Abstract
Background:
We previously reported that the primary tumour/vessel tumour/nodal tumour (PVN) classification is significantly superior to the UICC pTNM classification and the Nottingham Prognostic Index for accurately predicting the outcome of patients with invasive ductal carcinoma of the breast in a manner that is independent of the nodal status and the hormone receptor status.
Methods:
The purpose of the present study was to compare the outcome predictive power of a modified PVN classification to that of the newly devised pathological UICC pTNM classification and the reclassified Nottingham Prognostic Index in a different group of patients with invasive ductal carcinoma (n=1042) using multivariate analyses by the Cox proportional hazard regression model.
Results:
The modified PVN classification clearly exhibited a superior significant power, compared with the other classifications, for the accurate prediction of tumour recurrence and tumour-related death among patients with invasive ductal carcinoma in a manner that was independent of the nodal status, the hormone receptor status, and adjuvant therapy status.
Conclusion:
The modified PVN classification is a useful classification system for predicting the outcome of invasive ductal carcinoma of the breast.
Similar content being viewed by others
Main
We previously reported that the primary tumour/vessel tumour/nodal tumour (PVN) classification is significantly superior to the UICC pTNM classification (Sobin and Wittekind, 2002), the Nottingham Prognostic Index (Todd et al, 1987; Sundquist et al, 1999), and the histologic grade (Elston and Ellis, 1991) for accurately predicting the outcome of patients with invasive ductal carcinoma of the breast in a manner that is independent of the nodal status and the hormone receptor status (Hasebe et al, 2005). Since then, we newly devised a histological prognostic system, namely a grading system for lymph vessel tumour emboli, and have clearly demonstrated that this grading system can accurately predict the outcome of patients with invasive ductal carcinoma in a manner that is independent of nodal metastasis (Hasebe et al, 2008, 2010). In addition, although we have already reported that the diameter of the fibrotic focus is an important histological factor for predicting the outcome of patients with invasive ductal carcinoma without nodal metastasis (Hasebe et al, 1998, 2002a), this parameter was also found to be an important outcome predictor for patients with invasive ductal carcinoma with nodal metastasis in a study with a different patient group (Hasebe et al, 2009). Although we have separately devised a PVN classification based on histological factors, for example, the diameter of the fibrotic focus, the number of apoptotic figures of lymph vessel tumour emboli, and the number of invaded lymph vessels, for accurately predicting the outcome of patients with invasive ductal carcinoma with or without nodal metastasis (Hasebe et al, 2005), the above-mentioned studies strongly suggested that the factors used in this classification can accurately predict the outcome of patients with invasive ductal carcinoma in a manner that is independent of the nodal status. Thus, we attempted to refine the PVN classification using well-known histological factors as well as the factors that we proposed by analysing the outcome predictive powers of these factors in a different invasive ductal carcinoma patient group.
The purpose of this study was to compare the outcome predictive power of the modified PVN classification with that of the newly devised pathological UICC pTNM classification (Sobin et al, 2009), and the reclassified Nottingham Prognostic Index (Blamey et al, 2007) in a different group of patients with invasive ductal carcinoma. The latter two classifications are the major histological prognostic classifications currently in use clinically to predict the outcome of patients with breast carcinoma. The results clearly indicated that the modified PVN classification is a useful histological classification available for predicting the outcome of invasive ductal carcinoma of the breast in a manner that is independent of the nodal status, the hormone receptor status, and the adjuvant therapy status.
Patients and methods
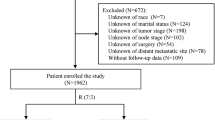
Patients
The subjects of this study were 1042 consecutive patients with invasive ductal carcinoma of the breast who did not receive neoadjuvant therapy and were selected among 1759 patients with breast cancer who were surgically treated at the National Cancer Center Hospital between January 2000 and December 2005 (almost the same case series as that used in our previous study)(Hasebe et al, 2010). The invasive ductal carcinomas were diagnosed preoperatively using a needle biopsy, aspiration cytology, a mammography, or ultrasonography. All the patients investigated in this study were Japanese women, ranging in age from 23 to 72 years old (median, 55 years). All had a solitary lesion; 498 patients were pre-menopausal and 544 were post-menopausal. A partial mastectomy had been performed in 458 patients, and a modified radical mastectomy had been performed in 584. A level I and level II axillary lymph node dissection had been performed in all the patients, and a level III axillary lymph node dissection had been performed in some of the invasive ductal carcinoma patients.
