Abstract
To estimate the current occupational cancer burden due to past exposures in Britain, estimates of the number of exposed workers at different levels are required, as well as risk estimates of cancer due to the exposures. This paper describes the methods and results for estimating the historical exposures. All occupational carcinogens or exposure circumstances classified by the International Agency for Research on Cancer as definite or probable human carcinogens and potentially to be found in British workplaces over the past 20–40 years were included in this study. Estimates of the number of people exposed by industrial sector were based predominantly on two sources of data, the CARcinogen EXposure (CAREX) database and the UK Labour Force Survey. Where possible, multiple and overlapping exposures were taken into account. Dose–response risk estimates were generally not available in the epidemiological literature for the cancer–exposure pairs in this study, and none of the sources available for obtaining the numbers exposed provided data by different levels of exposure. Industrial sectors were therefore assigned using expert judgement to ‘higher’- and ‘lower’-exposure groups based on the similarity of exposure to the population in the key epidemiological studies from which risk estimates had been selected. Estimates of historical exposure prevalence were obtained for 41 carcinogens or occupational circumstances. These include exposures to chemicals and metals, combustion products, other mixtures or groups of chemicals, mineral and biological dusts, physical agents and work patterns, as well as occupations and industries that have been associated with increased risk of cancer, but for which the causative agents are unknown. There were more than half a million workers exposed to each of six carcinogens (radon, solar radiation, crystalline silica, mineral oils, non-arsenical insecticides and 2,3,7,8-tetrachlorodibenzo-p-dioxin); other agents to which a large number of workers are exposed included benzene, diesel engine exhaust and environmental tobacco smoke. The study has highlighted several industrial sectors with large proportions of workers potentially exposed to multiple carcinogens. The relevant available data have been used to generate estimates of the prevalence of past exposure to occupational carcinogens to enable the occupational cancer burden in Britain to be estimated. These data are considered adequate for the present purpose, but new data on the prevalence and intensity of current occupational exposure to carcinogens should be collected to ensure that future policy decisions be based on reliable evidence.
Similar content being viewed by others
Main
Doll and Peto (1981) estimated that about 4% of cancer deaths in the United States (with an uncertainty range from 2% to 8%) were due to occupational causes. If this percentage was applied to current cancer deaths in Britain, it would equate to ∼6000 deaths per annum (with a range of 3000–12, 000). However, there has been no systematic estimation of occupational cancer burden specific to Britain, and thus the relevance of these historical estimates of the cancer burden in the United States to the British situation is uncertain. The aim of this study, overviewed in Rushton et al (2010), was to provide an estimate of the burden of cancer in Britain due to occupational carcinogens or occupational circumstances that are definite or probable causes of cancer.
Estimates of current occupational cancer deaths and registrations are a consequence of past exposures to hazardous agents. However, many of these agents continue to be present in workplaces and may potentially cause deaths and illness in the future. These potential outcomes are preventable through interventions to reduce occupational exposure to carcinogens, but this requires targeting resources on those situations that contribute importantly to the burden. For this study, the underlying disease rates, prevalence of exposures and size of the potentially exposed population were required along with estimates of risk due to these exposures. These risk estimates are dependent on the intensity and duration of exposure in these populations. This paper describes the methods used for estimating the number of exposed workers and the results. Uncertainties in the estimated health impact arise because exposure–response studies often do not contain quantitative exposure estimates and rely on ordered categorical assessments of exposure whose meaning may differ from study to study. Consequently, the estimates of exposure prevalence used in this study were matched as closely as possible with existing exposure–response data for the most relevant epidemiological studies.
Methodology
Two criteria were used to determine whether an exposure was to be included in the analyses:
-
1)
Evidence for causality: substances or occupations in IARC Groups 1 and 2A with ‘strong’ evidence for carcinogenicity in humans for the cancer site being examined, as judged by Siemiatycki et al (2004).
-
2)
Evidence for the presence of the exposure within workplaces in Britain during the risk exposure period, that is, typically over the preceding 20 or 40 years depending on the likely latency of the cancer type.
These criteria were used to generate a list of cancer–exposure pairs that formed the basis of the assessment (Rushton et al, 2010).
