Abstract
Background:
YKL-40 and C-reactive protein (CRP) are biomarkers that may reflect cancer-related subclinical inflammation. We assessed elevated YKL-40 and CRP levels as combined risk predictors for cancer.
Methods:
We measured plasma YKL-40 and CRP at baseline in 8706 individuals from the Danish general population.
Results:
Hazard ratio (HR) of gastrointestinal cancer for a doubling of YKL-40 levels was 1.37 (95% CI: 1.17–1.61) and indifferent to adjustment for CRP levels. Hazard ratio of lung cancer for a doubling of CRP levels was 1.35 (1.17–1.56) and indifferent to adjustment for YKL-40 levels. Compared to individuals with both low CRP (<1.7 mg l−1) and YKL-40 (<154 μg l−1), individuals with high YKL-40 but low CRP had an HR of gastrointestinal cancer of 3.36 (1.70–6.64), whereas individuals with high CRP but low YKL-40 had an HR of lung cancer of 2.19 (1.24–3.87). The area under the receiver operating characteristic (ROC) curve was 0.68 for the ability of YKL-40 to predict gastrointestinal cancer and 0.67 for the ability of CRP to predict lung cancer.
Conclusion:
Elevated YKL-40 levels are associated with increased risk of gastrointestinal cancer, independently of CRP levels, whereas elevated CRP levels are associated with increased risk of lung cancer, independently of YKL-40 levels.
Similar content being viewed by others
Main
C-reactive protein (CRP) is a well-known acute-phase reactant that is produced in the liver in response to elevated cytokine levels after an inflammatory stimulus (Pepys and Hirschfield, 2003; Johnson, 2006). Individuals with slightly elevated CRP levels from 2 to 3 mg l−1 and above have an increased risk of cardiovascular disease, but also of several other diseases and all-cause mortality (Erlinger et al, 2004; Il’yasova et al, 2005; Gunter et al, 2006; Otani et al, 2006; Siemes et al, 2006; Trichopoulos et al, 2006; Allin et al, 2009; Nordestgaard, 2009; Marott et al, 2010; Zacho et al, 2010a, 2010b). YKL-40 is a newly discovered plasma protein that – like CRP – is elevated during inflammatory conditions and cancer (Cintin et al, 1999; Nordenbaek et al, 1999; Vos et al, 2000; Ostergaard et al, 2002; Johansen et al, 2004, 2009b). However, whereas CRP is produced in the liver, YKL-40 is produced at the site of pathology by different cells, including cancer cells and cancer-associated macrophages (Junker et al, 2005; Johansen et al, 2009b).
Chronic inflammation and cancer are associated: many solid cancers arise at sites of chronic inflammation and many solid cancers induce themselves an inflammatory response in the tumour microenvironment (Balkwill and Mantovani, 2001; Coussens and Werb, 2002; Colotta et al, 2009). Irrespective of the origin of the cancer-related inflammation, it is likely to result in elevated plasma levels of inflammatory proteins, which may therefore act as biomarkers of cancer. Numerous inflammatory biomarkers exist, but as we aimed to examine both the central and the peripheral response to inflammation, we chose to focus on a combination of an acute-phase protein produced centrally in the liver, that is, CRP, and a protein produced at the site of the inflammation itself, that is, YKL-40. Presently, it is unknown whether CRP and YKL-40 potentially could complement each other in cancer risk prediction.
In this observational cohort study of the general population, we did not seek to evaluate the aetiological aspects of an association between CRP, YKL-40, and cancer risk, but rather considered CRP and YKL-40 as biomarkers reflecting cancer-related subclinical inflammation. Thus, we first examined whether elevated levels of YKL-40 and CRP are mutually independent risk predictors for gastrointestinal, lung, and any cancer. Second, we examined whether YKL-40 and CRP levels combined better predict these risks than either one alone. And finally, we examined the predictive ability of CRP and YKL-40 by using receiver operating characteristics (ROC) curves. For these purposes, we used a prospective study of the Danish general population, the Copenhagen City Heart Study, in which plasma levels of both YKL-40 and CRP were measured at baseline in 8706 individuals who were followed for up to 18 years (Allin et al, 2009; Johansen et al, 2009a).
