Abstract
Background:
The increasing prevalence of diabetes may contribute to the rising incidence of hepatocellular carcinoma (HCC) in the US and other developed countries where HCC incidence is relatively low. Data from prospective studies on diabetes and risk of HCC in at-risk populations due to high prevalence of viral hepatitis in southeast Asia are sparse.
Methods:
The Singapore Chinese Health Study is a prospective cohort of 63 257 middle-aged and older Chinese men and women enrolled in 1993–1998. Besides an in-person interview administered to all participants at baseline, testing of serologic markers of hepatitis B or C infections were performed on a subset of cohort subjects. After a mean follow-up of 14 years, 499 cohort participants developed HCC.
Results:
A history of diabetes at baseline was associated with a hazard ratio of 2.14 (95% confidence interval, 1.69–2.71). This statistically significant association was comparable in magnitude between men and women, and remained equally strong across strata of subjects defined by the number of years between their first clinical diagnosis of diabetes and time of enrolment in this cohort. Within a nested case-control set of cohort subjects tested for serological markers of hepatitis B or C infections, the diabetes–HCC association was found to be present mainly among those devoid of any markers.
Conclusion:
A history of diabetes at baseline is highly associated with non-viral HCC. Future studies are warranted to elucidate the biological mechanism underpinning the role of diabetes in nonviral-related hepatocarcinogenesis.
Similar content being viewed by others
Main
Diabetes mellitus is a major cause of morbidity and mortality worldwide, and the influence of this metabolic disease on the overall health of populations is expected to increase as the overall prevalence of diabetes increases in both developed and developing countries. According to data by the International Diabetes Federation that tracks diabetes prevalence worldwide, the expected prevalence of diabetes is expected to increase from 6.6–7.8% by 2030, with the total number of patients living with diabetes expected to rise from 285 million to 438 million over that time span (Federation, 2009). Besides cardiovascular disease (Bjornholt et al, 1999), kidney disease (Foundation, 2002) and blindness (Tapp et al, 2003), diabetes has been associated with an increased risk of cancer including that of the pancreas (Huxley et al, 2005), endometrium (Friberg et al, 2007), colon/rectum (Larsson et al, 2005), bladder (Larsson et al, 2006) and breast (Larsson et al, 2007).
The association between diabetes and hepatocellular carcinoma (HCC) has been investigated for several decades in epidemiological studies. We first reported a positive association between history of diabetes and risk of HCC in a non-Asian population in Los Angeles County, California in 1991 (Yu et al, 1991). This association was confirmed in our later analysis with a larger study sample size (Yuan et al, 2004). Similar findings were reported in other populations in the US (Atchison et al, 2011; Coughlin et al, 2004; El-Serag et al, 2004), Japan (Fujino et al, 2001; Tazawa et al, 2002; Ohata et al, 2003; Shibata et al, 2003; Inoue et al, 2006), Taiwan (Lai et al, 2006; Wang et al, 2009; Lai et al, 2012) and in western Europe (Adami et al, 1996; Wideroff et al, 1997; Veldt et al, 2008; Ogunleye et al, 2009). The rising prevalence of obesity and diabetes could be one of the reasons contributing to the increasing incidence of HCC in the United States in the past three decades (El-Serag et al, 2003). Given the growing prevalence of obesity and diabetes in developing or recently developed countries where hepatitis B or C infections are endemic (Kelly et al, 2008), the establishment of a direct relationship between diabetes and HCC risk in such high-risk populations bears important public health implications.
In the present study, using a population-based prospective cohort, we evaluated the association between diabetes and HCC in Singaporean Chinese, a population with relatively high prevalence of hepatitis B infection and who are at relatively high risk of HCC (Koh et al, 2011). The cohort’s extensive period of follow-up (average of 14 years per participant) allows us to meaningfully examine the temporality of the diabetes–HCC association. The high prevalence of viral hepatitis in this target population also allows for a meaningful evaluation of the potential modifying role of viral hepatitis on the diabetes–HCC association.
Materials and methods
Study population
The Singapore Chinese Health Study is a population-based prospective cohort established between April 1993 and December 1998 through the recruitment of 63 257 Chinese men (n=27 959) and women (n=35 298), who were aged 45–74 years and residing in public housing estates, where 86% of Singapore resided at that time (Hankin et al, 2001). All participants belonged to one of the two major Chinese dialect groups in Singapore, the Hokkiens or the Cantonese, who originated from two contiguous prefectures in southern China. The study was approved by the Institutional Review Boards of the various sponsoring institutions in the US and Singapore.
