomarker in predicting cancer prognosis, immunity, and immunotherapeutic efficacy
European Journal of Medical Research (2024)
-
PCDH8 is a novel prognostic biomarker in thyroid cancer and promotes cell proliferation and viability
Functional & Integrative Genomics (2024)
-
Construction of a novel signature based on immune-related lncRNA to identify high and low risk pancreatic adenocarcinoma patients
BMC Gastroenterology (2023)
-
Immune landscape and prognostic index for pancreatic cancer based on TCGA database and in vivo validation
BMC Cancer (2023)
-
Molecular subtypes based on cuproptosis-related genes and tumor microenvironment infiltration characteristics in pancreatic adenocarcinoma
Cancer Cell International (2023)