Of the 1042 patients, 873 received adjuvant therapy, consisting of chemotherapy in 217 patients, endocrine therapy in 281 patients, and chemoendocrine therapy in 375 patients. The chemotherapy regimens used were anthracycline-based with or without taxane and non-anthracycline-based, and the endocrine therapy regimens consisted of tamoxifen with or without a gonadotropin-releasing hormone agonist, tamoxifen, with or without an aromatase inhibitor, an aromatase inhibitor alone, or a gonadotropin-releasing hormone agonist alone. No cases of inflammatory breast cancer were included in this series. All the tumours were classified according to the pathological UICC TNM classification (Sobin et al, 2009). The protocol for this study (20–112) was reviewed by the institutional review board of the National Cancer Center.
For the pathological examination, the surgically resected specimens were fixed in 10% formalin, and the size and gross appearance of the tumours were recorded. The tumour size was confirmed by comparison with the tumour size on the histological slides.
Improvement of the PVN classification
We previously reported that a grading system for lymph vessel tumour emboli is a very useful histological classification in the accurate prediction of the outcome of patients with invasive ductal carcinoma independent of nodal status using multivariate analyses with well-known clinicopathological factors (Hasebe et al, 2008, 2010). Furthermore, the diameter of the fibrotic focus has also been reported to be a useful histological predictor of outcome for invasive ductal carcinoma patients with or without nodal metastasis using multivariate analyses with well-known clinicopathological factors (Hasebe et al, 2009). Thus, based on these findings, we attempted to improve our original PVN classification (Hasebe et al, 2005) by performing multivariate analyses using the Cox proportional hazard regression model to analyse the effects of well-known histological factors, our proposed histological factors, age (⩽39 vs >39 years), the Allred scores for oestrogen receptor and progesterone receptor and the category of HER2 expression in the tumour cells, and the type of adjuvant therapy (no adjuvant therapy, endocrine therapy, chemoendocrine therapy, and chemotherapy). Factors that were significantly associated with outcome in univariate analyses were entered together into a multivariate analysis performed using the Cox proportional hazard regression model. The case-wise, step-down, and two-sided method was applied until all the remaining factors were significant at a P-value of <0.05. All analyses were performed using Statistica/Windows software (StatSoft, Tulsa, OK, USA).
The following 12 histological factors of the primary invasive ductal carcinomas were evaluated: (1) invasive tumour size (⩽20 mm, >20 to ⩽50 mm, and >50 mm), (2) tubule formation (well degree, moderate degree, and poor degree) (Elston and Ellis, 1991, 3) number of mitotic figures in the primary invasive ductal carcinoma (⩽9, >9 to ⩽19, and >20) (Elston and Ellis, 1991, 4) nuclear features (small and regular, moderate variation, and marked variation) (Elston and Ellis, 1991, 5) tumour necrosis (absent and present)(Gilchrist et al, 1993, 6) blood vessel invasion (absent and present), (7) adipose tissue invasion (absent and present), (8) skin invasion (absent and present), (9) muscle invasion (absent and present), (10) fibrotic focus (absent, fibrotic focus diameter ⩽8 mm, and fibrotic focus diameter >8 mm)(Hasebe et al, 1998, 2002a, 11) grading system for lymph vessel tumour emboli (grades 0, 1, 2, and 3) (Hasebe et al, 2008, 2010), and (12) number of apoptotic figures in blood vessel tumour emboli (blood vessel invasion absent, ⩽2, and >2) (Hasebe et al, 2003a).
The nodal metastases were evaluated using single sections of each node or half of each node stained with hematoxylin and eosin. The following 10 histological parameters of metastatic mammary carcinoma to the lymph nodes were evaluated: (1) number of nodal metastases (no nodal metastasis, 1–3, 4–9, 10, or more), (2) maximum dimension (no nodal metastasis, ⩽20 mm, and >20 mm), (3) tubule formation (no nodal metastasis, well degree, moderate degree, and poor degree), (4) nuclear features (no nodal metastasis, small and regular, moderate variation, and marked variation), (5) number of mitotic figures (no nodal metastasis, ⩽5, and >5)(Hasebe et al, 2003b, 2004, 2011, 6) fibrotic focus (no nodal metastasis, absent, and present), (7) tumour necrosis (no nodal metastasis, absent, and present), (8) grade of stromal fibrosis (no nodal metastasis, none, mild, moderate, and severe) (Hasebe et al, 2003b, 2004, 2011, 9) number of lymph nodes with extranodal invasion (no nodal metastasis, ⩽5, and >5) (Hasebe et al, 2003b, 2004, 2011), and (10) number of extranodal blood vessel tumour emboli (no nodal metastasis, <2, and >2) (Hasebe et al, 2003b, 2004, 2011). We randomly searched for mitotic figures in metastatic mammary carcinoma to the lymph nodes using mid-power magnification fields ( × 10 or × 20) of the tumour area and selected one high-power magnification field ( × 40) of the tumour area with the highest number of mitotic figures in metastatic mammary carcinoma to the lymph nodes to determine the largest number of metastatic mammary carcinoma to the lymph nodes exhibiting mitotic figures (Figure 1). The tubule formation, nuclear features, and presence of tumour necrosis in metastatic mammary carcinoma to the lymph nodes were evaluated in the same manner as for the primary invasive ductal carcinomas.