Baseline exposure assessment
At recruitment, an in-person interview was conducted in the subject’s home by a trained interviewer using a structured questionnaire that covered demographics, lifetime use of tobacco, current physical activity, menstrual/reproductive history (for women), occupational exposure, medical history and family history of cancer. The subjects were asked if they had a history of physician-diagnosed diabetes mellitus (fasting plasma glucose level ⩾126 mg dl−1); positive subjects were then asked for their ages at the time of diagnosis. Using standard protocols, a separate study of 1651 cohort subjects who self-reported a history of physician-diagnosed diabetes mellitus at baseline (Odegaard et al, 2008) has validated the accuracy (at 98.8%) of the self-reported diabetes in this cohort.
Between April 1994 and December 1999, blood and single-void urine specimens were collected from a random 3% sample of study enrollees (Koh et al, 2003). Starting in January 2000, the biospecimen collection was extended to all surviving cohort members. By April 2005, when all subjects had been contacted, biospecimens were collected from 32 543 participants, representing a ∼60% consent rate. Various components (plasma, red blood cell, serum and white blood cell) of blood were separated and have been stored continuously at −80 °C.
Case ascertainment
Incident cases of cancers and deaths among cohort members were identified through linkage of the cohort master files with databases of the population-based Singapore Cancer Registry and Singapore Registry of Births and Deaths. The nationwide cancer registry has been in place since 1968 and has been shown to be comprehensive in its recording of incident cancer cases (Parkin et al, 2002). As of December 31, 2010, 47 cohort subjects were lost to follow-up, mainly due to migration out of Singapore, and 499 cohort participants who were free of cancer at baseline had developed primary liver cancer. Among them, 18 (3.7%) were diagnosed with intrahepatic bile carcinoma or sarcomas. For 362 HCC cases diagnosed before December 31, 2006, their diagnoses were confirmed via manual review of pathology reports by a medically trained research staff. Among these HCC cases, 31.5% (114 cases) were diagnosed histologically, 65.0% (235 cases) were diagnosed on the basis of elevation in serum α-fetoprotin in conjunction with clinical and radiologic evidence consistent with HCC, and 3.5% (13 cases) were identified through death certificates.
Hepatitis B and C serology
Beginning in April 1994, a random 3% sample of cohort participants were asked to provide blood or buccal cells, and spot urine samples. Eligibility for this biospecimen subcohort was extended to all surviving cohort participants starting in January 2000. By April 2005, all surviving cohort subjects had been contacted for biospecimen donation. Samples were obtained from 32 535 subjects, representing a consent rate of about 60%.
We conducted a nested case-control study within the biospecimen subcohort for serological biomarkers of hepatitis B and C infection. All incident HCC cases with a baseline blood sample and the diagnosis of HCC before December 31, 2006 were eligible for this nested case-control study. Ninety-two HCC cases met these study criteria (Koh et al, 2011). For each case, three control subjects individually matched to the index case by gender, dialect group (Hokkien, Cantonese), age at enrolment (±2 years), date of baseline interview (±6 months) were randomly selected from the biospecimen subcohort who were alive and free of cancer on the date of cancer diagnosis of the index case. We assayed serological markers of hepatitis B virus (HBV) and hepatitis C virus (HCV) infections in baseline serum samples of 92 HCC cases and 274 matched control subjects. Briefly, we tested for the presence of HBsAg (Ausria, Abbott Laboratories, North Chicago, IL, USA), and negative samples were further tested for the presence of anti-HBc and anti-HBs (Corab and Ausab, Abbott Laboratories, North Chicago, IL, USA, respectively). All baseline serum samples also were tested for the presence of anti-HCV using the ELISA version 2.0 kit manufactured by Ortho Diagnostic Systems (Ortho, Raritan, NJ, USA), with confirmation of positive samples using RIBA version 2.0 (Chiron, Emeryville, CA, USA).
Statistical analysis
We excluded 1936 individuals with a history of invasive cancer (except non-melanoma skin cancer) at baseline interview. The present analysis included 61 321 cohort subjects. The distributions of demographic and lifestyle factors were compared between diabetics and non-diabetics, and between HCC cases and non-cases. We used the χ2 test for categorical variables, and the t-test or the analysis of variance method for continuous variables.
For each subject, person-year of follow-up was counted from the date of enrolment to the date of diagnosis of HCC, being lost to follow-up, death, or 31 December 2010, whichever occurred first. Proportional hazards (Cox) regression was used to evaluate the associations between diabetes status and the risk of developing HCC. The strength of the association was measured by the hazard ratio (HR) and its 95% confidence interval (CI) and P-value. All Cox regression models have the following covariates: age at recruitment (years), gender, year of cohort enrolment, dialect group (Hokkien, Cantonese), body mass index (BMI) (kg m−2), level of education (no formal schooling, primary school, secondary school or higher), cigarette smoking status (never, former or current smoker), consumption of alcoholic beverages (non-drinker, <7 or 7+ drinks per week), frequency of black tea or green tea consumption (none, monthly, weekly or daily) and coffee consumption (number of cups per week) (Johnson et al, 2011).