Materials and methods
Participants
We studied individuals from the Copenhagen City Heart Study, which is a prospective cohort study of the Danish general population (Schnohr et al, 2002; Nordestgaard et al, 2007). It was initiated in 1976–1978, with follow-up examinations in 1981–1983, 1991–1994, and 2001–2003. Participants in this study are from the 1991–1994 examination, where 16 563 individuals were invited and 10 135 individuals participated. Data collection from the 1991–1994 examination included a self-administered questionnaire, which was reviewed by an investigator at the day of attendance, a physical examination, and blood samples for biochemical analyses. Plasma samples were frozen at −80°C and were used for measurement of CRP and YKL-40 as described below. Height and weight were directly measured at the physical examination, whereas information about covariates such as smoking and alcohol consumption were obtained from the questionnaires. We excluded individuals without a measurement of CRP or YKL-40 due to unavailability of blood (n=1259). Furthermore, we excluded individuals with cirrhosis (n=105) (cirrhosis distorts levels of both CRP and YKL-40) and with incomplete information about smoking, alcohol consumption, or body mass index (n=65). Thus, we included 8706 individuals aged 21–93 years. Follow-up time for incident cancer began at blood sampling and ended at occurrence of cancer, death, emigration, or May 2009, whichever came first. We excluded individuals with a diagnosis of lung cancer (n=18), gastrointestinal cancer (n=83), or any cancer (n=444) before blood sampling from the analysis of the respective cancer types. Mean follow-up period was 13 years (range=0–18 years). Follow-up was 100% complete, that is, we did not loose track of even a single individual.
Outcome measures
Cancer diagnoses from 1943 through May 2009 were obtained from the National Danish Cancer Registry (Storm, 1988, 1991; Storm et al, 1997) and from the National Danish Patient Registry. Diagnoses were classified according to the World Health Organization International Classification of Diseases, Seventh revision (ICD-7) or Tenth revision (ICD-10). The lung cancer diagnosis included cancer of the bronchies and lungs (98% of cancers in the lung cancer category) and cancer of pleura and mediastinum (2% of cancers in the lung cancer category). The gastrointestinal cancer diagnosis included cancer of the oral cavity, pharynx, oesophagus, stomach, small intestine, liver, biliary tract, pancreas, colon, rectum, and anus. The diagnosis of any cancer included any cancer diagnosis, except for non-melanoma skin cancer. Dates of deaths were obtained from the National Danish Civil Registration System.
Ethics
The ethical committee of Copenhagen and Frederiksberg, Denmark approved the study (KF-100.2039/91). All participants gave written informed consent.
CRP and YKL-40 analysis
We determined the CRP and YKL-40 levels in the plasma stored at −80°C for 12–15 years. C-reactive protein was measured by a high-sensitivity turbidimetry assay (Dako, Glostrup, Denmark), assessed daily for precision (Allin et al, 2009). YKL-40 was measured in duplicates by a commercial two-site sandwich-type enzyme-linked immunosorbent assay (Quidel Corporation, San Diego, CA, USA) (Harvey et al, 1998; Johansen et al, 2009a), assessed daily for precision.
Statistical analysis
We analysed data using the STATA statistical software (version 10.1; StataCorp, College Station, TX, USA), and a two-sided P-value <0.05 was considered statistically significant. We used logarithmic base 2 transformations of the CRP and YKL-40 levels to estimate risk of cancer for a doubling of CRP and YKL-40 levels; we chose this approach rather than an earlier one with YKL-40 in 10 years age percentile categories (Johansen et al, 2009a), because we then used the same statistical approach for CRP and YKL-40 and because our use of age as the time scale in Kaplan–Meier curves and Cox proportional hazards regression models (see below) results in an optimal and precise adjustment for age, which makes the stratification by 10 years age groups redundant. Furthermore, we divided individuals into four categories based on of their CRP and YKL-40 levels. On the basis of previous knowledge, we used the median as cutoff value for CRP levels (1.7 mg l−1) and the 90% percentile as cutoff value for YKL-40 levels (154 μg l−1) (Allin et al, 2009; Johansen et al, 2009a). Thus, four categories were generated: CRP <1.7 mg l−1 and YKL-40 <154 μg l−1, CRP ⩾1.7 mg l−1 and YKL-40 <154 μg l−1, CRP <1.7 mg l−1 and YKL-40 ⩾154 μg l−1, and CRP ⩾1.7 mg l−1 and YKL-40 ⩾154 μg l−1.