One of the challenges for the exposure assessment was to avoid double counting of exposed workers with multiple, overlapping exposures, particularly where there were a large number of carcinogens involved. To identify overlapping and dominant exposures in the working population, an ‘exposure map’ was drawn up for the cancer sites. For a given cancer, the map entries comprise either an agent (or group of agents such as polycyclic aromatic hydrocarbons (PAHs)) or an exposure scenario (i.e., an industry or occupation in which such exposure may occur). The map for lung cancer was very complex because there were 32 exposures related to this cancer site (Figure 1). For other cancer sites, exposure maps were generally much simpler with fewer or no overlapping exposures. In Figure 1, agents are presented in plain type, whereas exposure scenarios are in italics. Lines joining boxes indicate where overlap could occur if all the entries in the map were simply considered separately. For example, if painters and asbestos were considered separately for lung cancer, overlap would occur in construction (these exposure scenarios are indicated in smaller print). Separate attributable fractions (AFs) have been estimated for substances and occupations that are shown in bold in the figure. For substances and occupations shown in boxes with dotted lines, a separate AF was not estimated, as these exposure scenarios were considered to be included with another exposure. Little is known about the possible toxicological interactions from coexposure to two or more agents. The methodology does not include any explicit allowance for synergistic or antagonistic effects from circumstances in which there is more than one agent present; however, if the risk estimates are derived from epidemiological studies undertaken in workplaces where there is coexposure (e.g., painting, welders), then such effects will be implicitly included.
For each cancer–exposure pairing, first the number of exposed workers within industrial sectors was estimated using a variety of sources, and second each industrial sector was assigned to a risk estimate based on the similarity of exposure intensity. This general methodology was applied to most of the exposure–cancer pairings, although alternative approaches were used for estimating the burden from exposure to asbestos and radon. These different approaches are described elsewhere (Hutchings and Rushton, 2012).
Number of exposed workers
To estimate the number of people exposed by industry, we relied predominantly upon two sources of data: the CARcinogen EXposure (CAREX) database (available at http://www.ttl.fi/en/chemical_safety/carex/pages/default.aspx; Kauppinen et al, 2000) and the UK Labour Force Survey (LFS; LFS, 2009). Other sources of information used included the Census of Employment (ONS, 2009) and industry-specific information, such as the number of female aircraft cabin crew in Britain.
CAREX has information for 139 carcinogens or carcinogenic circumstances, including all substances or mixtures that were in IARC Groups 1 and 2A when the database was compiled. Estimates of the number of exposed workers are available for the period 1990–1993 for the 15 countries that were members of the EU at that time, including Great Britain. Data for some of the newer member countries were added for 1997. The number of exposed workers is provided for each agent separately by industrial sector, as well as the total number of workers employed within each sector. The three-digit United Nations International Standard Industrial Classification (ISIC) revision 2 (1968) was used for manufacturing sectors, whereas for non-manufacturing sectors one- or two-digit ISIC codes were used. The CAREX estimates of the number of people exposed in Britain were based on data from Finland and the United States, adjusted using national employment statistics and reviewed by a British expert to ensure that it reflected national usage of chemicals and employment practice (Pannett et al, 1998). CAREX considered exposure by inhalation and dermal routes. The non-occupational background level was used as the minimum requirement for assigning occupational exposure (Kauppinen et al, 2000).
CAREX includes British estimates for 68 agents, classified by IARC for 830 combinations of agent and industry code. However, CAREX did not provide British estimates for all occupational and industrial circumstances classified by IARC as 1 or 2A; in these cases, we relied upon self-reported data from the LFS or the Census of Employment. The LFS is a Europe-wide household questionnaire survey that in Britain is undertaken by the Office for National Statistics (LFS, 2009). Its main purpose is to collect data on the UK labour market that can be used to develop, manage, evaluate and report on labour market policies. For our study, LFS estimates of the number of people employed in the specific jobs or industries, including all subdivisions by job status (manager, foreman or other) and gender, have been used. Data were available for the period from 1973 to 2003, and an appropriate year was chosen as a point estimate for estimating the proportion exposed depending on the latency of the cancer of concern (Hutchings and Rushton, 2012).
For some exposures, other sources of information were used to obtain estimates of the number of exposed workers. For example, the Central Index of Dose Information for ionising radiation (HSE, 1998) and data obtained from the British Airways Stewards and Stewardesses Union were used for estimating the number of workers exposed to ionising radiation.