Using the nested case-control set of cohort subjects with HBV/HCV serology measurements, we first examined the relationships between markers of HBV and HCV infections and HCC risk using conditional logistic regression methods. We then examined the diabetes–HCC association stratified by the subjects’ status on viral serology. These latter analyses were conducted using the unconditional logistic regression methods.
We used SAS statistical software version 9.2 (SAS Institute, Cary, NC, USA). All P-values quoted are two-sided. P-values <0.05 were considered statistically significant.
Results
A total of 5469 (8.9%) subjects reported a history of diabetes at baseline. The mean age of initial diagnosis of diabetes was 51.8 (s.d. 9.4) years and >95% were diagnosed with diabetes after 35 years of age. The diabetics were older, less educated, had higher BMI, consumed less alcohol and drank less coffee, but more tea than non-diabetics. Diabetics who smoked were more likely to quit smoking than their non-diabetic counterparts (Table 1).
After an average of 14.0 (s.d. 3.7) years of follow-up, there were 499 incident HCC cases in this cohort. Men comprised close to three-fourths of the HCC case group (Table 1). The HCC cases were older, slightly higher in BMI, more likely to smoke cigarettes and consumed more alcoholic beverages than cohort subjects free of HCC (Table 1).
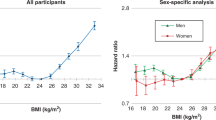
A history of diabetes was associated with an approximately two-fold risk of developing HCC (HR 2.64, 95% CI 2.09–3.33) (Table 2). Adjustment for cigarette smoking, alcohol intake and other potential confounders did not materially change the HR for HCC associated with diabetes (HR 2.14, 95% CI 1.69–2.71). The HRs for HCC in men (HR 2.11, 95% CI 1.58–2.81) and in women (HR 2.14, 95% CI 1.41–3.25) were comparable, though the women had only one-third the incidence rate of HCC in men (28.2 vs 98.3 per 100 000 person-years).
Table 2 also shows the diabetes–HCC association across strata of subjects defined by their time interval (years) between first clinical diagnosis of diabetes and enrolment in the cohort. There was no material differences in risk across the three strata, with subjects having the longest history of diabetes being those diagnosed ⩾10 years prior to their cohort enrolment, and subjects having the shortest history being those diagnosed within 5 years of cohort enrolment. The ORs of HCC for subjects with different length of diabetes history compared with non-diabetics were constant (P for heterogeneity=0.58). We further examined the diabetes–HCC association, stratified by established and probable risk factors of HCC including BMI, cigarette smoking status and alcohol consumption status at baseline. No material differences across the subgroups were observed (data not shown).
We have previously published the relationships between markers of HBV and HCV infections and HCC risk in a case-control set nested within the cohort of The Singapore Chinese Health Study (Koh et al, 2011) (reproduced in Table 3). Chronic carriers of HBV (HBsAg-positive subjects) exhibited the highest risk of HCC (odds ratio (OR)=24.79; 95% confidence interval (CI)=8.61- 71.34). Subjects with a history of primary infection of HBV (anti-HBc positive) without subsequent acquisition of immunity (anti-HBs negative) also were at an increased risk of HCC, though the risk level was an order of magnitude lower than those positive for HBsAg (OR=2.01; 95% CI=0.92–4.39). Conversely, subjects showing the presence of serum anti-HBs were not at an increased risk of HCC. Hepatitis C virus infection was rare in this population; only 5 HCC cases (5%) and 3 control subjects (1%) were positive for anti-HCV. Nonetheless, HCV infection was statistically significantly related to HCC (OR=10.12; 95% CI=2.19–46.80) (Table 3).
Table 4 shows the diabetes–HCC association within the nested case-control set of HCC as described in Table 3. The diabetes–HCC association was mainly noted in the serology-negative subgroup (HR=5.15; 95%CI=2.08–12.73). The corresponding HR in the serology-positive subgroup was 1.01 (95% CI=0.30–3.39). The interaction between diabetes and serological markers for hepatitis B or C on HCC risk was statistically significant (P for interaction=0.012).
