Abstract
Background:
Platinum-based doublet chemotherapy is the standard first-line treatment for advanced non-small cell lung cancer (NSCLC), but earlier studies have suggested that non-platinum combinations are equally effective and better tolerated. We conducted a national, randomised study to compare a non-platinum with a platinum combination.
Methods:
Eligible patients had stage IIIB/IV NSCLC and performance status (PS) 0–2. Patients received up to three cycles of vinorelbine 60 mg m−2 p.o.+gemcitabine 1000 mg m−2 i.v. day 1 and 8 (VG) or vinorelbine 60 mg m−2 p.o. day 1 and 8+carboplatin area under the curve=5 (Calvert's formula) i.v. day 1 (VC). Patients ⩾75 years received 75% of the dose. Endpoints were overall survival, health-related quality of life (HRQoL), toxicity, and the use of radiotherapy.
Results:
We randomised 444 patients from September 2007 to April 2009. The median age was 65 years, 58% were men and 25% had PS 2. Median survival was VG: 6.3 months; VC: 7.0 months, P=0.802. Vinorelbine plus carboplatin patients had more grade III/IV nausea/vomiting (VG: 4%, VC: 12%, P=0.008) and grade IV neutropenia (VG: 7%, VC: 19%, P<0.001). Infections, HRQoL and the use of radiotherapy did not differ significantly between the treatment groups.
Conclusion:
The two regimens yielded similar overall survival. The VG combination had only a slightly better toxicity profile.
Similar content being viewed by others
Main
The ideal palliative cancer therapy is effective, harmless and easy to administer. Platinum-based combination chemotherapy is regarded as the standard in first-line therapy in the majority of patients with advanced non-small cell lung cancer (NSCLC). However, benefits in terms of prolonged survival and symptom relief are modest, whereas side effects are common, even when carboplatin is chosen over cisplatin for its favourable toxicity profile (Azzoli et al, 2009; Goffin et al, 2010). Thus, searching for alternative regimens that might improve health-related quality of life (HRQoL) while maintaining efficacy, is still warranted. An approach is to combine two of the modern third generation non-platinum agents, such as docetaxel, paclitaxel, pemetrexed, vinorelbine, or gemcitabine.
Several randomised controlled trials have compared a platinum combination with vinorelbine and gemcitabine (VG) (Laack et al, 2004; Zhang et al, 2004; Barlesi and Pujol, 2005; Lilenbaum et al, 2005; Tan et al, 2005; Yamamoto et al, 2006; Greco et al, 2007; Han et al, 2008; Kubota et al, 2008). Most of these studies demonstrated that VG is as effective but less toxic than the respective platinum combinations. One study (Tan et al, 2005), however, compared VG with vinorelbine plus carboplatin (VC), both regimens administered in a 3-week schedule to a maximum of six cycles. They found superior survival of 3 months and a more favourable toxicity profile for the VG combination.
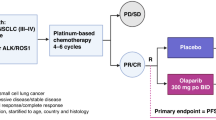
As a response to the improved survival by VG over VC presented by Tan et al (2005), the Norwegian Lung Cancer Study Group designed a randomised study comparing VG with VC as a first-line treatment in patients with advanced NSCLC. We chose to administer three cycles of chemotherapy, based on the results of three randomised studies assessing the length of therapy in advanced NSCLC (Smith et al, 2001; Socinski et al, 2002; von Plessen et al, 2006). Further, we chose oral vinorelbine for both treatment arms because of convenient administration, patient preferences, and a similar safety profile as the intravenous formulation (Vokes et al, 1994; Liu et al, 1997; Jassem et al, 2001; Marty et al, 2001; Jassem et al, 2003; O'Brien et al, 2004; Jensen et al, 2008).
The primary aim of the study was whether VG is superior to VC with respect to overall survival. Secondary aims were to compare HRQoL, toxicity, and the use of palliative radiotherapy.