We used the Kaplan–Meier method to plot cumulative incidence of cancer against age and used the log-rank test to test for differences between categories. We used Cox proportional hazards regression models to estimate hazard ratios (HRs) of cancer as a function of CRP and YKL-40 levels. To automatically adjust for age, we used left truncation and age as time scale. In addition, HRs were adjusted for sex, smoking status (never, former, or current smoker), smoking dose (cigarettes or equivalent per day), alcohol consumption (women: ⩽168 or >168 g per week; men: ⩽252 or >252 g per week), and body mass index (<18.5, 18.5–24.9, 25–29.9, or ⩾30.0 kg m−2). To examine whether elevated CRP and YKL-40 levels are mutually independent risk predictors, we used likelihood ratio tests to compare statistical models including one or both biomarkers. The likelihood ratio test comparing the model including only CRP levels with the model that includes both CRP and YKL-40 levels evaluated whether the model with YKL-40 levels had more ability to predict/explain cancer risk than the model without. Statistical significance of this test means that elevated YKL-40 levels are a risk predictor, independent of CRP levels. Likewise, the likelihood ratio test comparing the model including only YKL-40 levels with the model that includes both YKL-40 and CRP levels evaluated whether the model with CRP levels had more ability to predict/explain cancer risk than the model without. Statistical significance of this test means that elevated CRP levels are a risk predictor, independent of YKL-40 levels.
We tested the Cox proportional hazards assumption graphically. Any indication of non-conformity to proportional hazards assumptions led to further examination with a test based on Schoenfeld residuals. We detected no major violations. For logarithmic base 2 (log 2) transformations of CRP and YKL-40 levels, we assumed linearity between log 2 (CRP levels), respectively, log 2 (YKL-40 levels) and the log-hazards of cancer. We tested this assumption by computing a likelihood ratio test comparing a quadratic model to a linear model and detected no signs of nonlinearity.
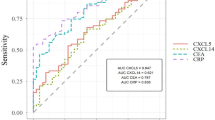
The predictive ability of CRP and YKL-40 in the prediction of lung cancer, gastrointestinal cancer, and any cancer was estimated as the area under the curve from ROC curves. Sensitivity was calculated as the number of true positives/(number of true positives+false negatives) and specificity was calculated as the number of true negatives/(number of true negatives+false positives).
Results
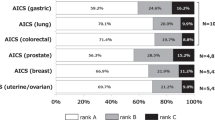
Characteristics of participants at blood sampling are listed in Table 1. Figure 1 demonstrates a different distribution of CRP and YKL-40 levels, that is, some individuals have high CRP levels but low YKL-40 levels, and vice versa. Hazard ratios of lung cancer, gastrointestinal cancer, and any cancer for a doubling of CRP or YKL-40 levels were attenuated with increasing follow-up time (Supplementary Figure 1). In consequence, we censored individuals at 5 years after blood sampling when calculating HRs of incident cancer. Thus, HRs presented below are HRs of cancer that occurred within the first 5 years after blood sampling. Hazard ratios of cancer that occurred within the full period of follow-up are presented in Supplementary Table 1. Likewise, data on predictive ability of CRP and YKL-40 are based on cancers that occurred within the first 5 years after blood sampling.
YKL-40 levels by CRP levels in 8706 individuals from the general population. The horizontal red line depicts the median CRP level=1.7 mg l−1. The vertical red line depicts the 90% percentile for YKL-40 levels=154 μg l−1. From these values, four categories were generated based on combinations of high and low levels of CRP and YKL-40. The colour reproduction of this figure is available at British Journal of Cancer online.