Assignment of exposure levels
Dose–response estimates were generally not available in the epidemiological literature for the cancer–exposure pairs in this study. Where possible, risk estimates were obtained for an overall ‘lower’ level and an overall ‘higher’ level of exposure to the agents of concern. However, none of the sources available for obtaining the numbers exposed subdivided these data by different levels of exposure. At a workshop to discuss the methodology for estimating the burden of occupational cancer in Britain (HSE, 2007), a pragmatic decision was therefore taken to generally assign industrial sectors in CAREX into ‘higher’- and ‘lower’-exposure groups. In addition, for certain exposure–cancer pairs, the exposed population was assigned to a ‘background’ exposure level group, where exposure was considered to be comparable to non-occupational background levels. The exposure categories were not defined in terms of measured or estimated exposure levels; rather, industries were included in the higher, lower or background exposure category based on the similarity of exposure to the population in the key epidemiological study on which the risk estimate was based.
Two experienced occupational exposure experts (MvT and JWC) carried out this partitioning using information from the peer-reviewed literature together with data abstracted from the National Exposure Database (British National Exposure DataBase (NEDB)) held by the Health and Safety Executive (HSE; Burns and Beaumont, 1989). This database contains information on exposure measurements for about 70 different substances recorded in Britain over about the past 25 years, mostly from measurements recorded by HSE for compliance or for intelligence gathering. The majority of data were collected between 1986 and 2001 (about 80 000 measurements), with the number of measurements per substance ranging from >6000 (respirable quartz) to <5 (Cherrie et al, 2007). The data from NEDB and other sources, including the scientific literature, were used to judge whether risk estimates derived from epidemiological studies were likely to be from situations broadly comparable to conditions in Britain in the 1970s and 1980s.
Results
Following the review of the evidence and development of the exposure maps for each cancer, the cancer burden due to occupation was estimated for 41 exposures or exposure situations (Table 1). These included exposures to single chemical agents and metals, combustion products, other mixtures or groups of chemicals, mineral and biological dusts, physical agents and work patterns, as well as occupations and industries that have been associated with increased risk of cancer, but for which the causative agents are not known.
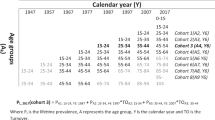
Tables 2 and 3 summarise the point estimates (e.g., 1990–1993 for CAREX) of the number of workers for each exposure–cancer pair who were exposed to levels for which the assigned relative risk (RR) estimate was >1, subdivided into high- and low-exposure groups. For some agents, no designation of the exposure levels is given in Table 2. This was either because there was just one exposure group, for example, leather dust, or because there were more than two RR estimates used in the calculations, and for simplicity the subdivisions are not shown, for example, aromatic amines. For some in the low-exposed group, the assigned RR was 1 and these workers were excluded from Tables 2 and 3, as they did not contribute to the attributable cancer burden. The number of exposed workers in Table 2 may therefore be lower for some agents than that provided by CAREX. For example, according to CAREX, 16 336 workers in the Great Britain were exposed to trichloroethylene in the period 1990–1993. However, a total of 721 workers were employed in industrial sectors, such as the beverage industry, tobacco industry and education services, and were not considered to be exposed at levels that are associated with an increased risk of developing cancer of the kidney or liver, or non-Hodgkin's lymphoma.
The estimated number of exposed workers provided in Tables 2 and 3 relate to different time periods, depending on which data source was used and the latency of the cancer site. For example, when using CAREX, the estimated number of workers given was only available for the period 1990–1993. In contrast, when using the LFS data, the numbers related to the year 1979 (for solid tumours with an assumed latency of 10–50 years and risk exposure period (REP) 1956–1995 (the REP is defined as the period during which exposure occurred that was relevant to the development of the cancer in the target year 2005) or 1991 (for haematopoietic cancers with an assumed latency of 0–20 years and REP of 1986–2005). For the solid tumours, an algorithm was developed to convert the CAREX estimates into estimates of the number of workers ever exposed during the REP, taking into account the staff turnover rate and changing patterns in the number of people employed in main industry groupings (Hutchings and Rushton, 2012). It is inappropriate to add the total number of workers exposed to carcinogens across cancer sites, because of potential double counting and because of the different time periods to which these data relate.