Patients and methods
Design and approval
The study was an open, randomised, multicenter phase III trial. It was approved by the Regional Committee for Medical Research Ethics, Western Norway, the Norwegian Social Science Data Services, and the Norwegian Medicines Agency.
Eligibility criteria
Eligible patients had NSCLC stage IV or stage IIIB not eligible for curative treatment, and WHO performance status (PS) 0–2. Patients had to have adequate bone marrow and liver function, no other active malignancy and no gastrointestinal disease affecting absorption of vinorelbine. We allowed inclusion of patients with brain metastases, and defined no upper age limit.
Randomisation
After the patients had signed the informed consent form and completed the baseline HRQoL form, they were randomised by phone to the central study office at Haukeland University Hospital, Bergen, Norway. Randomisation was stratified by WHO PS 0–1 vs 2, stage IIIB vs IV and age <75 vs ⩾75 years.
Chemotherapy
Both groups were planned for three cycles of chemotherapy in 3-week cycles. Vinorelbine and gemcitabine patients received vinorelbine capsules 60 mg m−2 plus intravenous gemcitabine 1000 mg m−2, on days 1 and 8. Vinorelbine plus carboplatin patients received carboplatin according to area under the curve=5 (Calvert's formula) on day 1 plus vinorelbine capsules 60 mg m−2 on days 1 and 8. The oral dose of vinorelbine 60 mg m−2 is comparable with the commonly used intravenous dose of 25 mg m−2 (Marty et al, 2001). Patients 75 years and older had their doses reduced by 25%. Both groups received prophylactic antiemetics with an intravenous glucocorticoid and 5-HT3-antagonist on day 1, the VG patients also on day 8. Vinorelbine plus carboplatin patients received an oral 5-HT3-antagonist b.i.d. on day 8.
Before the start of each cycle, the absolute neutrophil count (ANC) had to be ⩾1.0 × 109 l−1 and platelets ⩾75 × 109 l−1. The doses were reduced by 25% if ANC was 1.0–1.49 × 109 l−1, platelets were 75–99 × 109 l−1, or preceding nadir ANC was <0.5 × 109 l−1. Doses were reduced by 50% if the nadir platelet count was <50 × 109 l−1. All dose reductions were maintained for subsequent cycles. Chemotherapy was discontinued if a cycle was delayed by more than 21 days. In cases of neutropenic infections or other grade 3–4 toxicity, chemotherapy was postponed until clinical and haematological recovery and all remaining doses were reduced by 25%. Disease progression, unacceptable toxicity or a patient’s request were reasons for discontinuation of the study treatment.
Patient follow-up
All patients underwent a chest X-ray and a CT scan of thorax and upper abdomen before randomisation. Patients were examined clinically and weighed at the start of each treatment cycle. Laboratory tests were performed weekly throughout the treatment period. A chest x-ray was performed at week 9 and every 8 weeks thereafter. Further imaging to determine the disease progression was performed at the treating physician’s discretion.
Endpoints
The primary endpoint was overall survival. The secondary endpoints were HRQoL, toxicity and the use of palliative radiotherapy. The prespecified HRQoL analyses were differences between the treatment arms in global QoL and symptom scales for pain, nausea/vomiting, dyspnoea, and fatigue. We defined global QoL at week 9 as the primary HRQoL-endpoint. The study was not designed to assess response rates or time to progression.
Assessment of HRQoL
The patients reported HRQoL on the European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire QLQ-C30 and its lung cancer-specific module LC13 (Aaronson et al, 1993). The QLQ-C30 measures fundamental aspects of HRQoL and symptoms commonly reported by cancer patients, whereas the LC13 measures symptoms commonly associated with lung cancer and its treatment. Baseline HRQoL questionnaires had to be completed before randomisation. Follow-up questionnaires were mailed from the study office to the patients' home addresses and were completed immediately before each cycle, 3 weeks after the last cycle, and then every 8 weeks until 57 weeks after the start of treatment. Patients returned the completed forms to the study office in a pre-stamped envelope. Non-responders received one reminder by mail after 14 days.