Histological factors of the modified PVN classification (A–G). (A) Invasive ductal carcinomas with a fibrotic focus. A fibrotic focus measuring 13.4 × 6.8 mm is visible within the tumour (panoramic view, arrows). The fibrotic focus shows a scar-like feature and is surrounded by invasive ductal carcinoma cells. (B) Invasive ductal carcinoma cells showing marked variations in nuclear features; mitotic figures are also visible in the tumour cells. (C) Several apoptotic bodies and apoptotic tumour cells are visible (arrows), and three mitotic tumour cells (arrowheads) are visible in the tumour embolus in the lymph vessel. (D) One blood vessel tumour embolus is seen adjacent to one artery. Seven apoptotic bodies or apoptotic tumour cells are seen in the blood vessel tumour embolus, and red blood cells are also visible. (E) Lymph node metastases exhibited a severe grade of tumour stroma. (F) Five extranodal blood vessel tumour emboli are seen in metastatic carcinoma to the lymph node (arrows). (G) Six mitotic tumour cells are visible in the tumour of the lymph node (arrows).
Prognostic histological classifications for comparative study
The following existing histological classifications were compared with our modified classification with regard to the prediction of disease-free survival and overall survival: (1) the UICC pTNM classification (Sobin et al, 2009) and (2) the Nottingham Prognostic Index (Blamey et al, 2007).
The Nottingham Prognostic Index (Blamey et al, 2007) is based on the tumour size, histologic grade (Elston and Ellis, 1991), and nodal classification of the UICC pTNM classification (Sobin et al, 2009). Thus, multivariate analyses for tumour recurrence and tumour-related death were performed using the following models to avoid the mutual influences of each classification: (1) model 1, the modified PVN classification and the UICC pTNM classification; and (2) model 2, the modified PVN classification and the Nottingham Prognostic Index.
The predictive powers for the disease-free and overall survivals of each classification, age (⩽39 vs >39 years), the Allred scores for oestrogen receptor and progesterone receptor and the category of HER2 expression in the tumour cells, and the type of adjuvant therapy (no adjuvant therapy, endocrine therapy, chemoendocrine therapy, and chemotherapy) were evaluated using univariate analyses with the Cox proportional hazard regression model according to nodal status, hormone receptor status, and adjuvant therapy status. The classifications and factors that were significantly associated with outcome in the univariate analyses were then entered together into the multivariate analyses that were performed using the Cox proportional hazard regression model. The case-wise, step-down and two-sided method was applied until all the remaining factors were significant at a P-value of <0.05. The survival curves were drawn using the Kaplan–Meier method. All the analyses were performed with Statistica/Windows software (StatSoft).
Assessment of oestrogen receptor, progesterone receptor, and HER2 expression
Slides of the tumour cells immunostained for oestrogen receptor or progesterone receptor were scored using the Allred scoring system, as described previously (Harvey et al, 1999; Mohsin et al, 2004), and the Allred scores for oestrogen receptor and progesterone receptor in the tumour cells were classified into the following three categories (Hasebe et al, 2009): (1) Allred score for oestrogen receptor in tumour cells (0 or 2, 3–6, and 7 or 8); and (2) Allred score for progesterone receptor in tumour cells (0 or 2, 3–6, and 7 or 8). The HER2 status of the tumour cells was semiquantitatively scored on a scale of 0–3 according to the level of HER2 protein expression (Wolff et al, 2007) and was classified into three categories: 0 or 1, 2, and 3.
Patient outcome
Survival was evaluated using a median follow-up period of 98 months (range: 63–134 months) until March 2011. Of the 1042 invasive ductal carcinoma patients, 858 patients were alive and well, 184 had developed tumour recurrences (distant-organ metastasis and local recurrence), and 89 had died of their disease. The tumour recurrence-free survival and overall survival periods were calculated using the time of surgery as the starting point. Tumour relapse was considered to have occurred whenever evidence of distant-organ metastasis or local recurrence was found.