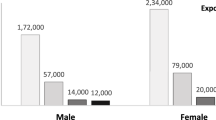
Table 2 indicates those agents with large numbers of exposed workers. A total of nearly 300 000 workers were considered to be exposed to benzene in the early 1990s at levels where there was an elevated risk of developing leukaemia. Nearly all were considered to be exposed to relatively low levels; relatively high exposure levels were only assigned for workers considered to be exposed to benzene in land transport and manufacture of industrial chemicals. In addition to exposure to benzene, agents with large numbers of workers exposed include radon (∼560,000 in 1990–1993), solar radiation (∼1.1 million in 1990–1993), silica (∼560,000 in 1990–1993), wood dust (∼430,000 in 1990–1993), mineral oils (∼1.3 million in 1979), non-arsenical insecticides (∼650,000 in 1991), 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD; ∼1.1 million in 1991), diesel exhaust fumes (∼470 000 in 1990–1993) and environmental tobacco smoke (∼360 000 in 1990–1993).
In addition, Table 3 shows that a considerable number of workers were employed in occupations or industries that have been linked with elevated cancer risks, including painters, hairdressers/barbers and welders.
For TCDD, ionising radiation (Table 2) and hairdressers (Table 3), the number of exposed workers varied by cancer site, because different data sources were used for cancers with long and short latencies. In the case of TCDD exposure, the number of exposed workers for lung cancer (a long latency cancer) was based on data from the LFS in 1979 and CoE in 1981, whereas for soft-tissue sarcoma and non-Hodgkin's lymphoma (short latency malignancies) LFS data from 1991 were used. Similarly, for hairdressers, the LFS data from 1979 were used for bladder cancer, but for non-Hodgkin's lymphoma LFS data from 1991 were used. The reason for this was that for soft-tissue sarcoma, non-Hodgkin's lymphoma and other haematopoietic malignancies the REP was set at 1986–2005, whereas for solid tumours the REP was 1956–1995. Hence, data from 1979 were considered to be most appropriate for solid cancers and data from 1991 for the haematopoietic neoplasms. Furthermore, the number of exposed workers for TCDD when considering non-Hodgkin's lymphoma was lower than that when considering soft-tissue sarcoma, as the group of farmers was excluded in order to avoid double counting with exposure to non-arsenic pesticides.
For PAH, fewer workers were considered to be exposed when considering lung and bladder cancer in comparison with non-melanoma skin cancer. The calculation for the AF for non-melanoma skin cancer from PAH exposure was based on the RR observed for the occupations of roofers, road surfacers, roadmen and pavers due to exposure to coal tars and pitches.
For a number of agents in Table 2 (i.e., formaldehyde, tetrachloroethylene, chromium, nickel, wood dust and mineral oil) that were linked to multiple cancer sites, the number of exposed workers used in the estimation of the AF for a cancer site may have been lower than that indicated in the table. The reason for this is that for some cancer sites the low-exposure group was assigned an RR of 1, whereas for others the low-exposure group had an RR of >1. For example, in the case of formaldehyde, the low-exposure group was also considered to be associated with an increased RR for leukaemia, whereas for nasopharyngeal and sinonasal cancer there was an increased risk assumed only for the workers in the high-exposed industries.
For a number of exposure–cancer pairs, the risk was gender dependent. For example, the epidemiological evidence for sinonasal cancer suggested that only males exposed to formaldehyde are at risk, and therefore female workers exposed to formaldehyde were excluded from the high-exposed group. Similarly, the risk of cervical cancer due to tetrachloroethylene is obviously confined to women.
Table 2 also shows the industrial sectors with 10% or more exposed workers for each carcinogen. There are several sectors where there was exposure to multiple carcinogens, both in manufacturing and in other sectors. In the manufacturing sector, industries with multiple exposures include the following:
-
i)
Manufacture of industrial chemicals: 1,3 butadiene, acrylamide, benzene, vinyl chloride monomer (VCM), arsenic, cadmium, cobalt, PAH, strong inorganic acid mists.
-
ii)
Manufacture of other chemical products: 1,3 butadiene, acrylamide, ethylene oxide, VCM, cobalt, strong inorganic acid mists.
-
iii)
Manufacture of machinery except electrical: tetrachloroethylene, trichloroethylene, arsenic, beryllium, chromium VI, cobalt, wood dust.