Lung cancer
The multifactorially adjusted HR of lung cancer for a doubling of CRP levels was 1.35 (95% CI: 1.17–1.56), while further adjustment for YKL-40 levels resulted in a similar HR of 1.35 (1.16–1.57) (Figure 2; likelihood ratio test between models, P=0.99). The corresponding HR for a doubling of YKL-40 levels was 1.10 (0.90–1.36), while further adjustment for CRP levels resulted in an HR of 1.00 (0.80–1.25) (Figure 2; P<0.001). This means that elevated CRP levels are a risk predictor for lung cancer, independent of YKL-40 levels.
Risk of cancer by CRP or YKL-40 levels in the general population. Multifactorial adjustment included age, sex, smoking, alcohol consumption, and body mass index. P-values from likelihood ratio tests examine whether inclusion of YKL-40 levels/CRP levels in the statistical model improves the fit of the statistical model to the data.
The cumulative incidence of lung cancer as a function of age increased with increasing levels of CRP and YKL-40 (Figure 3; log-rank, P<0.001). Multifactorially adjusted HRs of lung cancer were 2.19 (1.24–3.87) for individuals with CRP ⩾1.7 mg l−1 and YKL-40 <154 μg l−1, 1.08 (0.25–4.72) for individuals with CRP <1.7 mg l−1 and YKL-40 ⩾154 μg l−1, and 2.58 (1.23–5.41) for individuals with CRP ⩾1.7 mg l−1 and YKL-40 ⩾154 μg l−1 compared to individuals with CRP <1.7 mg l−1 and YKL-40 <154 μg l−1 (Figure 3).
Cumulative incidence of cancer by CRP and YKL-40 levels in the general population. Green line: CRP <1.7 mg l−1, YKL-40 <154 μg l−1; blue line: CRP ⩾1.7 mg l−1, YKL-40 <154 μg l−1; cyan line: CRP <1.7 mg l−1, YKL-40 ⩾154 μg l−1, and red line: CRP ⩾1.7 mg l−1, YKL-40 ⩾154 μg l−1. Hazard ratios were multifactorially adjusted for age, sex, smoking, alcohol consumption, and body mass index. CI=confidence interval. The colour reproduction of this figure is available at British Journal of Cancer online.
The sensitivity and specificity of CRP ⩾1.7 mg l−1 was 79 and 49% (Table 2). The corresponding values for YKL-40 ⩾154 μg l−1 was 19 and 90% (Table 2). The area under the ROC curve was 0.67 for CRP and 0.64 for YKL-40 (Figure 4). By maximising both sensitivity and specificity for prediction of lung cancer, a cut-point of 2.1 mg l−1 was identified for levels of CRP (sensitivity and specificity both 61%) and of 68.6 μg l−1 for levels of YKL-40 (sensitivity and specificity both 62%).
Gastrointestinal cancer
The multifactorially adjusted HR of gastrointestinal cancer for a doubling of YKL-40 levels was 1.37 (95% CI: 1.17–1.61), while further adjustment for CRP levels resulted in a similar HR of 1.36 (1.15–1.60) (Figure 2; likelihood ratio test between models, P=0.77). The corresponding HR for a doubling of CRP levels was 1.09 (0.94–1.26), while further adjustment for YKL-40 levels resulted in an HR of 1.02 (0.88–1.19) (Figure 2; P<0.001). This means that elevated YKL-40 levels are a risk predictor for gastrointestinal cancer, independent of CRP levels.
The cumulative incidence of gastrointestinal cancer as a function of age increased with increasing levels of CRP and YKL-40 (Figure 3; log-rank, P<0.001). Multifactorially adjusted HRs of gastrointestinal cancer were 1.48 (0.95–2.29) for individuals with CRP ⩾1.7 mg l−1 and YKL-40 <154 μg l−1, 3.36 (1.70–6.64) for individuals with CRP <1.7 mg l−1 and YKL-40 ⩾154 μg l−1, and 2.41 (1.37–4.24) for individuals with CRP ⩾1.7 mg l−1 and YKL-40 ⩾154 μg l−1 compared to individuals with CRP <1.7 mg l−1 and YKL-40 <154 μg l−1 (Figure 3).