Results
Histological factors significantly associated with the outcome of patients with invasive ductal carcinoma
Among all the patients with invasive ductal carcinoma, a fibrotic focus diameter >8 mm, lymph vessel tumour embolus grades 2 and 3, lymph node metastases with a dimension of >20 mm, >2 apoptotic figures in blood vessel tumour emboli, and >5 mitotic figures in metastatic carcinoma to the lymph nodes had significantly higher hazard ratios for tumour recurrence and tumour-related death in multivariate analyses (Table 1). Marked variation in the nuclear features of the primary invasive ductal carcinoma had a significantly higher hazard ratio for tumour recurrence, and >2 extranodal blood vessel tumour emboli had a significantly higher hazard ratio for tumour-related death in multivariate analyses (Table 1). An Allred score of 7 or 8 for progesterone receptor in the tumour cells had a significantly lower hazard ratio for tumour-related death in multivariate analysis (Table 1).
Among patients with invasive ductal carcinoma without nodal metastasis, lymph vessel tumour grade 3 and >19 mitotic figures in primary invasive ductal carcinomas had a significantly higher hazard ratio for tumour recurrence and tumour-related death in multivariate analyses (Table 2). Lymph vessel tumour grade 2, a fibrotic focus >8 mm, and HER2 category 3 had significantly higher hazard ratios for tumour recurrence, and >2 apoptotic figures in blood vessel tumour emboli had a significantly higher hazard ratio for tumour-related death in multivariate analyses.
Among patients with invasive ductal carcinoma with nodal metastases, a fibrotic focus diameter >8 mm, lymph vessel tumour embolus grades 2 and 3, lymph node metastases with a dimension of >20 mm, >2 apoptotic figures in blood vessel tumour emboli, >2 extranodal blood vessel tumour emboli, and >5 mitotic figures in metastatic carcinoma to the lymph nodes had significantly higher hazard ratios for tumour recurrence and tumour-related death in multivariate analyses (Table 3). A severe grade of stromal fibrosis in metastatic carcinoma to the lymph nodes had a significantly higher ratio for tumour recurrence, and an Allred score of 7 or 8 for progesterone receptors had a significantly lower hazard ratio for tumour-related death in a multivariate analysis (Table 3).
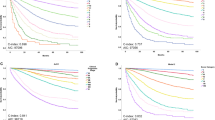
Modified PVN classification
We refined our previously proposed PVN classification (Hasebe et al, 2005) based on the above results of the present study, and the nine parameters that were selected for modified PVN classification are listed in Table 4 (Figure 1). Four factors (mitotic figures in primary invasive ductal carcinoma, lymph vessel tumour grade, grade of stromal fibrosis in metastatic carcinoma to the lymph nodes, and maximum dimension of metastatic carcinoma to the lymph nodes) were newly added to the classification based on the results of this study. In the modified PVN classification, a score of 1 point was given for each unfavourable parameter. A grading system of 0–3 was used to score the lymph vessel tumour emboli (Hasebe et al, 2008, 2010) (Figure 1D). The total score was then calculated (0–11). The resulting scores were divided into the following six classes according to their significant associations with tumour recurrence or tumour-related death in univariate analyses using the logrank test: (1) class 0 (score 0), (2) class 1 (scores 1 and 2), (3) class 2 (scores 3 and 4), (4) class 3 (score 5), (5) class 4 (scores 6 and 7), and (6) class 5 (score of 8 or more) (Table 5, Figure 2).
Disease-free survival curve and overall survival curve according to the modified PVN classification for all the patients in the present study (A and B). The disease-free survival curve (A) and the overall survival curve (B) for each class significantly decrease according to the increasing order of the classifications (P<0.001).
Furthermore, we also attempted to modify the PVN classification using the weight given to each factor based on its median hazard ratio obtained using the multivariate analyses in this study. The weights that were given for each factor were as follows: (1) 2.0 for a fibrotic focus diameter >8 mm, (2) 1.5 for the marked variation of nuclear features of primary invasive ductal carcinoma, (3) 7.2 for >19 mitotic figures in primary invasive ductal carcinoma, (4) 2.9 for lymph vessel tumour embolus grade 2 and 4.2 for lymph vessel tumour embolus grade 3, (5) 3.2 for >2 apoptotic figures in blood vessel tumour emboli, (6) 1.9 for a severe grade of stromal fibrosis in metastatic carcinoma to the lymph nodes, (7) 1.9 for lymph node metastases with a dimension of >20, (8) 1.9 for >2 extranodal blood vessel tumour emboli, and (9) 3.1 for >5 mitotic figures in metastatic carcinoma to the lymph nodes. The total factor weights for individual patients were calculated (minimum, 0; maximum, 27.3; median, 1.5) and we classified all the patients into the following five classes based on the total factor weight for each patient: (1) 484 patients with a total factor weight of 0, class 0; (2) 192 with a total factor weight of >0 to ⩽5, class 1; (3) 321 with a total factor weight of >5 to ⩽10, class 2; (4) 31 with a total factor weight of >10 to ⩽18, class 3; and (5) 14 with a total factor weight of >18, class 4.