Statistical considerations
We needed 444 patients to detect an increase in 1-year survival from 29 to 40% with 80% power at a 5% significance level, assuming an accrual time of 52 weeks and a minimum follow-up time of 52 weeks. We used the function cpower in Frank Harrell’s Hmisc package for R for power calculations (Harrell, 2003). We defined survival time as the time from randomisation until death, and compared the treatment groups with the Kaplan–Meier method and the log-rank test.
Health-related quality of life scores were calculated according to the EORTC QLQ-C30 Scoring Manual (Fayers et al, 2001). A high global health status QoL score represents a good QoL, whereas a high symptom-scale score represents more symptoms. Mean scores were calculated for reported values only and compared between the two groups using the Mann–Whitney U-test. We considered a difference in the mean score of >10 points as clinically relevant. Toxicity was categorised according to the Common Terminology Criteria for Adverse Events (CTCAE) v3.0 (http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf). The Mann–Whitney U-test was used for group comparisons of haematological toxicity. For analyses of other adverse events and the need for palliative radiotherapy, the χ2 test was used. The level of significance was defined as P<0.05.
Results
Patients
Between September 2007 and April 2009, 444 patients from 35 Norwegian hospitals were randomised. Seven patients were excluded from all analyses; six because of ineligibility, and one because of administration of the wrong study therapy. Three patients did not receive any study treatment (Figure 1). The analysed patients had, VG vs VC respectively, a median age of 65 vs 65 years, 41% vs 43% had female gender, 26% vs 25% had PS level 2, 85% vs 85% had disease stage IV, 55% vs 59% had adenocarcinoma, and 5% vs 7% were never smokers (Table 1). We analysed 437 patients for survival, HRQoL and use of palliative radiotherapy, and 434 for toxicity. The survival analysis was finalised in May 2011 after 416 patients had died.
Chemotherapy
The mean number of chemotherapy cycles was (VG vs VC, respectively) 2.6 vs 2.7, while patients ⩾75 years received 2.3 vs 2.7 cycles. The number of patients receiving three cycles without dose reduction was 127 (59%) vs 128 (58%). Study therapy was discontinued due to toxicity in 9 (4%) vs 7 (3%) patients, and due to progressive disease in 24 (11%) vs 25 (11%) patients. Study therapy on day 8 was omitted in 44 of 551 (8%) vs 37 of 593 (6%) cycles.
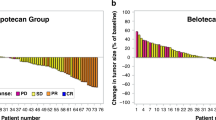
Overall survival
Overall survival did not differ significantly between the two treatment groups (Figure 2). The median survival time was 6.3 vs 7.0 months (HR=1.025, CI=0.85–1.24; P=0.802), with a corresponding 1-year survival rate of 30% vs 27% in the VG and VC arms, respectively.
Good PS and disease stage III were associated with a better prognosis. Median survival was 12.2, 6.8, and 4.3 months for PS 0, 1, and 2, respectively, (P<0.001). Median survival was 9.0, 10.4, and 6.3 months for stage IIIBdry, stage IIIBwet, and stage IV, respectively (P=0.036).
Post-hoc subgroup analyses showed that among patients ⩾75 years (n=74) VG patients had an inferior median survival of 4.6 vs 8.0 months for the VC patients (HR=1.70, CI=1.05–2.73; P=0.028), and a corresponding 1-year survival rate of 18% vs 28%. This difference was, however, not statistically significant in a multivariate analysis adjusting for PS level and stage of disease (HR=1.55, CI=0.95–2.53). We found no differences in median survival between the treatment arms for patients <75 years (VG: 6.9 months, VC: 6.8 months; HR=0.89, CI=0.72–1.10; P=0.296). Age itself was not found to be a significant prognostic factor (<75 years: 6.9 months, ⩾75 years: 6.2 months, P=0.066). Neither did multivariate analysis with interaction test reveal any significant association between age and survival.