The sensitivity and specificity of CRP ⩾1.7 mg l−1 was 66 and 49% (Table 2). The corresponding values for YKL-40 ⩾154 μg l−1 was 27 and 90% (Table 2). The area under the ROC curve was 0.60 for CRP and 0.68 for YKL-40 (Figure 4). By maximising both sensitivity and specificity for prediction of gastrointestinal cancer, a cut-point of 1.8 mg l−1 was identified for levels of CRP (sensitivity and specificity both 54%) and of 69.0 μg l−1 for levels of YKL-40 (sensitivity and specificity both 63%).
Any cancer
Excluding cancers in the categories of lung cancer and gastrointestinal cancer, the major cancers in the category of any cancer were breast cancer (15% of any cancers), prostate cancer (9%), bladder and urinary tract cancer (4%), melanoma (4%), metastases with unknown primary tumour (4%), corpus uteri cancer (3%), cancer of the ovary and female genital organs (3%), and leukaemia (3%).
The multifactorially adjusted HR of any cancer for a doubling of CRP levels was 1.15 (95% CI: 1.07–1.24), while further adjustment for YKL-40 levels resulted in a similar HR of 1.14 (1.05–1.23) (Figure 2; likelihood ratio test between models, P=0.26). The corresponding HR for a doubling of YKL-40 levels was 1.09 (1.00–1.20), while further adjustment for CRP levels resulted in an HR of 1.06 (0.96–1.16) (Figure 2; P<0.001). This means that elevated CRP levels are a risk predictor for any cancer, independent of YKL-40 levels.
The cumulative incidence of any cancer as a function of age increased with increasing levels of CRP and YKL-40 (Figure 3; log-rank, P<0.001). Multifactorially adjusted HRs of any cancer were 1.40 (1.13–1.73) for individuals with CRP ⩾1.7 mg l−1 and YKL-40 <154 μg l, 1.54 (0.98–2.43) for individuals with CRP <1.7 mg l and YKL-40 ⩾154 μg l, and 1.62 (1.18–2.23) for individuals with CRP ⩾1.7 mg l and YKL-40 ⩾154 μg l compared to individuals with CRP <1.7 mg l and YKL-40 <154 μg l (Figure 3).
The sensitivity and specificity of CRP ⩾1.7 mg l was 66 and 50% (Table 2). The corresponding values for YKL-40 ⩾154 μg l was 17 and 91% (Table 2). The area under the ROC curve was 0.61 for CRP and 0.62 for YKL-40 (Figure 4). Maximising both sensitivity and specificity for prediction of any cancer, a cut-point of 1.9 mg /l−1 was identified for levels of CRP (sensitivity and specificity both 57%) and of 62.0 μg l−1 for levels of YKL-40 (sensitivity and specificity both 59%).
Discussion
In this prospective cohort study of the Danish general population, we observed that elevated YKL-40 levels were associated with an increased risk of gastrointestinal cancer, independently of CRP levels, and that elevated CRP levels were associated with an increased risk of lung cancer, independently of YKL-40 levels. These findings are novel.