Next, we performed multivariate analyses for tumour recurrence and tumour-related death between the score-modified PVN and the weight-modified PVN classification as a whole. Although both classifications significantly increased the hazard ratios for tumour recurrence and tumour-related death, the score-modified PVN classification (tumour recurrence: trend hazard ratio, 2.1, P<0.001; tumour-related death: trend hazard ratio, 2.2, P<0.001) had higher trend hazard ratios and lower trend P-values for tumour recurrence and tumour-related death than the weight-modified PVN classification (tumour recurrence: trend hazard ratio, 1.3, P=0.019; tumour-related death: trend hazard ratio, 1.5, P=0.033). Therefore, we adopted the former classification for a comparison with the other two classifications in this study.
Tumour recurrence and death rates according to each classification
According to the modified PVN classification, the rates of tumour recurrence or death from invasive ductal carcinoma increased as the order of the classes increased; the rates of classes 4 and 5, in particular, were higher than those of the high-risk groups of the other classifications (Table 5). Significantly shorter crude disease-free survival and overall survival periods were observed according to the increasing order of classes, with the exception of both survival periods for classes 3 and 4 and the overall survival periods for classes 4 and 5 (Table 5, Figure 2).
Among the other classifications, the UICC pTNM stage classification showed significantly shorter crude disease-free survival and overall survival periods according to the increasing order of stages (Table 5). Among the three classifications, the Nottingham Prognostic Index clearly exhibited the lowest tumour recurrence rate in patients with a good prognosis (excellent prognostic group). The Nottingham Prognostic Index showed a significantly shorter crude disease-free survival period according to the increasing order of groups with the exception of moderate prognostic group II, but significant differences in the overall survival periods were seen between the moderate prognostic group II and the poor prognostic group, and between the poor prognostic group and the very poor prognostic group out of the six groups (Table 5).
Comparison of the classifications
In model 1 multivariate analyses of all the patients, the modified PVN classification significantly increased the trend hazard ratios for tumour recurrence (P<0.001) and tumour-related death (P<0.001). Although the UICC pTNM classification showed a significant association with tumour recurrence (P=0.018), it failed to show a significant association with tumour-related death (P=0.165). HER2 category 3 had a significant association with tumour recurrence (P=0.033). In model 2 multivariate analyses, the modified PVN classification significantly increased the trend hazard ratios for tumour recurrence (P<0.001) and tumour-related death (P<0.001). The Nottingham Prognostic Index also showed significant associations with tumour recurrence (P=0.003) and tumour-related death (P=0.006). HER2 category 3 failed to significantly increase the hazard ratio for tumour recurrence in model 2 multivariate analyses.
In patients with invasive ductal carcinoma without nodal metastasis, the UICC pTNM classification failed to show a significant association with tumour recurrence or tumour-related death in univariate analyses (data not shown). In model 1 multivariate analyses, the modified PVN classification was significantly associated with tumour recurrence (P<0.001) and tumour-related death (P<0.001). In model 2 multivariate analyses, the modified PVN classification was significantly associated with tumour recurrence and tumour-related death, but the Nottingham Prognostic Index was not significantly associated with tumour recurrence or tumour-related death (Table 6).
In patients with invasive ductal carcinoma with nodal metastasis, the modified PVN classification showed significant associations with tumour recurrence and tumour-related death but the UICC pTNM classification did not show a significant association with tumour recurrence or tumour-related death in model 1 multivariate analyses (Table 6). In model 2 multivariate analyses, the modified PVN classification also showed significant associations with tumour recurrence and tumour-related death. The Nottingham Prognostic Index did not show a significant association with tumour recurrence, but a significant association with tumour-related death was observed (Table 6).
In patients with invasive ductal carcinoma who were completely negative for hormone receptors, only the modified PVN classification showed significantly increasing trend hazard ratios for tumour recurrence and tumour-related death in the multivariate analyses (Table 6).
In model 1 and 2 multivariate analyses of patients with invasive ductal carcinoma who were positive for one or two hormone receptors, the modified PVN classification exhibited significantly increasing trend hazard ratios for tumour recurrence and tumour-related death (Table 6). The Nottingham Prognostic Index also showed significantly increasing trend hazard ratios for tumour recurrence and tumour-related death (Table 6). Although the UICC pTNM classification significantly increased the trend hazard ratio for tumour recurrence, it failed to significantly increase the trend hazard ratio for tumour-related death (Table 6). In model 1 and 2 multivariate analyses, the adjuvant therapy status significantly increased the trend hazard ratios for tumour-related death (model 1, P=0.007; model 2, P=0.022) but failed to significantly increase the trend hazard ratios for tumour recurrence (model 1, P=0.996; model 2, P=0.597).