Discussion
The present study shows that diabetics experienced a two-fold risk of HCC in this high-risk population with a relatively high prevalence of hepatitis B viral infection. The observed elevation in HCC risk among diabetics was statistically significant in the subgroup of subjects totally devoid of viral HBV/HCV serology. Chronic carriers of viral hepatitis are at risk for diabetes (Naing et al, 2012; Schillie et al, 2012). Thus, our observation of a clear and highly significant association between diabetes and HCC risk among subjects completely devoid of viral hepatitis serology greatly strengthens the notion that the diabetes–HCC association is direct and causal in nature. The magnitude of risk for HCC among diabetics did not vary materially by the duration of diabetes among at-risk individuals. Diabetics who were diagnosed ⩾10 years prior to cohort enrolment continued to exhibit a two-fold risk of HCC that was statistically significant and comparable to the risk of HCC among patients with the diagnosis of diabetes within 5 years prior to study enrolment. These latter findings strongly argue against the possibility of diabetes present in HCC patients as a consequence of late-stage liver disease. These results also suggest that medication treatment for diabetes did not have much impact on the risk of developing HCC.
Our results are consistent with the literature. Previous population-based studies representing observations from varied geographical locations, including Japan (Fujino et al, 2001; Tazawa et al, 2002; Shibata et al, 2003; Inoue et al, 2006), Korea (Jee et al, 2005), the US (Coughlin et al, 2004; El-Serag et al, 2004; Atchison et al, 2011) and European countries (Adami et al, 1996; Wideroff et al, 1997; Batty et al, 2004; Ogunleye et al, 2009; Zhou et al, 2010) have recorded a statistically significant increased incidence of HCC among patients with diabetes. The present study represents the first analysis from a southeast Asian population at relatively high risk for HCC. Overall, the epidemiologic evidence strongly supports a role for diabetes in the development of liver cancer across diverse populations with different levels of risk for HCC.
The biological mechanism of diabetes and its associated condition, obesity, in hepatocarcinogenesis is not well understood. The effect of increased serum insulin levels remains the most well studied and plausible mechanism for the association between diabetes and cancer (Ma et al, 1999), though increased insulin level alone may not be sufficient in causing HCC. Levels of insulin-like growth factor-1 (IGF-1) has been associated with the risk of colorectal (Ma et al, 1999; Grimberg and Cohen, 2000) and pancreatic cancer (Ohmura et al, 1990). Recent studies have suggested that circulating IGF-1 levels were associated with the increased risk of HCC (Elsammak et al, 2006; Su et al, 2010), and IGF-1 levels have been shown to promote liver tumour cell growth in experimental studies (Dunn et al, 1997; Pollak, 2000).
The development of primary liver cancer undergoes a long process in which chronic hepatic insult results in increased tissue turnover that leads to elevated risk of hepatocarcinogenesis. The intersecting effects of alcohol intake, chronic infection with hepatitis B and/or C viruses, obesity and the development of insulin resistance makes understanding the exact nature of the association between diabetes and HCC difficult, though the effects of elevated insulin levels due to insulin resistance remains the most well studied effect of diabetes on HCC development. Increased levels of insulin in the body due to insulin resistance results in compensatory increases in the level of growth hormone (Le Roith, 1997), potentially leading to the downstream promotion of carcinogenesis. This effect has been shown to promote cell proliferation in the pancreas (Ohmura et al, 1990), and it is possible that similar effects would be observed in the liver.
In the present study, the effect of diabetes on HCC risk was confined to individuals negative for all HBV and HCV serological markers. Our results are consistent with those reported from a recent prospective study of Chinese in Taiwan. History of diabetes was associated with a statistically significant 5.4-fold risk of HCC among study participants negative for chronic HBV or HCV infections (Wang et al, 2009). Unlike the Singapore Chinese in whom hepatitis C infection has a negligible role in HCC, both HBV and HCV have been shown to contribute to the HCC burden in Taiwan Chinese (Lai et al, 2012). Significantly, the Taiwan study reports a 3.1-fold HCC risk for diabetes among subjects positive for anti-HCV but no increased HCC risk for diabetes among subjects positive for HBsAg, a marker of chronic HBV infection (Wang et al, 2009).
The issue of temporality has been raised for the association between diabetes and HCC, given the critical roles of the liver in the metabolism of glucose. Glucose is absorbed from the intestinal tract and transported via the portal vein to the liver, where glycogen is made and stored. Hepatocytes have specific cell membrane insulin receptors, where insulin secreted by the pancreatic β-cells can bind and facilitate the uptake and utilisation of glucose. The utilisation and storage of glucose as a fuel in humans is promoted by insulin. Excessive glycogen accumulation in the liver is seen in 80% of diabetic patients (Stone and Van Thiel, 1985). Patients showing solely excessive glycogen deposition may exhibit hepatomegaly and liver enzyme abnormalities (Chatila and West, 1996), an indication of liver damage. Diabetes increases the risk of steatohepatitis, which can progress to cirrhosis. Obesity is a comorbidity of diabetes and the underlying cause of nonalcoholic steatohepatitis (NASH). Clinical studies have shown that 40–100% patients with NASH are obese and that 20–75% of them have a history of adult-onset diabetes (Reid, 2001). Furthermore, the severity of fibrosis among NASH patients is positively associated with obesity and diabetes (Angulo et al, 1999). It is known that a high percentage (up to 70%) of patients with cryptogenic cirrhosis were obese and/or diabetic (Caldwell et al, 1999). These clinical data suggest that obesity/diabetes are risk factors for hepatic fibrosis and progression to cirrhosis, a recognised predisposing factor for HCC regardless of the underlying cause of hepatic cirrhosis (Zaman et al, 1985).