-
iv)
Manufacture of transport equipment: trichloroethylene, chromium VI, nickel, wood dust, solar radiation.
-
v)
Manufacture of fabricated metal products except machinery and equipment: trichloroethylene, chromium VI, cobalt, nickel, strong inorganic acid mists.
-
vi)
Manufacture of electrical machinery apparatus, appliances and supplies: trichloroethylene, arsenic, cadmium, inorganic lead, strong inorganic acid mists.
-
vii)
Non-ferrous basic metal industries: arsenic, cadmium, cobalt, inorganic lead, nickel, PAH, strong inorganic acid mists.
However, it should be noted that although these exposures all occurred within the same sector this does not necessarily mean that multiple exposures occurred within the same subgroup of workers.
Several non-manufacturing sectors were estimated to have had very high numbers of exposed workers, including the following:
-
i)
Agricultural sector: TCDD, non-arsenic insecticides, solar radiation;
-
ii)
Construction: tetrachloroethylene, arsenic, inorganic lead, diesel engine exhaust, soots, asbestos, silica, wood dust, solar radiation.
-
iii)
Land transport: benzene, tetrachloroethylene, diesel engine exhaust, wood dust, solar radiation.
-
iv)
Personal household services: aromatic amines, benzene, tetrachloroethylene, trichloroethylene, chromium VI, diesel engine exhaust.
-
v)
Wholesale and retail trade and restaurants and hotels: benzene, radon, environmental tobacco smoke, asbestos, solar radiation.
Discussion
This paper presents the methods and results of the exposure assessment carried out for the British occupational cancer burden study. The results suggest that there were high numbers of exposed workers for carcinogenic agents from natural sources (e.g., solar radiation and radon), pesticides, oils and mists, dusts and combustion fumes. The number of individuals exposed were somewhat lower for manufactured chemicals (with the exception of benzene), metals and physical agents (man-made). A relatively high number of individuals were at elevated risk from working as a painter, welder or hairdresser. Several industrial sectors have been highlighted where many workers were exposed potentially to multiple carcinogens.
Estimates of the number of exposed workers were based upon a variety of data sources, whereas estimates of the intensity of exposure were predominantly based upon expert assessment. The main source of exposure prevalence was the CAREX database, which is a European-wide database on the prevalence of occupational exposure to carcinogens that was developed in the early 1990s. A weakness of the CAREX system is that many of the estimates were inferred from Finnish and US data, and although a British expert reviewed the data (Pannett, 1998), it is very likely that some estimates were not accurate for the British situation. This may have resulted in either over- or underestimation of the number of exposed workers in Britain. When CAREX could not be used, for example, when the exposure was not included in CAREX or when the prevalence of workers in an occupation or industry was required, the UK LFS data were generally used. We recognise that the information from the LFS is not directly comparable to CAREX; the CAREX data relate to workers exposed to specific agents within industrial sectors, whereas the LFS is based on the number of people employed within an occupation.
Expert judgement was used to allocate industrial sectors within CAREX to high or low exposure categories, as the data do not provide a breakdown of differing levels of exposure within industries or the proportions exposed at these levels. Similarly, all those in specific occupations within the LFS were assumed exposed, and these will have included a proportion of individuals with very low, perhaps even background, exposure. Therefore, the estimated number of exposed workers from these sources may provide an overestimate or underestimate of the number of exposed workers. For the exposure situations linked to elevated cancer risk described in Table 3, this is not a major problem, because for these exposure situations risk estimates were used that were derived from population-based studies where the definition of the exposed population was broadly comparable to the definition used in the LFS survey (Hutchings and Rushton, 2012). For non-arsenical pesticide exposure, the risk estimates were based on studies of farmers in general, and therefore expected to include a similar proportion of farmers who are not exposed to non-arsenical pesticides as in the LFS data. For exposures to mineral oils, the risk estimates for the various cancer sites were obtained from case–control studies, some of which looked specifically at exposure to mineral oils (e.g., sinonasal cancer), and this may not be directly comparable to the definition of the exposed workers using the LFS data, even though the LFS data were assigned to exposure groups based on occupation code. High exposures were assigned to ‘Press and Machine Tool Setters’, ‘Other Centre Lathe Turners’, ‘Machine Tool Setter Operators’, ‘Machine Tool Operators’, ‘Press Stamping and Automatic Machine Operators’ and ‘Toolmakers Tool Fitters Markers-Out’, all of which were expected to have been exposed to relatively high levels of mineral oils.