We observed no significant differences between treatment arms (VG vs VC, respectively) at any PS level (PS 0: 12.6 vs 11.4 months, P=0.208; PS 1: 6.5 vs 7.0 months, P=0.835; PS 2: 4.0 vs 4.5 months, P=0.418) or stage of disease (IIIBdry: 11.3 vs 7.5 months, P=0.446; IIIBwet: 7.6 vs 10.8 months, P=0.913; IV: 6.2 vs 6.7 months, P=0.924). Neither did we find any significant association between survival and gender, histology or smoking history (data not shown).
Health-related quality of life
Alive patients completed, VG and VC, respectively, 89% (850 forms) and 90% (910 forms), of the expected HRQoL questionnaires during the first 17 weeks. The results of prespecified HRQoL analyses are summarised in Table 2. Vinorelbine plus carboplatin patients had a statistically significantly higher mean score for nausea/vomiting at week 3 (P=0.028) and week 6 (P=0.012), but the difference was only four points. We observed no significant differences between treatment arms after week 17, and neither did other scales or items differ consistently between treatment arms.
Toxicity
Haematological toxicity, adverse events, and hospital admissions are summarised in Table 3. Fewer patients in the VG arm experienced grade 4 neutropenia (VG: 7%; VC: 19%; P<0.001). We found no corresponding difference in the number of patients experiencing febrile neutropenia (VG: 4%; VC: 8%; P=0.127), or other grade 3 or grade 4 infections over all (VG: 20%, VC: 18%; P=0.517). Fewer VG patients experienced grade 3 or grade 4 nausea/vomiting (VG: 4%; VC: 12%; P=0.008). More VC patients received blood transfusions, but the difference was not statistically significant (VG: 10%; VC: 16%; P=0.092).
Post-study therapy
The use of palliative radiotherapy did not differ between the treatment arms as 101 (47%) VG patients and 111 (50%) VC patients received palliative radiotherapy (P=0.497).
Ninety-one (42%) VG patients and 97 (44%) VC patients received at least one systemic second-line therapy (P=0.773). The most common regimens were (VG vs VC) erlotinib (25% vs 27%), pemetrexed (17% vs 15%), and carboplatin-doublets (19% vs 9%). The use of systemic second-line therapy was associated with a better PS level (PS 0: 72%; PS 1: 39%; PS 2: 27%; P<0.001) and low age (<75 years: 46%; ⩾75 years: 27%; P=0.003).
Discussion
In this randomised trial we did not observe any difference in overall survival between VG and VC as first-line chemotherapy of advanced NSCLC. Thus, we could not confirm the results from Tan et al’s (2005) study where VG was found superior to VC. Our results corroborate a meta-analysis that demonstrated similar survival between carboplatin-based doublets and modern non-platinum doublets (Rajeswaran et al, 2008).
During the inclusion period of this study, 1185 individuals in Norway were diagnosed with NSCLC stage IV, whereas the number of stage IIIB patients, specifically, could not be assessed (Norwegian Cancer Registry, personal communication). Hence, the 371 stage IV patients enrolled in this study constituted 31% of these patients nationwide during the period, suggesting this study to be representative for the Norwegian population of patients with advanced NSCLC.
We chose an open-study design to facilitate participation of lung cancer centres of all sizes in this national study. The open design could possibly bias the HRQoL reporting. On the other hand, a blinded study’s drawback would be the necessity of a placebo infusion on day 8 in the VC arm, and thereby not reflecting the real clinical practice.
The median survival time was relatively short in both the treatment arms, only 6.3 and 7.0 months for patients in the VG and VC arms, respectively. This survival is lower than the 11.5 and 8.6 months in the study by Tan et al (2005). While the median age in their study was 60 years, it was 65 years in ours. They included patients with only Karnofsky PS level of 80–100 points, which approximates WHO PS level 0–1 (Buccheri et al, 1996), while we included 25% PS 2 patients. Tan et al (2005) did not include patients with brain metastases, which was allowed in the present study. The inclusion of patients with dissimilar important prognostic factors is a plausible explanation for the survival difference between these two studies.