In model 1 and 2 multivariate analyses of patients with invasive ductal carcinoma not treated with adjuvant therapy, the modified PVN classification significantly increased the hazard ratios for tumour recurrence (Table 7). The UICC pTNM classification and the Nottingham Prognostic Index failed to show significant associations with tumour recurrence (Table 7). HER2 category 3 significantly increased the trend hazard ratio for tumour recurrence in a model 1 multivariate analysis (P=0.048) but failed to significantly increase the trend hazard ratio for tumour recurrence in a model 2 multivariate analysis (P=0.093). As only five patients died as a result of their disease in this series, a multivariate analysis for tumour-related death could not be performed.
In model 1 and 2 multivariate analyses of patients with invasive ductal carcinoma treated with endocrine therapy, the modified PVN classification significantly increased the trend hazard ratios for tumour recurrence and tumour-related death (Table 7). The UICC pTNM classification and the Nottingham Prognostic Index failed to show significant associations with tumour recurrence and tumour-related death (Table 7). In model 1 and 2 multivariate analyses, HER2 category 3 significantly increased the trend hazard ratios for tumour-related death (model 1 and model 2, P<0.001) but failed to significantly increase the trend hazard ratios for tumour recurrence (model 1, P=0.082; model 2, P=0.086).
In model 1 and 2 multivariate analyses of patients with invasive ductal carcinoma treated with chemoendocrine therapy, the modified PVN classification significantly increased the hazard ratios for tumour recurrence and tumour-related death (Table 7). The UICC pTNM classification did not show significantly increasing trend hazard ratios for tumour recurrence and tumour-related death (Table 7). The Nottingham Prognostic Index significantly increased the trend hazard ratios for tumour recurrence and tumour-related death (Table 7).
In model 1 and 2 multivariate analyses of patients with invasive ductal carcinoma treated with chemotherapy, although the modified PVN classification significantly increased the trend hazard ratios for tumour recurrence and tumour-related death, the UICC pTNM classification and the Nottingham Prognostic Index failed to show significant associations with tumour recurrence or tumour-related death (Table 7).
Discussion
We previously reported that the PVN classification can accurately predict the outcome of patients with invasive ductal carcinoma in a manner that is independent of the nodal status or hormone receptor status (Hasebe et al, 2005), and the present study also clearly demonstrated that the modified PVN classification accurately predicted the outcome of patients with invasive ductal carcinoma in a manner that was independent of the nodal status, hormone receptor status, or adjuvant therapy status in a different group of patients with invasive ductal carcinoma. The clinical value of prognostic factors is particularly useful for the selection of different treatment regimens, especially adjuvant therapy in patients with invasive ductal carcinoma. One could argue that identifying patients with invasive ductal carcinoma who have a good prognosis and who do not require adjuvant therapy is of particular importance. The modified PVN classification was capable of classifying 815 (78%) out of 1042 patients as class 0 or 1, and patients belonging to these classes may be considered as good and moderately good prognostic groups, respectively. In contrast, patients belonging to class 2 or higher classes of the modified PVN classification may be considered as belonging to poor or very poor prognostic groups, respectively. In addition, the modified PVN classification had a superior outcome predictive power for the other two classifications in a manner that was independent of the adjuvant therapy status. Thus, the results of this study suggest that patients belonging to class 0 or 1 of the modified PVN classification can be spared adjuvant therapy, while patients belonging to class 2 or higher classes of the classification should be treated with adjuvant therapy in a manner that is independent of the nodal status or the hormone receptor status.
The factors included in the modified PVN classification were selected based on the precise analyses of this study using well-known clinicopathological factors, such as histologic grade, invasive tumour size, and nodal status. Among the nine factors in the modified PVN classification, seven of them were the histological factors that we proposed for primary invasive ductal carcinoma, carcinomas in vessels, and metastatic carcinoma to the lymph nodes (Hasebe et al, 1998, 2002a, 2003a, 2003b, 2004, 2008, 2010, 2011). This study clearly confirmed that these histological factors are important outcome predictors for different patient series of invasive ductal carcinoma of the breast. Among them, the outcome predictive power of the fibrotic focus among patients with invasive ductal carcinoma has also been confirmed by other investigators (Colpaert et al, 2001; Baak et al, 2005). Thus, these parameters are likely to be the most suitable parameters for accurately assessing the true biological malignant potential of invasive ductal carcinomas. In addition, we also confirmed the prognostic significance of the following factors that were previously reported by other investigators (Elston and Ellis, 1991) to be useful histological factors for predicting the outcome of patients with invasive ductal carcinomas: (1) the nuclear features of primary invasive ductal carcinoma and (2) the number of mitotic figures in primary invasive ductal carcinoma. Thus, the modified PVN classification appears to be better at accurately predicting the outcome of patients with invasive ductal carcinoma, compared with the other two classifications.