The results of this study indicate that the combined use of YKL-40 and CRP does not necessarily improve the prediction ability of either CRP or YKL-40 alone. Although elevated YKL-40 levels were associated with increased risk of gastrointestinal cancer, independently of CRP levels, CRP levels were not related to gastrointestinal cancer risk. These observations mean that YKL-40 alone is enough to predict gastrointestinal cancer risk. A similar issue can be pointed out in the association of CRP and YKL-40 with lung cancer that the present results merely imply that CRP alone is enough to predict lung cancer risk. The complementary and mutually independent associations between CRP and lung cancer, respectively, YKL-40 and gastrointestinal cancer are intriguing. First, although CRP and YKL-40 levels are increased during similar clinical conditions in response to elevated levels of interleukin-6 (Cintin et al, 1999; Nordenbaek et al, 1999; Vos et al, 2000; Ostergaard et al, 2002; Pepys and Hirschfield, 2003; Johansen et al, 2004, 2009b; Johnson, 2006; Nielsen et al, 2011), CRP and YKL-40 are produced by different cell types and in different parts of the body. Thus, CRP is produced in the liver, whereas YKL-40 is produced at the site of pathology by different cells, including cancer cells and cancer-associated macrophages (Pepys and Hirschfield, 2003; Junker et al, 2005; Johnson, 2006; Johansen et al, 2009b). Second, cancer is not a single entity, but rather a collection of diseases, each characterised by individual pathogenesis, which might be reflected in the plasma.
Although we cannot evaluate the aetiological aspects of an association between CRP, YKL-40, and cancer risk in this observational cohort study of the general population, several biological mechanisms may account for the observed associations. One could speculate that elevated CRP levels closely reflect the extent of pulmonary inflammation. Causes of pulmonary inflammation include smoking, asthma, and chronic lung infections, conditions that are all associated with an increased risk of lung cancer (Engels, 2008). Another cause of pulmonary inflammation is the presence of occult lung cancer (Balkwill and Mantovani, 2001; Coussens and Werb, 2002; Colotta et al, 2009). Thus, the association between elevated CRP levels and risk of lung cancer could represent confounding by pulmonary inflammation or reverse causation by occult lung cancer. It seems unlikely that elevated CRP levels play a causal role in the pathogenesis of lung cancer, as three former studies found that single-nucleotide polymorphisms in the CRP gene that are associated with increased circulating CRP levels were not associated with an increased risk of lung cancer (Siemes et al, 2006; Allin et al, 2010; Chaturvedi et al, 2010).
As the biological function of YKL-40 is poorly understood and as genetic studies like those mentioned above do not exist for YKL-40, we cannot exclude that YKL-40 could play a causal role in the pathogenesis of gastrointestinal cancer. However, at this stage, we consider it more likely that YKL-40 is a mere marker of gastrointestinal cancer. Thus, chronic gastrointestinal inflammation is a well-known risk predictor for gastrointestinal cancer (Balkwill and Mantovani, 2001; Coussens and Werb, 2002), and YKL-40 levels could closely reflect the amount of gastrointestinal inflammation. Furthermore, in accordance with the observation that gastrointestinal cancers are typically surrounded by extensive inflammation and some fibrosis, we speculate that YKL-40, which is a growth factor of fibroblasts (Recklies et al, 2002), is secreted in large amounts by gastrointestinal cancer cells. Thus, the association between elevated YKL-40 levels and increased risk of gastrointestinal cancer could represent confounding by gastrointestinal inflammation or reverse causation by occult gastrointestinal cancer.
Sensitivity and specificity of CRP for predicting lung cancer was both 61% when using a cut-point of 2.1 mg l−1, whereas corresponding values for YKL-40 in risk prediction of gastrointestinal cancer were 63% using a cut-point of 69.0 μg l−1. Although these values may not seem high, they are in fact comparable to the sensitivity and specificity of low-density lipoprotein cholesterol for prediction of ischemic cardiovascular events (Benn et al, 2007).
The interpretation of our data is potentially limited by our amalgamation of heterogeneous cancer types into the three outcome measures lung cancer, gastrointestinal cancer, and any cancer; however, we did not have sufficient statistical power to examine the risk of individual cancer types.
In conclusion, we have demonstrated that elevated YKL-40 levels are associated with increased risk of gastrointestinal cancer, independently of CRP levels and that elevated CRP levels are associated with increased risk of lung cancer, independently of YKL-40 levels.