The choice of carboplatin instead of cisplatin is a factor that could have influenced survival negatively in this study. The debate on cisplatin vs carboplatin is beyond the scope of this paper, but we note that the updated ASCO guideline state carboplatin as an acceptable option in advanced NSCLC, despite a small survival disadvantage (Azzoli et al, 2011).
Another question is whether the administration of only three chemotherapy cycles (as compared with four to six cycles recommended in guidelines) has influenced the survival negatively. A Scandinavian study showed that a six-cycle schedule is not significantly better than three cycles (von Plessen et al, 2006). Further, in another Norwegian study from our group, the four-cycle schedule of carboplatin and pemetrexed yielded a similar survival of 7.3 months (Gronberg et al, 2009). This suggests that a negative survival contribution from the short treatment length is of only minor significance in this study.
The current study offered combination chemotherapy to both elderly patients and PS 2 patients, while current NSCLC guidelines suggest the use of single-agent therapy in these groups (D’Addario et al, 2010). The trend towards a favourable survival of 8.0 months with VC in the elderly patients suggests that this regimen, with a 25% dose reduction, is an acceptable option. However, the poor 4.3 months median survival in PS 2 patients questions the use of toxic and time-consuming combination chemotherapy.
The use of systemic second-line therapy in only 43% of patients may have negatively affected the survival in this study. In selected populations of some clinical trials as many as 67% of the patients received second-line treatment (Ciuleanu et al, 2009; Reck et al, 2010). In routine clinical practice, however, the rate can be as low as 25% (Ramsey et al, 2008). Thus our second-line chemotherapy rate is closer to what is administered in the general clinical routine, presumably a consequence of the representative patient inclusion.
The response rates and survival results of oral vinorelbine are similar to intravenous vinorelbine in advanced NSCLC and breast cancer (Gralla et al, 2007; Aapro and Finek, 2011). The advantage of oral vinorelbine is home administration, so that patients, relatives and health care providers can save valuable time. Besides, oral vinorelbine induces no phlebitis, in contrast to the intravenous administration. The disadvantage is more frequent nausea and vomiting, which can be adequately controlled by prophylactic antiemetics. It has been shown that patients prefer taking oral vinorelbine at home instead of intravenous administration at the clinic (Jensen et al, 2008). Oral vinorelbine costs more than intravenous vinorelbine, but this is probably outweighed by fewer outpatient visits, quicker and less resource-demanding administration of the drug, and lower transportation expenses (Le et al, 2007). Overall, oral vinorelbine can be a useful alternative to the intravenous formulation in advanced NSCLC, especially where the distance to the hospital is substantial.
Both CTCAE reporting and HRQoL measurements indicated slightly more nausea and vomiting in VC patients. The antiemetic regimen differed a little between the treatment groups (VG patients received an i.v. glucocorticoid and 5-HT3-antagonist on day 8, VC patients an oral 5-HT3-antagonist only), but we find it unlikely that this minor difference should explain more nausea and vomiting in VC patients. However, the differences between the treatment arms in HRQoL analyses were below what are considered as clinically relevant, and the difference in grade III/IV adverse events of nausea and vomiting was relatively small. A previous meta-analysis failed to detect any significant difference in nausea and vomiting between non-platinum and carboplatin-based doublets (Rajeswaran et al, 2008).
In summary, the current study did not confirm prolonged survival of VG over VC, as first-line treatment in advanced NSCLC. The minor toxicity differences in favour of VG do not justify a change in the treatment practice. Thus, platinum-based doublet chemotherapy remains as the standard first-line treatment.