Conversely, individuals with cirrhosis have elevated insulin levels, suggesting insulin resistance or reduced degradation of insulin by the cirrhotic liver. Impaired insulin secretion from the pancreatic β-cells has been proposed as a cause for the hyperglycaemia. Hepatogenous diabetes, characterised by glucose intolerance due to extensive liver damage, is estimated to be present in 30–60% of patients with cirrhosis (Garcia-Compean et al, 2009). Glucose intolerance in patients with cirrhosis has been found to be associated with low insulin secretion (Shah et al, 1995). These clinical findings suggest that elevated levels of circulating glucose or diabetes could be the result of a chronic liver disease that is aetiologically linked to the patient’s HCC development. The long period between the onset of diabetes and diagnosis of HCC allowed us to address this issue. The equally strong elevation in HCC risk, we noted in diabetics diagnosed 10 or more years prior to cohort enrolment, supports a causal interpretation of the association rather than the occurrence of diabetes as a consequence of late-stage liver disease.
The strengths of this study include the prospective study design, long-term follow-up, (up to 15 years) and complete ascertainment of incident HCC cases among cohort participants. A comprehensive questionnaire for the collection of data on many potentially confounding factors allowed for their adjustment in the examination of the association between diabetes and HCC risk. The available data on HBV/HCV serology on a subset of the present study population also allowed us to rule out the possibility of confounding by HBV/HCV infection on the diabetes–HCC risk association.
However, there are a number of potential limitations in our study. First, we only use the baseline status of diabetes in our analysis, and with increasing age, there would be an increase in incidence of diabetes in the non-diabetic subpopulation. Such misclassification in diabetes based on the baseline interview only can potentially bias the magnitude of the diabetes–HCC risk association towards the null. We did not differentiate between type 1 and type 2 diabetes when we interviewed the participants. However, >95% of patients were diagnosed with diabetes after 35 years of age. Hence, virtually all diabetes cases in the present study would be considered as type 2 diabetes. We did not have data on the treatment for diabetes, including the use of medication, and the adequacy of diabetes control in our study population. The lack of a dose–response relationship for duration of diabetes prior to the baseline interview (Table 2) did not support a modifying effect of the use of diabetes medication or diabetes severity on HCC risk. Furthermore, diabetic patients using statins or metformin experienced reduced, but not increased risk of HCC (El-Serag et al, 2009; Chen et al, 2012). Therefore, the observed positive association between diabetes and the risk of developing HCC in this prospective study would be less likely due to the use of medication for diabetes. Finally, we did not measure serological markers of HBV/HCV infections on all cohort participants nor did we assess the history of cirrhosis in our baseline interviews. Therefore, we were unable to examine these confounders in a whole cohort statistical analysis of the diabetes–HCC risk association. However, an appropriately designed nested case-control study within a whole cohort is universally recognised to yield valid findings, and we have conducted such a study to examine the potential modifying role of viral hepatitis in the diabetes–HCC association. We noted that the diabetes–HCC association was seen only among subjects negative for all tested HBV/HCV serology, indicating a lack of influence by viral hepatitis or its clinical sequelae (cirrhosis) on the diabetes–HCC association.
In conclusion, the present study demonstrates a statistically significant, positive association between diabetes status at baseline and elevated risk of developing HCC among Singaporean Chinese, a population with relatively high prevalence of HBV infection and HCC incidence. This positive diabetes–HCC risk association present in individuals without chronic infection with HBV or HCV virus suggests an independent role of diabetes in HCC development, which has an important implication in public health, given the worldwide increasing incidence of type 2 diabetes.