Change history
29 March 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Allin KH, Bojesen SE, Nordestgaard BG (2009) Baseline C-reactive protein is associated with incident cancer and survival in patients with cancer. J Clin Oncol 27: 2217–2224
Allin KH, Nordestgaard BG, Zacho J, Tybjaerg-Hansen A, Bojesen SE (2010) C-reactive protein and the risk of cancer: a Mendelian randomization study. J Natl Cancer Inst 102: 202–206
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357: 539–545
Benn M, Nordestgaard BG, Jensen GB, Tybjaerg-Hansen A (2007) Improving prediction of ischemic cardiovascular disease in the general population using apolipoprotein B: the Copenhagen City Heart Study. Arterioscler Thromb Vasc Biol 27: 661–670
Chaturvedi AK, Caporaso NE, Katki HA, Wong H, Chatterjee N, Pine SR, Chanock SJ, Goedert JJ, Engels EA (2010) C-reactive protein and risk of lung cancer. J Clin Oncol 28: 2719–2726
Cintin C, Johansen JS, Christensen IJ, Price PA, Sorensen S, Nielsen HJ (1999) Serum YKL-40 and colorectal cancer. Br J Cancer 79: 1494–1499
Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A (2009) Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis 30: 1073–1081
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420: 860–867
Engels EA (2008) Inflammation in the development of lung cancer: epidemiological evidence. Expert Rev Anticancer Ther 8: 605–615
Erlinger TP, Platz EA, Rifai N, Helzlsouer KJ (2004) C-reactive protein and the risk of incident colorectal cancer. JAMA 291: 585–590
Gunter MJ, Stolzenberg-Solomon R, Cross AJ, Leitzmann MF, Weinstein S, Wood RJ, Virtamo J, Taylor PR, Albanes D, Sinha R (2006) A prospective study of serum C-reactive protein and colorectal cancer risk in men. Cancer Res 66: 2483–2487
Harvey S, Weisman M, O’Dell J, Scott T, Krusemeier M, Visor J, Swindlehurst C (1998) Chondrex: new marker of joint disease. Clin Chem 44: 509–516
Il’yasova D, Colbert LH, Harris TB, Newman AB, Bauer DC, Satterfield S, Kritchevsky SB (2005) Circulating levels of inflammatory markers and cancer risk in the health aging and body composition cohort. Cancer Epidemiol Biomarkers Prev 14: 2413–2418
Johansen JS, Bojesen SE, Mylin AK, Frikke-Schmidt R, Price PA, Nordestgaard BG (2009a) Elevated plasma YKL-40 predicts increased risk of gastrointestinal cancer and decreased survival after any cancer diagnosis in the general population. J Clin Oncol 27: 572–578
Johansen JS, Drivsholm L, Price PA, Christensen IJ (2004) High serum YKL-40 level in patients with small cell lung cancer is related to early death. Lung Cancer 46: 333–340
Johansen JS, Schultz NA, Jensen BV (2009b) Plasma YKL-40: a potential new cancer biomarker? Fut Oncol 5: 1065–1082
Johnson AM (2006) Amino acids, peptides, and proteins. In Tietz Textbook of Clinical Chemistry and Molecular Diagnostics, Burtis CA, Ashwood ER, Bruns DE (eds), pp 555–556. Elsevier Saunders: St Louis, MO
Junker N, Johansen JS, Andersen CB, Kristjansen PE (2005) Expression of YKL-40 by peritumoral macrophages in human small cell lung cancer. Lung Cancer 48: 223–231
Marott SC, Nordestgaard BG, Zacho J, Friberg J, Jensen GB, Tybjaerg-Hansen A, Benn M (2010) Does elevated C-reactive protein increase atrial fibrillation risk? A Mendelian randomization of 47,000 individuals from the general population. J Am Coll Cardiol 56: 789–795
Nielsen AR, Plomgaard P, Krabbe KS, Johansen JS, Pedersen BK (2011) IL-6, but not TNF-alpha, increases plasma YKL-40 in human subjects. Cytokine 55: 152–155
Nordenbaek C, Johansen JS, Junker P, Borregaard N, Sorensen O, Price PA (1999) YKL-40, a matrix protein of specific granules in neutrophils, is elevated in serum of patients with community-acquired pneumonia requiring hospitalization. J Infect Dis 180: 1722–1726