Change history
17 July 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Aapro M, Finek J (2011) Oral vinorelbine in metastatic breast cancer: A review of current clinical trial results. Cancer Treat Rev 38 (2): 120–126
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85: 365–376
Azzoli CG, Baker Jr S, Temin S, Pao W, Aliff T, Brahmer J, Johnson DH, Laskin JL, Masters G, Milton D, Nordquist L, Pfister DG, Piantadosi S, Schiller JH, Smith R, Smith TJ, Strawn JR, Trent D, Giaccone G (2009) American Society of Clinical Oncology Clinical Practice Guideline update on chemotherapy for stage IV non-small-cell lung cancer. J Clin Oncol 27: 6251–6266
Azzoli CG, Temin S, Aliff T, Baker Jr S, Brahmer J, Johnson DH, Laskin JL, Masters G, Milton D, Nordquist L, Pao W, Pfister DG, Piantadosi S, Schiller JH, Smith R, Smith TJ, Strawn JR, Trent D, Giaccone G (2011) 2011 Focused Update of 2009 American Society of Clinical Oncology Clinical Practice Guideline Update on Chemotherapy for Stage IV Non-Small-Cell Lung Cancer. J Clin Oncol 29: 3825–3831
Barlesi F, Pujol JL (2005) Combination of chemotherapy without platinum compounds in the treatment of advanced non-small cell lung cancer: A systematic review of phase III trials. Lung Cancer 49: 289–298
Buccheri G, Ferrigno D, Tamburini M (1996) Karnofsky and ECOG performance status scoring in lung cancer: a prospective, longitudinal study of 536 patients from a single institution. Eur J Cancer 32A: 1135–1141
Ciuleanu T, Brodowicz T, Zielinski C, Kim JH, Krzakowski M, Laack E, Wu YL, Bover I, Begbie S, Tzekova V, Cucevic B, Pereira JR, Yang SH, Madhavan J, Sugarman KP, Peterson P, John WJ, Krejcy K, Belani CP (2009) Maintenance pemetrexed plus best supportive care versus placebo plus best supportive care for non-small-cell lung cancer: a randomised, double-blind, phase 3 study. Lancet 374: 1432–1440
D’Addario G, Fruh M, Reck M, Baumann P, Klepetko W, Felip E (2010) Metastatic non-small-cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 21 (Suppl 5): v116–v119
Fayers P, Aaronson NK, Bjordal K, Groenvold M, Curran D, Bottomley A (2001) On Behalf of the EORTC Quality of Life Groups: The EORTC QLQ-C30 Scoring Manual 3rd edition. European Organisation for Research and Treatment of Cancer: Brussels
Goffin J, Lacchetti C, Ellis PM, Ung YC, Evans WK (2010) First-line systemic chemotherapy in the treatment of advanced non-small cell lung cancer: a systematic review. J Thorac Oncol 5: 260–274
Gralla RJ, Gatzemeier U, Gebbia V, Huber R, O'Brien M, Puozzo C (2007) Oral vinorelbine in the treatment of non-small cell lung cancer: rationale and implications for patient management. Drugs 67: 1403–1410
Greco FA, Spigel DR, Kuzur ME, Shipley D, Gray JR, Thompson DS, Burris HA, Yardley DA, Pati A, Webb CD, Gandhi JG, Hainsworth JD (2007) Paclitaxel/Carboplatin/gemcitabine versus gemcitabine/vinorelbine in advanced non-small-cell lung cancer: a phase II/III study of the Minnie Pearl Cancer Research Network. Clin Lung Cancer 8: 483–487
Gronberg BH, Bremnes RM, Flotten O, Amundsen T, Brunsvig PF, Hjelde HH, Kaasa S, von Plessen C, Stornes F, Tollali T, Wammer F, Aasebo U, Sundstrom S (2009) Phase III study by the Norwegian lung cancer study group: pemetrexed plus carboplatin compared with gemcitabine plus carboplatin as first-line chemotherapy in advanced non-small-cell lung cancer. J Clin Oncol 27: 3217–3224