Change history
19 March 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Adami HO, Chow WH, Nyren O, Berne C, Linet MS, Ekbom A, Wolk A, McLaughlin JK, Fraumeni JF Jr (1996) Excess risk of primary liver cancer in patients with diabetes mellitus. J Natl Cancer Inst 88: 1472–1477
Angulo P, Keach JC, Batts KP, Lindor KD (1999) Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology 30: 1356–1362
Atchison EA, Gridley G, Carreon JD, Leitzmann MF, McGlynn KA (2011) Risk of cancer in a large cohort of US veterans with diabetes. Int J Cancer 128: 635–643
Batty GD, Shipley MJ, Marmot M, Smith GD (2004) Diabetes status and post-load plasma glucose concentration in relation to site-specific cancer mortality: findings from the original Whitehall study. Cancer Causes Control 15: 873–881
Bjornholt JV, Erikssen G, Aaser E, Sandvik L, Nitter-Hauge S, Jervell J, Erikssen J, Thaulow E (1999) Fasting blood glucose: an underestimated risk factor for cardiovascular death. Results from a 22-year follow-up of healthy nondiabetic men. Diabetes Care 22: 45–49
Caldwell SH, Oelsner DH, Iezzoni JC, Hespenheide EE, Battle EH, Driscoll CJ (1999) Cryptogenic cirrhosis: clinical characterization and risk factors for underlying disease. Hepatology 29: 664–669
Chatila R, West AB (1996) Hepatomegaly and abnormal liver tests due to glycogenosis in adults with diabetes. Medicine 75: 327–333
Chen HP, Shieh JJ, Chang CC, Chen TT, Lin JT, Wu MS, Lin JH, Wu CY (2012) Metformin decreases hepatocellular carcinoma risk in a dose-dependent manner: population-based and in vitro studies. Gut e-pub ahead of print 7 July 2012; doi:10.1136/gutjnl-2011-201708
Coughlin SS, Calle EE, Teras LR, Petrelli J, Thun MJ (2004) Diabetes mellitus as a predictor of cancer mortality in a large cohort of US adults. Am J Epidemiol 159: 1160–1167
Dunn SE, Kari FW, French J, Leininger JR, Travlos G, Wilson R, Barrett JC (1997) Dietary restriction reduces insulin-like growth factor I levels, which modulates apoptosis, cell proliferation, and tumor progression in p53-deficient mice. Cancer Res 57: 4667–4672
El-Serag HB, Davila JA, Petersen NJ, McGlynn KA (2003) The continuing increase in the incidence of hepatocellular carcinoma in the United States: an update. Ann Intern Med 139: 817–823
El-Serag HB, Johnson ML, Hachem C, Morgana RO (2009) Statins are associated with a reduced risk of hepatocellular carcinoma in a large cohort of patients with diabetes. Gastroenterology 136: 1601–1608
El-Serag HB, Tran T, Everhart JE (2004) Diabetes increases the risk of chronic liver disease and hepatocellular carcinoma. Gastroenterology 126: 460–468
Elsammak MY, Amin GM, Khalil GM, Ragab WS, Abaza MM (2006) Possible contribution of serum activin A and IGF-1 in the development of hepatocellular carcinoma in Egyptian patients suffering from combined hepatitis C virus infection and hepatic schistosomiasis. Clin Biochem 39: 623–629
Federation ID (2009) IDF Diabetes Atlas 4th edn, International Diabetes Federation: Brussels, Belgium
Foundation NK (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39: S1–266
Friberg E, Orsini N, Mantzoros CS, Wolk A (2007) Diabetes mellitus and risk of endometrial cancer: a meta-analysis. Diabetologia 50: 1365–1374
Fujino Y, Mizoue T, Tokui N, Yoshimura T (2001) Prospective study of diabetes mellitus and liver cancer in Japan. Diabetes Metab Res Rev 17: 374–379
Garcia-Compean D, Jaquez-Quintana JO, Maldonado-Garza H (2009) Hepatogenous diabetes. Current views of an ancient problem. Ann Hepatol 8: 13–20
Grimberg A, Cohen P (2000) Role of insulin-like growth factors and their binding proteins in growth control and carcinogenesis. J Cell Physiol 183: 1–9
Hankin JH, Stram DO, Arakawa K, Park S, Low SH, Lee HP, Yu MC (2001) Singapore Chinese Health Study: development, validation, and calibration of the quantitative food frequency questionnaire. Nutr Cancer 39: 187–195
Huxley R, Ansary-Moghaddam A, Berrington de Gonzalez A, Barzi F, Woodward M (2005) Type-II diabetes and pancreatic cancer: a meta-analysis of 36 studies. Br J Cancer 92: 2076–2083