This study also strongly suggests that the tumour characteristics of invasive ductal carcinomas matter more than the quantity of tumour with regard to the accurate prediction of the outcome of patients with invasive ductal carcinoma. Both the UICC pTNM stage classification and the Nottingham Prognostic Index evaluate the malignant potential of invasive ductal carcinomas based on the invasive tumour size and the number of nodal metastases. These factors reflect the quantity of invasive ductal carcinoma cells. In contrast, almost all the factors in the modified PVN classification, exception of the maximum diameter of lymph node metastases, represent the tumour characteristics of invasive ductal carcinomas. In addition, we previously showed that mitotic figures and apoptotic figures in tumour cells of lymph vessel tumour emboli have significantly stronger outcome predictive powers than the number of lymph vessels that have been invaded (Hasebe et al, 2002b), and we devised a grading system for lymph vessel tumour emboli based on the presence of mitotic figures and apoptotic figures in the tumour cells of lymph vessel tumour emboli (Hasebe et al, 2008, 2010). As the modified PVN classification can evaluate the tumour characteristics of the invasive ductal carcinoma more precisely than the other two classifications, it appears to have a superior ability for accurately predicting patient outcome. Therefore, we concluded that the modified PVN classification is a useful prognostic histological classification available for predicting the outcome of patients with invasive ductal carcinoma of the breast.
We used the modified PVN classification for patients with invasive ductal carcinoma because our previous studies clearly demonstrated that the factors included in this classification were significant outcome predictors only for patients with invasive ductal carcinoma (Hasebe et al, 1998, 2002a, 2003a, 2003b, 2004, 2008, 2010, 2011). The UICC pTNM classification and the Nottingham Prognostic Index can be applied to all invasive breast carcinomas and may be superior to the modified PVN classification for predicting the outcome of overall patients with invasive carcinoma. Thus, we should confirm whether the modified PVN classification is also able to accurately predict the outcome of patients with non-ductal carcinomas of the breast in the future.
In conclusion, the current study clearly confirmed that the modified PVN classification is a useful histological classification for predicting the outcome of patients with invasive ductal carcinoma of the breast. Thus, pathologists should attempt to assess the true malignant potential of invasive ductal carcinomas using the criteria of the modified PVN classification.
Change history
29 March 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Baak JP, Colpaert CG, van Diest PJ, Janssen E, van Diermen B, Albernaz E, Vermeulen PB, Van Marck EA (2005) Multivariate prognostic evaluation of the mitotic activity index and fibrotic focus in node-negative invasive breast cancers. Eur J Cancer 41: 2093–2101
Blamey RW, Ellis IO, Pinder SE, Lee AHS, Macmillan RD, Morgan DAL, Robertson JFR, Mitchell MJ, Ball GR, Haybittle JL, Elston CW (2007) Survival of invasive breast cancer according to the Nottingham Prognostic Index in cases diagnosed in 1990–1999. Eur J Cancer 43: 1548–1555
Colpaert C, Vermeulen PB, van Beest P, Goovaerts G, Weyler J, Van Dam P, Dirix L, Van Marck E (2001) Intratumoral hypoxia resulting in the presence of a fibrotic focus is an independent predictor of early distant relapse in lymph node-negative breast cancer patients. Histopathology 39: 416–425
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19: 403–4l0
Gilchrist KW, Gray R, Fowble B, Fowble B, Tormey DC, Taylor SG (1993) Tumor necrosis is a prognostic predictor for early recurrence and death in lymph node-positive breast cancer: a 10-year follow-up study of 728 eastern cooperative oncology group patients. J Clin Oncol 11: 1929–1935
Harvey JM, Clark GM, Osborne K, Allred DC (1999) Estrogen receptor status by immunohistochemistry is superior to the ligand-binding assay for predicting response to adjuvant endocrine therapy in breast cancer. J Clin Oncol 17: 1474–1481
Hasebe T, Iwasaki M, Akashi-Tanaka S, Hojo T, Shibata T, Sasajima Y, Tsuda H, Kinoshita T (2011) Prognostic significance of mitotic figures in metastatic mammary ductal carcinoma to the lymph nodes. Hum Pathol; e-pub ahead of print 17 June 2011