Han JY, Lee DH, Song JE, Lee SY, Kim HY, Kim HT, Lee JS (2008) Randomized phase 2 study of irinotecan plus cisplatin versus gemcitabine plus vinorelbine as first-line chemotherapy with second-line crossover in patients with advanced nonsmall cell lung cancer. Cancer 113: 388–395
Harrell FE (2003) Hmisc S function library. http://hesweb1.med.virginia.edu/biostat/s/Hmisc.html. 2003. Ref Type: Electronic Citation
Jassem J, Kosmidis P, Ramlau R, Zarogoulidis K, Novakova L, Breton J, Etienne PL, Seebacher C, Grivaux M, Ojala A, Aubert D, Lefresne F (2003) Oral vinorelbine in combination with cisplatin: a novel active regimen in advanced non-small-cell lung cancer. Ann Oncol 14: 1634–1639
Jassem J, Ramlau R, Karnicka-Mlodkowska H, Krawczyk K, Krzakowski M, Zatloukal P, Lemarie E, Hartmann W, Novakova L, O'Brien M, Depierr A (2001) A multicenter randomized phase II study of oral vs. intravenous vinorelbine in advanced non-small-cell lung cancer patients. Ann Oncol 12: 1375–1381
Jensen LH, Osterlind K, Rytter C (2008) Randomized cross-over study of patient preference for oral or intravenous vinorelbine in combination with carboplatin in the treatment of advanced NSCLC. Lung Cancer 62: 85–91
Kubota K, Kawahara M, Ogawara M, Nishiwaki Y, Komuta K, Minato K, Fujita Y, Teramukai S, Fukushima M, Furuse K (2008) Vinorelbine plus gemcitabine followed by docetaxel versus carboplatin plus paclitaxel in patients with advanced non-small-cell lung cancer: a randomised, open-label, phase III study. Lancet Oncol 9: 1135–1142
Laack E, Dickgreber N, Muller T, Knuth A, Benk J, Lorenz C, Gieseler F, Durk H, Engel-Riedel W, Dalhoff K, Kortsik C, Graeven U, Burk M, Dierlamm T, Welte T, Burkholder I, Edler L, Hossfeld DK (2004) Randomized phase III study of gemcitabine and vinorelbine versus gemcitabine, vinorelbine, and cisplatin in the treatment of advanced non-small-cell lung cancer: from the German and Swiss Lung Cancer Study Group. J Clin Oncol 22: 2348–2356
Le LK, Myon E, Hill S, Riou-Franca L, Scott D, Sidhu M, Dunlop D, Launois R (2007) Comparative cost-minimisation of oral and intravenous chemotherapy for first-line treatment of non-small cell lung cancer in the UK NHS system. Eur J Health Econ 8: 145–151
Lilenbaum RC, Chen CS, Chidiac T, Schwarzenberger PO, Thant M, Versola M, Lane SR (2005) Phase II randomized trial of vinorelbine and gemcitabine versus carboplatin and paclitaxel in advanced non-small-cell lung cancer. Ann Oncol 16: 97–101
Liu G, Franssen E, Fitch MI, Warner E (1997) Patient preferences for oral versus intravenous palliative chemotherapy. J Clin Oncol 15: 110–115
Marty M, Fumoleau P, Adenis A, Rousseau Y, Merrouche Y, Robinet G, Senac I, Puozzo C (2001) Oral vinorelbine pharmacokinetics and absolute bioavailability study in patients with solid tumors. Ann Oncol 12: 1643–1649
O'Brien ME, Szczesna A, Karnicka H, Zatloukal P, Eisen T, Hartmann W, Kasan P, Longerey B, Lefresne F (2004) Vinorelbine alternating oral and intravenous plus carboplatin in advanced non-small-cell lung cancer: results of a multicentre phase II study 11. Ann Oncol 15: 921–927
Rajeswaran A, Trojan A, Burnand B, Giannelli M (2008) Efficacy and side effects of cisplatin- and carboplatin-based doublet chemotherapeutic regimens versus non-platinum-based doublet chemotherapeutic regimens as first line treatment of metastatic non-small cell lung carcinoma: a systematic review of randomized controlled trials. Lung Cancer 59: 1–11
Ramsey SD, Martins RG, Blough DK, Tock LS, Lubeck D, Reyes CM (2008) Second-line and third-line chemotherapy for lung cancer: use and cost. Am J Manag Care 14: 297–306