Inoue M, Iwasaki M, Otani T, Sasazuki S, Noda M, Tsugane S (2006) Diabetes mellitus and the risk of cancer: results from a large-scale population-based cohort study in Japan. Arch Intern Med 166: 1871–1877
Jee SH, Ohrr H, Sull JW, Yun JE, Ji M, Samet JM (2005) Fasting serum glucose level and cancer risk in Korean men and women. JAMA 293: 194–202
Johnson S, Koh WP, Wang R, Govindarajan S, Yu MC, Yuan JM (2011) Coffee consumption and reduced risk of hepatocellular carcinoma: findings from the Singapore Chinese Health Study. Cancer Causes Control 22: 503–510
Kelly T, Yang W, Chen CS, Reynolds K, He J (2008) Global burden of obesity in 2005 and projections to 2030. Int J Obes 32: 1431–1437
Koh WP, Robien K, Wang R, Govindarajan S, Yuan JM, Yu MC (2011) Smoking as an independent risk factor for hepatocellular carcinoma: the Singapore Chinese Health Study. Br J Cancer 105: 1430–1435
Koh WP, Yuan JM, Sun CL, van den Berg D, Seow A, Lee HP, Yu MC (2003) Angiotensin I-converting enzyme (ACE) gene polymorphism and breast cancer risk among Chinese women in Singapore. Cancer Res 63: 573–578
Lai MS, Hsieh MS, Chiu YH, Chen TH (2006) Type 2 diabetes and hepatocellular carcinoma: A cohort study in high prevalence area of hepatitis virus infection. Hepatology 43: 1295–1302
Lai SW, Chen PC, Liao KF, Muo CH, Lin CC, Sung FC (2012) Risk of hepatocellular carcinoma in diabetic patients and risk reduction associated with anti-diabetic therapy: a population-based cohort study. Am J Gastroenterol 107: 46–52
Larsson SC, Mantzoros CS, Wolk A (2007) Diabetes mellitus and risk of breast cancer: a meta-analysis. Int J Cancer 121: 856–862
Larsson SC, Orsini N, Brismar K, Wolk A (2006) Diabetes mellitus and risk of bladder cancer: a meta-analysis. Diabetologia 49: 2819–2823
Larsson SC, Orsini N, Wolk A (2005) Diabetes mellitus and risk of colorectal cancer: a meta-analysis. J Natl Cancer Inst 97: 1679–1687
Le Roith D (1997) Seminars in medicine of the Beth Israel Deaconess Medical Center. Insulin-like growth factors. N Engl J Med 336: 633–640
Ma J, Pollak MN, Giovannucci E, Chan JM, Tao Y, Hennekens CH, Stampfer MJ (1999) Prospective study of colorectal cancer risk in men and plasma levels of insulin-like growth factor (IGF)-I and IGF-binding protein-3. J Natl Cancer Inst 91: 620–625
Naing C, Mak JW, Ahmed SI, Maung M (2012) Relationship between hepatitis C virus infection and type 2 diabetes mellitus: meta-analysis. World J Gastroenterol 18: 1642–1651
Odegaard AO, Pereira MA, Koh WP, Arakawa K, Lee HP, Yu MC (2008) Coffee, tea, and incident type 2 diabetes: the Singapore Chinese Health Study. Am J Clin Nutr 88: 979–985
Ogunleye AA, Ogston SA, Morris AD, Evans JM (2009) A cohort study of the risk of cancer associated with type 2 diabetes. Br J Cancer 101: 1199–1201
Ohata K, Hamasaki K, Toriyama K, Matsumoto K, Saeki A, Yanagi K, Abiru S, Nakagawa Y, Shigeno M, Miyazoe S, Ichikawa T, Ishikawa H, Nakao K, Eguchi K (2003) Hepatic steatosis is a risk factor for hepatocellular carcinoma in patients with chronic hepatitis C virus infection. Cancer 97: 3036–3043
Ohmura E, Okada M, Onoda N, Kamiya Y, Murakami H, Tsushima T, Shizume K (1990) Insulin-like growth factor I and transforming growth factor alpha as autocrine growth factors in human pancreatic cancer cell growth. Cancer Res 50: 103–107
Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas D (2002) Cancer Incidence in Five Continents IARC Scientific Publications No 155. IARC: Lyon
Pollak M (2000) Insulin-like growth factor physiology and cancer risk. Eur J Cancer 36: 1224–1228
Reid AE (2001) Nonalcoholic steatohepatitis. Gastroenterology 121: 710–723
Schillie SF, Xing J, Murphy TV, Hu DJ (2012) Prevalence of hepatitis B virus infection among persons with diagnosed diabetes mellitus in the United States, 1999-2010. J Viral Hepat 19: 674–676
Shah P, Mares D, Fineberg E, Pescovitz M, Filo R, Jindal R, Mahoney S, Lumeng L (1995) Insulin autoimmune syndrome as a cause of spontaneous hypoglycemia in alcoholic cirrhosis. Gastroenterology 109: 1673–1676