The assignment of exposure intensity categories was relatively straightforward for some combinations of industry and substance. For example, the assignments of high exposure for tetrachloroethylene in the manufacture of metal products (degreasing) or personal and household services (dry cleaning) seem reliable (Gold et al, 2008). Jobs in the high category comprise about two-thirds of the total exposed population according to CAREX. However, the remaining exposed individuals are found in a disparate group of industries where the proportion of individuals exposed is generally very low and the use of tetrachloroethylene not immediately obvious, for example, 24 people from 9950 employed in tobacco manufacture (0.24%). These types of situations have generally been assigned to the low category on the assumption that the uses have generally been minor, but it is possible that in some cases this is incorrect. From the NEDB, we know that historically there were high exposures to tetrachloroethylene in British industry; 25% of the long-term measurements were above 26 p.p.m. (the current British Occupational Exposure Limit is 50 p.p.m.). There was, however, a similar proportion of the data where levels were low, with 25% of measurements <2 p.p.m. We consider the assumptions about the higher-exposure groups to be generally reliable; however, such errors may have underestimated the numbers assessed as more highly exposed.
In any binary classification of exposure, it is clear that there must be some threshold below which exposure is considered insufficient to be categorised. The researchers who developed CAREX discussed the difficulty in assigning low or background exposures, for example, where small amounts of carcinogens were used in laboratories, pharmacies or hospitals. In an earlier analysis (Cherrie et al, 2007), we showed that for 20 substances for which we had data on the numbers exposed from CAREX and from independent assessments by the British regulator, the HSE, there was a relatively good association between the two measures (r2=0.61 on the log-transformed data), but the CAREX estimates were about 2.5 times higher than the other data. We concluded that the official data represented higher-exposed workers, whereas CAREX represented a wider range of potentially exposed people.
The results presented in this paper related to the historical prevalence of exposed workers in Britain. Exposure levels to most manufactured chemical agents have significantly declined in Europe and North America in recent years (see for example Symanski et al, 1998; van Tongeren et al, 2000; Creely et al, 2007; Agostini et al, 2010), and the number of workers in the manufacturing sector has also declined. Therefore, the number of current workers exposed at levels where there is an elevated risk of developing cancer will be much smaller compared with that presented in this paper.
A key weakness in the assessment of occupational cancer burden has been the limited information available about the prevalence of occupational exposure to carcinogenic agents and the level at which people were exposed. CAREX and the LFS data have provided a reasonable basis to estimate current burden given the latency of the diseases involved. However, these data are much less appropriate for assessing the current number of people at work who are exposed to carcinogens. This information is necessary if we are to intervene effectively to reduce the future occupational cancer burden, and there is therefore an urgent need to update CAREX to provide current data on the prevalence of exposure including estimates of the level of exposure in workplaces in Britain and throughout the European Union.
One new opportunity to obtain reliable data is to collate evidence that has and will continue to be produced to support registration and authorisation of manufactured chemicals under the European REACH Regulations (Registration, Evaluation, Authorisation and Restriction of Chemicals). Chemicals identified as substances of very high concern, such as carcinogenic substances, may be subject to authorisation. The process of seeking authorisation will require an assessment of the risks for the substances ‘in use’, to ensure that they are either adequately controlled or their continued use can be justified by socio-economic benefits. This will require data on the number of individuals exposed, the level of exposure, the circumstances of use, control measures and other information relevant to assessment of occupational cancer burden. It would be very valuable if these data could be centrally collated and made available to researchers and policy makers.
Clearly, REACH does not cover all workplace carcinogens. Physical agents such as sunlight, process-generated emissions such as diesel engine exhaust particulate and exposure circumstances such as painting are not covered by REACH. It will therefore be necessary to identify alternative ways of collecting appropriate intelligence on these carcinogenic exposures to ensure that in the future we have an improved understanding of the risk for occupational cancer. These data collection initiatives could best be achieved through a partnership between government, industry and other interested parties. Reliable data on current prevalence and intensity of occupational exposure to carcinogens will ensure that future policy decisions are based on reliable evidence.