Reck M, von PJ, Zatloukal P, Ramlau R, Gorbounova V, Hirsh V, Leighl N, Mezger J, Archer V, Moore N, Manegold C (2010) Overall survival with cisplatin-gemcitabine and bevacizumab or placebo as first-line therapy for nonsquamous non-small-cell lung cancer: results from a randomised phase III trial (AVAiL). Ann Oncol 21: 1804–1809
Smith IE, O'Brien ME, Talbot DC, Nicolson MC, Mansi JL, Hickish TF, Norton A, Ashley S (2001) Duration of chemotherapy in advanced non-small-cell lung cancer: a randomized trial of three versus six courses of mitomycin, vinblastine, and cisplatin. J Clin Oncol 19: 1336–1343
Socinski MA, Schell MJ, Peterman A, Bakri K, Yates S, Gitten R, Unger P, Lee J, Lee JH, Tynan M, Moore M, Kies MS (2002) Phase III trial comparing a defined duration of therapy versus continuous therapy followed by second-line therapy in advanced-stage IIIB/IV non-small-cell lung cancer. J Clin Oncol 20: 1335–1343
Tan EH, Szczesna A, Krzakowski M, Macha HN, Gatzemeier U, Mattson K, Wernli M, Reiterer P, Hui R, Pawel JV (2005) Randomized study of vinorelbine-gemcitabine versus vinorelbine-carboplatin in patients with advanced non-small cell lung cancer. Lung Cancer 49: 233–240
Vokes EE, Rosenberg R, Jahanzeb M, Craig J, Gralla R, Belani C, Jones S, Bigley J, Hohneker J (1994) Oral vinorelbine (Navelbine) in the treatment of advanced non-small cell lung cancer: a preliminary report. Semin Oncol 21: 35–38
von Plessen C, Bergman B, Andresen O, Bremnes RM, Sundstrom S, Gilleryd M, Stephens R, Vilsvik J, Aasebo U, Sorenson S (2006) Palliative chemotherapy beyond three courses conveys no survival or consistent quality-of-life benefits in advanced non-small-cell lung cancer. Br J Cancer 95: 966–973
Yamamoto N, Nakagawa K, Uejima H, Sugiura T, Takada Y, Negoro S, Matsui K, Kashii T, Takada M, Nakanishi Y, Kato T, Fukuoka M (2006) Randomized phase II study of carboplatin/gemcitabine versus vinorelbine/gemcitabine in patients with advanced nonsmall cell lung cancer: West Japan Thoracic Oncology Group (WJTOG) 0104. Cancer 107: 599–605
Zhang L, Zhang Y, Li N, Xu F, Pan ZK, Guan ZZ (2004) [Gemcitabine plus cisplatin versus gemcitabine plus vinorelbine in treatment of advanced non-small cell lung cancer (NSCLC)]. Ai Zheng 23: 1455–1458
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Fløtten, Ø., Grønberg, B., Bremnes, R. et al. Vinorelbine and gemcitabine vs vinorelbine and carboplatin as first-line treatment of advanced NSCLC. A phase III randomised controlled trial by the Norwegian Lung Cancer Study Group. Br J Cancer 107, 442–447 (2012). https://doi.org/10.1038/bjc.2012.284
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.284
Keywords
This article is cited by
-
Trajectory of health-related quality of life during the last year of life in patients with advanced non-small–cell lung cancer
Supportive Care in Cancer (2022)
-
A comparison of CT based measures of skeletal muscle mass and density from the Th4 and L3 levels in patients with advanced non-small-cell lung cancer
European Journal of Clinical Nutrition (2019)
-
Assessment of proportional hazard assumption in aggregate data: a systematic review on statistical methodology in clinical trials using time-to-event endpoint
British Journal of Cancer (2018)
-
Can body composition be used to optimize the dose of platinum chemotherapy in lung cancer? A feasibility study
Supportive Care in Cancer (2017)
-
Methodology of health-related quality of life analysis in phase III advanced non-small-cell lung cancer clinical trials: a critical review
BMC Cancer (2016)