Shibata A, Ogimoto I, Kurozawa Y, Nose T, Yoshimura T, Suzuki H, Iwai N, Sakata R, Fujita Y, Ichikawa S, Fukuda K, Tamakoshi A (2003) Past medical history and risk of death due to hepatocellular carcinoma, univariate analysis of JACC study data. Kurume Med J 50: 109–119
Stone BG, Van Thiel DH (1985) Diabetes mellitus and the liver. Semin Liver Dis 5: 8–28
Su WW, Lee KT, Yeh YT, Soon MS, Wang CL, Yu ML, Wang SN (2010) Association of circulating insulin-like growth factor 1 with hepatocellular carcinoma: one cross-sectional correlation study. J Clin Lab Anal 24: 195–200
Tapp RJ, Shaw JE, Harper CA, de Courten MP, Balkau B, McCarty DJ, Taylor HR, Welborn TA, Zimmet PZ (2003) The prevalence of and factors associated with diabetic retinopathy in the Australian population. Diabetes Care 26: 1731–1737
Tazawa J, Maeda M, Nakagawa M, Ohbayashi H, Kusano F, Yamane M, Sakai Y, Suzuki K (2002) Diabetes mellitus may be associated with hepatocarcinogenesis in patients with chronic hepatitis C. Dig Dis Sci 47: 710–715
Veldt BJ, Chen W, Heathcote EJ, Wedemeyer H, Reichen J, Hofmann WP, de Knegt RJ, Zeuzem S, Manns MP, Hansen BE, Schalm SW, Janssen HL (2008) Increased risk of hepatocellular carcinoma among patients with hepatitis C cirrhosis and diabetes mellitus. Hepatology 47: 1856–1862
Wang CS, Yao WJ, Chang TT, Wang ST, Chou P (2009) The impact of type 2 diabetes on the development of hepatocellular carcinoma in different viral hepatitis statuses. Cancer Epidemiol Biomarkers Prev 18: 2054–2060
Wideroff L, Gridley G, Mellemkjaer L, Chow WH, Linet M, Keehn S, Borch-Johnsen K, Olsen JH (1997) Cancer incidence in a population-based cohort of patients hospitalized with diabetes mellitus in Denmark. J Natl Cancer Inst 89: 1360–1365
Yu MC, Tong MJ, Govindarajan S, Henderson BE (1991) Nonviral risk factors for hepatocellular carcinoma in a low-risk population, the non-Asians of Los Angeles County, California. J Natl Cancer Inst 83: 1820–1826
Yuan JM, Govindarajan S, Arakawa K, Yu MC (2004) Synergism of alcohol, diabetes, and viral hepatitis on the risk of hepatocellular carcinoma in blacks and whites in the US. Cancer 101: 1009–1017
Zaman SN, Melia WM, Johnson RD, Portmann BC, Johnson PJ, Williams R (1985) Risk factors in development of hepatocellular carcinoma in cirrhosis: prospective study of 613 patients. Lancet 1: 1357–1360
Zhou XH, Qiao Q, Zethelius B, Pyorala K, Soderberg S, Pajak A, Stehouwer CD, Heine RJ, Jousilahti P, Ruotolo G, Nilsson PM, Calori G, Tuomilehto J (2010) Diabetes, prediabetes and cancer mortality. Diabetologia 53: 1867–1876
Acknowledgements
We thank Siew-Hong Low of the National University of Singapore for supervising the field work of the Singapore Chinese Health Study. The Singapore Cancer Registry assisted with the identification of cancer and mortality outcomes via database linkages. This study was supported by National Institutes of Health (NCI R01 CA55069, R35 CA53890 and R01 CA80205, R01 CA144034).
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Koh, WP., Wang, R., Jin, A. et al. Diabetes mellitus and risk of hepatocellular carcinoma: findings from the Singapore Chinese Health Study. Br J Cancer 108, 1182–1188 (2013). https://doi.org/10.1038/bjc.2013.25
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.25
Keywords
This article is cited by
-
VFMAP predicted hepatocellular carcinoma development in patients with chronic hepatitis C who were treated with direct-acting antiviral and achieved sustained virologic response
Journal of Medical Ultrasonics (2023)
-
Decreased ZO1 expression causes loss of time-dependent tight junction function in the liver of ob/ob mice
Molecular Biology Reports (2022)
-
Hepatocellular carcinoma as a leading cause of cancer-related deaths in Japanese type 2 diabetes mellitus patients
Journal of Gastroenterology (2019)
-
Diabetes mellitus and the risk of gastrointestinal cancer in women compared with men: a meta-analysis of cohort studies
BMC Cancer (2018)
-
Sex differences in the association between diabetes and cancer: a systematic review and meta-analysis of 121 cohorts including 20 million individuals and one million events
Diabetologia (2018)