References
Agostini M, de Vocht F, van Tongeren M, Cherrie JW, Galea KS, Kromhout H, and on Behalf of the EU-EXASRUB Consortium (2010) Exposure to rubber process dust and fume since 1970s in the United Kingdom. The influence of origin of the measurement data. J Environ Monit 12 (5): 1170–1178
Burns DK, Beaumont PL (1989) The HSE National Exposure Database (NEDB). Ann Occup Hyg 33 (1): 1–14
Cherrie JW, Van Tongeren M, Semple S (2007) Exposure to occupational carcinogens in Great Britain. Ann Occup Hyg 51 (8): 653–664
Creely K, Cowie H, van Tongeren M, Kromhout H, Tickner J, Cherrie J (2007) Trends in inhalation exposure – a review of the data in the published literature. Ann Occup Hyg 51: 665–678
Doll R, Peto R (1981) The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States today. J Nat Cancer Inst 66 (6): 1191–1308
Gold L, De Roos A, Waters M, Stewart P (2008) Systematic literature review of uses and levels of occupational exposure to tetrachloroethylene. J Occup Environ Hyg 5 (12): 807–839
HSE (1998) Occupational exposure to ionising radiation 1990–1996. Analysis of doses reported to the Health and Safety Executive's Central Index of Dose Information
HSE (2007) Burden of occupational cancer in Great Britain: summary report of cancer epidemiology workshop held on 27 and 28 June 2006. Report HSL/2007/32. http://www.hse.gov.uk/research/hsl_pdf/2007/hsl0732.pdf
Hutchings SJ, Rushton L (2012) Occupational cancer in Britain: Statistical methodology. Br J Cancer 107 (Suppl 1): S8–S17
Kauppinen T, Toikkanen J, Pedersen D, Young R, Ahrens W, Boffetta P, Hansen J, Kromhout H, Maqueda Blasco J, Mirabelli D, de la Orden-Rivera V, Pannett B, Plato N, Savela A, Vincent R, Kogevinas M (2000) Occupational exposure to carcinogens in the European Union. Occup Environ Med 57 (1): 10–18
Labour Force Survey (LFS) (2009) Available at: http://www.statistics.gov.uk/
ONS (2009) Census of employment. Available at: https://www.nomisweb.co.uk/
Pannett B, Kauppinen T, Toikkanen J, Pedersen J, Young R, Kogevinas M (1998) Occupational exposure to carcinogens in Great Britain in 1990–1993: preliminary results. In CAREX: International Information System on Occupational Exposure to Carcinogens. Finnish Institute of Occupational Health: Helsinki. Available at: http://www.ttl.fi/en/chemical_safety/carex/Pages/default.aspx (accessed April 2012)
Rushton L, Bagga S, Bevan R, Brown TP, Cherrie JW, Holmes P, Fortunato L, Slack R, Van Tongeren M, Young C, Hutchings SJ (2010) Occupation and cancer in Britain. Br J Cancer 102 (9): 1428–1437
Siemiatycki J, Richardson L, Straif K, Latreille B, Lakhani R, Sally Campbell S, Rousseau MC, Paolo Boffetta P (2004) Listing occupational carcinogens. Environ Health Perspec 112 (5): 1447–1459
Symanski E, Kupper LL, Hertz-Piciotto I, Rappaport SM (1998) Comprehensive evaluation of long term trends in occupational exposure: part 2. Predictive models for declining exposures. Occup Environ Med 55: 310–316
van Tongeren MJA, Kromhout H, Gardiner K (2000) Trends in levels of inhalable dust exposure, exceedance and overexposure in the European carbon black manufacturing industry. Ann Occup Hyg 44: 271–280
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Van Tongeren, M., Jimenez, A., Hutchings, S. et al. Occupational cancer in Britain. Br J Cancer 107 (Suppl 1), S18–S26 (2012). https://doi.org/10.1038/bjc.2012.114
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.114
Keywords
This article is cited by
-
Absence of multiplicative interactions between occupational lung carcinogens and tobacco smoking: a systematic review involving asbestos, crystalline silica and diesel engine exhaust emissions
BMC Public Health (2017)
-
Occupational cancer burden in Great Britain
British Journal of Cancer (2012)
-
Occupational cancer in Britain
British Journal of Cancer (2012)
-
Occupational cancer in Britain
British Journal of Cancer (2012)