Hasebe T, Okada N, Iwasaki M, Akashi-Tanaka S, Hojo T, Shibata T, Sasajima Y, Tsuda H, Kinoshita T (2010) Grading system for lymph vessel tumor emboli: significant outcome predictor for invasive ductal carcinoma of the breast. Hum Pathol 41: 706–715
Hasebe T, Sasaki S, Imoto S, Mukai K, Yokose T, Ochiai A (2002a) Prognostic significance of fibrotic focus in invasive ductal carcinoma of the breast: a prospective observational study. Mod Pathol 15: 502–516
Hasebe T, Sasaki S, Imoto S, Ochiai A (2003a) Histological characteristics of tumors in blood vessels play an important role in tumor progression of invasive ductal carcinoma of the breast. Cancer Sci 94: 158–165
Hasebe T, Sasaki S, Imoto S, Ochiai A (2003b) Significance of nodal metastatic tumor characteristics in nodal metastasis and prognosis of patients with invasive ductal carcinoma of the breast. Cancer Sci 94: 181–187
Hasebe T, Sasaki S, Imoto S, Ochiai A (2004) Histological characteristics of tumors in vessels and lymph nodes are significant parameter for predicting tumor progression of invasive ductal carcinoma of the breast: a prospective study. Hum Pathol 35: 298–308
Hasebe T, Sasaki S, Imoto S, Ochiai A (2002b) Characteristics of tumors in lymph vessels play an important role in the tumor progression of invasive ductal carcinoma of the breast: a prospective study. Mod Pathol 15: 904–913
Hasebe T, Sasaki S, Imoto S, Wada N, Ochiai A (2005) Primary tumor-vessel tumor-nodal tumor classification for patients with invasive ductal carcinoma of the breast. Br J Cancer 92: 847–856
Hasebe T, Tsuda H, Hirohashi S, Shimosato Y, Tsubono Y, Yamamoto H, Mukai K (1998) Fibrotic focus in infiltrating ductal carcinoma of the breast: a significant histopathological prognostic parameter for predicting the long-term survival of the patients. Breast Cancer Res Treat 49: 195–208
Hasebe T, Yamauchi C, Iwasaki M, Ishii G, Wada N, Imoto S (2008) Grading system for lymph vessel tumor emboli for prediction of the outcome of invasive ductal carcinoma of the breast. Hum Pathol 39: 427–436
Hasebe T, Okada N, Tamura N, Houjoh T, Akashi-Tanaka S, Tsuda H, Shibata T, Sasajima Y, Iwasaki M, Kinoshita T (2009) p53 expression in tumor stromal fibroblasts is associated with the outcome of patients with invasive ductal carcinoma of the breast. Cancer Sci 100: 2101–2108
Mohsin S, Weiss H, Havighurst T, Clark GM, Berardo M, Roanh le D, To TV, Qian Z, Love RR, Allred DC (2004) Progesterone receptor by immunohistochemistry and clinical outcome in breast cancer: a validation study. Mod Pathol 17: 1545–1554
Sobin LH, Gospodarowicz MK, Wittekind Ch (eds). (2009) International Union Against Cancer TNM Classification of Malignant Tumours, 7th edn, pp 181–193. Wiley-Liss: Geneva
Sobin LH, Wittekind Ch (eds). (2002) International Union Against Cancer TNM Classification of Malignant Tumors, 6th edn, pp 131–141. Wiley-Liss: Geneva
Sundquist M, Thorstenson S, Brudin L, Nordenskjold B (1999) Applying the Nottingham Prognostic Index to a Swedish breast cancer population. Breast Cancer Res Treat 53: 1–8
Todd JH, Dowle C, Williams MR, Elston CW, Ellis O, Hinton CP, Blamey RW, Haybittle JL (1987) Confirmation of a prognostic index in primary breast cancer. Br J Cancer 56: 489–492
Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, Dowsett M, Fitzgibbons PL, Hanna WM, Langer A, McShane LM, Paik S, Pegram MD, Perez EA, Press MF, Rhodes A, Sturgeon C, Taube SE, Tubbs R, Vance GH, van de Vijver M, Wheeler TM, Hayes DF, American Society of Clinical Oncolgy/College of American Pathologists (2007) American Scociety of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. Arch Pathol Lab Med 131: 18–43
Acknowledgements
This study was supported in part by a Grant-in-Aid for Scientific Research (KAKENHI) (C) (21590393) from the Japan Society for the Promotion of Science and was supported in part by a Grant-in-Aid for Cancer Research from the Ministry of Health, Labor and Welfare of Japan (H21-006).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Hasebe, T., Iwasaki, M., Akashi-Tanaka, S. et al. Modified primary tumour/vessel tumour/nodal tumour classification for patients with invasive ductal carcinoma of the breast. Br J Cancer 105, 698–708 (2011). https://doi.org/10.1038/bjc.2011.279
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2011.279