Nordestgaard BG (2009) Does elevated C-reactive protein cause human atherothrombosis? Novel insights from genetics, intervention trials, and elsewhere. Curr Opin Lipidol 20: 393–401
Nordestgaard BG, Benn M, Schnohr P, Tybjaerg-Hansen A (2007) Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA 298: 299–308
Ostergaard C, Johansen JS, Benfield T, Price PA, Lundgren JD (2002) YKL-40 is elevated in cerebrospinal fluid from patients with purulent meningitis. Clin Diagn Lab Immunol 9: 598–604
Otani T, Iwasaki M, Sasazuki S, Inoue M, Tsugane S (2006) Plasma C-reactive protein and risk of colorectal cancer in a nested case-control study: Japan Public Health Center-based prospective study. Cancer Epidemiol Biomarkers Prev 15: 690–695
Pepys MB, Hirschfield GM (2003) C-reactive protein: a critical update. J Clin Invest 111: 1805–1812
Recklies AD, White C, Ling H (2002) The chitinase 3-like protein human cartilage glycoprotein 39 (HC-gp39) stimulates proliferation of human connective-tissue cells and activates both extracellular signal-regulated kinase- and protein kinase B-mediated signalling pathways. Biochem J 365: 119–126
Schnohr P, Jensen JS, Scharling H, Nordestgaard BG (2002) Coronary heart disease risk factors ranked by importance for the individual and community. A 21 year follow-up of 12 000 men and women from The Copenhagen City Heart Study. Eur Heart J 23: 620–626
Siemes C, Visser LE, Coebergh JW, Splinter TA, Witteman JC, Uitterlinden AG, Hofman A, Pols HA, Stricker BH (2006) C-reactive protein levels, variation in the C-reactive protein gene, and cancer risk: the Rotterdam Study. J Clin Oncol 24: 5216–5222
Storm HH (1988) Completeness of cancer registration in Denmark 1943–1966 and efficacy of record linkage procedures. Int J Epidemiol 17: 44–49
Storm HH (1991) The Danish Cancer Registry, a self-reporting national cancer registration system with elements of active data collection. IARC Sci Publ 95: 220–236
Storm HH, Michelsen EV, Clemmensen IH, Pihl J (1997) The Danish Cancer Registry – history, content, quality and use. Dan Med Bull 44: 535–539
Trichopoulos D, Psaltopoulou T, Orfanos P, Trichopoulou A, Boffetta P (2006) Plasma C-reactive protein and risk of cancer: a prospective study from Greece. Cancer Epidemiol Biomarkers Prev 15: 381–384
Vos K, Steenbakkers P, Miltenburg AM, Bos E, van Den Heuvel MW, van Hogezand RA, de Vries RR, Breedveld FC, Boots AM (2000) Raised human cartilage glycoprotein-39 plasma levels in patients with rheumatoid arthritis and other inflammatory conditions. Ann Rheum Dis 59: 544–548
Zacho J, Tybjaerg-Hansen A, Nordestgaard BG (2010a) C-reactive protein and all-cause mortality – the Copenhagen City Heart Study. Eur Heart J 31: 1624–1632
Zacho J, Tybjaerg-Hansen A, Nordestgaard BG (2010b) C-reactive protein and risk of venous thromboembolism in the general population. Arterioscler Thromb Vasc Biol 30: 1672–1678
Acknowledgements
We are indebted to the staff and participants of the Copenhagen City Heart Study for their important contributions.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies the paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Allin, K., Bojesen, S., Johansen, J. et al. Cancer risk by combined levels of YKL-40 and C-reactive protein in the general population. Br J Cancer 106, 199–205 (2012). https://doi.org/10.1038/bjc.2011.501
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2011.501
Keywords
This article is cited by
-
A prospective follow-up study of the relationship between high-sensitivity C-reactive protein and primary liver cancer
BMC Cancer (2020)
-
Elevated pretreatment serum concentration of YKL-40: An independent prognostic biomarker for poor survival in patients with colorectal cancer
Medical Oncology (2014)